Lyme Disease Case Report Form
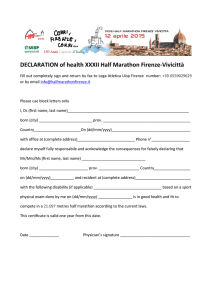
advertisement

LYME DISEASE CASE REPORT FORM DHA: ANDS Case ID: Classification: Confirmed Probable Date Investigation Opened Does not meet (yyyy/mm/dd): / / CASE DEMOGRAPHICS Last Name: DOB First Name: (yyyy/mm/dd): / Age: / Middle Name: Sex: Male Female HCN: Phone Number: Street Address: City: Transgender Postal Code: MEDICAL HISTORY Date of Onset (yyyy/mm/dd): / Re-infection: Physician’s Name: Yes / No Unknown No Date of initial diagnosis / Hospitalized: Yes (yyyy/mm/dd): / Location: If yes, Duration: Erythema Migrans : 1 Erythema Migrans (EM)1: Yes No Unknown EM diagnosed by a health care provider: Yes No Unknown Date EM diagnosed: Central Clearing: No (yyyy/mm/dd): / Yes / Unknown EM - Date of Onset / (yyyy/mm/dd): / Site(s) Specify: Lesion: Size (diameter): cm Other Symptoms: Other skin rashes: Yes Influenza-Like Illness: Yes No No Unknown Date of Onset / Unknown If yes, description: (yyyy/mm/dd): Late Manifestation(s) – see sections below Yes / No Unknown If no, continue with the ‘Exposure Information’ section. Notes: Musculoskeletal System: Yes No Unknown (If yes, please specify below) Description: Yes No Unk Date of Onset (yyyy/mm/dd) Recurrent, brief attacks (lasting weeks or months) of large joint swelling. Number of Joints involved: / / Other (specify): / / Notes: Document1 1 Cardiovascular System: Yes No Unknown (If yes, please specify below) Description: Yes No Unk Date of Onset (yyyy/mm/dd) AV Heart Block / / Myocarditis / / Other (specify) / / Notes: Nervous System: Yes No Unknown (If yes, please specify below) Description: Yes No Unk Date of Onset (yyyy/mm/dd) Peripheral Nervous System: Mononeuropathy – cranial or peripheral nerve (e.g. Bell’s Palsy), pain, numbness, tingling or weakness in distribution of single peripheral nerve / / Mononeuropathy multiplex – pain, numbness, tingling or weakness in distribution of a few or several peripheral nerves / / Peripheral polyneuropathy – pain, numbness, tingling or weakness in a symmetrical, diffuse fashion not corresponding to the distribution of specific peripheral nerves / / Lymphocytic Meningitis / / Encephalopathy / / Encephalomyelitis / / Other (specify) / / Central Nervous System: Notes: EXPOSURE INFORMATION History of tick exposure (bite): Definite Possible (exposed to wood or brushy areas) No Geographic location of tick exposure – please specify as much as possible: Unknown Date of Tick Exposure (yyyy/mm/dd) / / If exposure outside of Nova Scotia or Canada, please specify as much as possible: History of residence in, or visit to, an endemic2 area? Yes No Unknown - If yes, specify: Received a donation of blood, blood products, tissue/organs? Yes No Document1 Donated blood, blood products, tissue/organs? Yes No 2 TREATMENT Did case receive treatment? Yes No If yes, start date (yyyy/mm/dd): If yes, antibiotic: / / Dose: Duration of treatment: Have symptoms resolved? Yes No Notes: LABORATORY EVIDENCE3 Was laboratory testing ordered? Yes Test No If yes, specify in table below: Result Collection Date Lab Report Date (yyyy/mm/dd) (yyyy/mm/dd) EIA / / / / lgM WB / / / / lgG WB / / / / Other / / / / Was client referred to infectious disease? Follow-up completed with: Client Yes No Parent/Guardian Unknown Physician Other MOH/PHN Comments: CASE DEFINITION ASSESSMENT 1. Clinical Illness: Yes No 2. Clinician-observed EM: Yes No 3. Positive serologic test using two-tier ELISA and Western blot criteria: 4. History of residence in, or visit to an endemic area? Confirmed Case: i. ii. 1+3+4 OR 2+3+4 Document1 Probable 1 Case: i. ii. 1+3 OR 2+3 Yes Yes No No Probable 2 Case: 2+4 3 STATUS OF INVESTIGATION Open – pending further information Closed – incomplete Reason: Lost to follow-up Deceased Transferred Other (specify: Closed – completed Not a case (please comment): Date investigation closed (yyyy/mm/dd): / / LYME DISEASE CASE DEFINITION: Confirmed case: Clinical evidence of illness with laboratory conformation: Isolation of Borrelia burgdorferi from an appropriate clinical specimen, OR Detection of B. burgdorferi DNA by PCR OR Clinical evidence of illness with a history of residence in, or visit to, an endemic2 area and with laboratory evidence of infection: i.e. Positive serologic test using the two-tier ELISA and Western Blot criteria Probable case: Clinical evidence of illness without a history of residence in, or visit to, an endemic2 area and with laboratory evidence of infection: i.e. Positive serologic test using the two-tier ELISA and Western Blot criteria OR Clinician-observed EM1 without laboratory evidence but with history of residence in, or visit to, an endemic2 area. NOTES: 1. Erythema migrans (EM) A round or oval expanding erythematous area of the skin greater than 5 cm in diameter and enlarging slowly over a period of several days to weeks. It appears 1-2 weeks (range 3-30 days) after infection & persists for up to 8 weeks. Some lesions are homogeneously erythematous, whereas others have prominent central clearing or a distinctive target-like appearance. On the lower extremities, the lesion may be partially purpuric. Signs of acute or chronic inflammation are not prominent. There is usually little pain, itching, swelling, scaling, exudation or crusting, erosion or ulceration, except that some inflammation may be associated with the tick bite itself, which may be present at the very centre of the lesion. Note: an erythematous skin lesion present while a tick vector is still attached or that has developed within 48 hours of a tick bite is most likely a tick bite hypersensitivity reaction (i.e. a non-infectious process), rather than EM. Tick bite hypersensitivity reactions are usually <5cm in largest diameter, sometimes have an urticarial appearance & typically begin to disappear within 24-48 hours. 2. Endemic area An endemic area is defined as a locality in which a reproducing population of Ixodes scapularis or Ixodes pacificus tick vectors is known to exist, as demonstrated by molecular methods, to support transmission of B. burgdorferi at that site. Endemic areas in NS: http://www.gov.ns.ca/hpp/cdpc/lyme.asp Endemic areas in Canada: http://www.phac-aspc.gc.ca/id-mi/tickinfo-eng.php Endemic areas in the USA: http://www.cdc.gov/mmwr/preview/mmwrhtml/mm5623a1.htm 3. Lyme Serology (Positive) Criteria for serologic testing are described by the guidelines of the Canadian Public Health Laboratory Network. Serologic evidence is confirmatory only in patients with EM or objective clinical evidence of disseminated Lyme disease, and a history of residence in, or visit to, an endemic area. Reporter’s Name/Signature: Document1 Collection Date (yyyy/mm/dd): / / 4