Ped ED Headache Treatment Protocol
advertisement
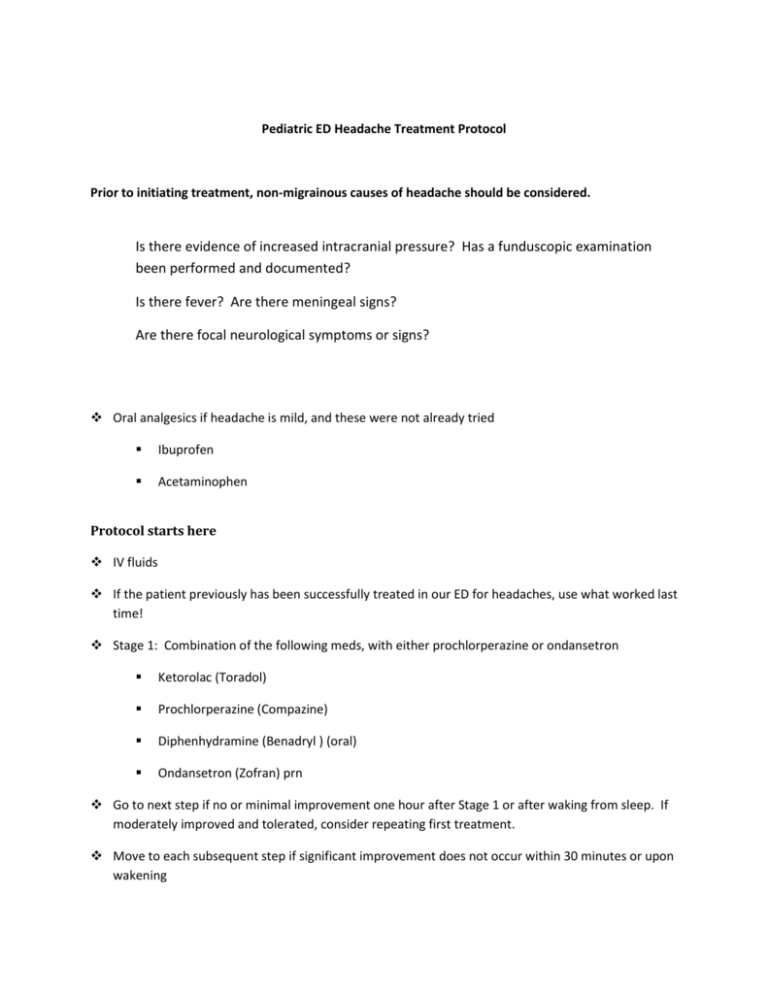
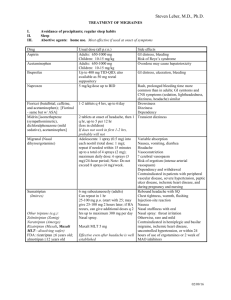
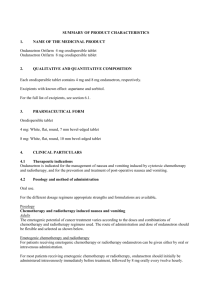
Pediatric ED Headache Treatment Protocol Prior to initiating treatment, non-migrainous causes of headache should be considered. Is there evidence of increased intracranial pressure? Has a funduscopic examination been performed and documented? Is there fever? Are there meningeal signs? Are there focal neurological symptoms or signs? Oral analgesics if headache is mild, and these were not already tried Ibuprofen Acetaminophen Protocol starts here IV fluids If the patient previously has been successfully treated in our ED for headaches, use what worked last time! Stage 1: Combination of the following meds, with either prochlorperazine or ondansetron Ketorolac (Toradol) Prochlorperazine (Compazine) Diphenhydramine (Benadryl ) (oral) Ondansetron (Zofran) prn Go to next step if no or minimal improvement one hour after Stage 1 or after waking from sleep. If moderately improved and tolerated, consider repeating first treatment. Move to each subsequent step if significant improvement does not occur within 30 minutes or upon wakening Stage 2: Triptans – use either rizatritan (preferred) or sumatriptan Contraindicated in hemiplegic, basilar migraines (and to be avoided in most patients with migraines with non-visual aura). (Basilar migraines are migraines with at least two brainstem symptoms; e.g., syncope, diplopia, bilateral sensory changes, tinnitus, vertigo, and ataxia.) Will also delay DHE use for 24 hours Use with caution in patients on SSRIs due to possible serotonin syndrome Oral Rizatriptan (Maxalt) o Melt (MLT) o Tablet o Only 10 mg on formulary but tablets (not MLT) can be split in half Children ≥6 years old and adolescents Note that safety and efficacy of multiple rizatriptan doses in a 24-hour period has not been established for pediatric patients. <40 kg: 5 mg as a single dose; maximum 15 mg in 24-hour period ≥40 kg: 10 mg as a single dose; maximum 30 mg in 24-hour period Adults: 5-10 mg, repeat after 2 hours if significant relief is not attained; maximum 30 mg in a 24-hour period Dosage adjustment with concomitant propranolol: Children ≥6 years old and adolescents : <40 kg: Do not use rizatriptan ≥40 kg: 5 mg as a single dose; maximum 15 mg in 24-hour period Adults: 5 mg; may repeat after 2 hours; maximum daily dose: 15 mg in a 24hour period Subcutaneous (alternative to rizatriptan: if rizatriptan historically ineffective or if oral medications not tolerated) Sumatriptan (Imitrex) 6 mg/0.5 mL o Children < 14 y.o. or <50 kg: 0.1 mg/kg, maximum 4.8 mg. Round to nearest 0.1 mL (1.2 mg, 2.4 mg, etc.). Do not repeat. ≥ 14 y.o. and ≥50 kg: 6 mg. Do not repeat. o Adults: 6 mg Stage 3 Methylprednisolone (Solumedrol) 15 mg/kg/dose, up to 1 gm. Do not repeat. Stage 4 Magnesium sulfate 15 mg/kg/dose, up to 1 gm. Do not repeat. Stage 5: CONTACT NEUROLOGY AT THIS POINT. The order of the subsequent treatment steps is not fixed, and should be determined by the patient’s past and present responses, and by preferences of the neurologist on-call and ED physician. In general, sequential treatment with one agent at a time is preferred to concurrent treatment with several agents. In addition, at this point the ED physicians will discuss with the Neurology team the next steps in management if needed, such as having the patient seen by a Neurology resident, obtaining a formal Neurology consultation in the ED, or admission. Valproic acid (Depacon); IV 15 mg/kg/dose, up to 1 gm. Do not repeat. Chlorpromazine (Thorazine) 0.1 mg/kg IV q 15 minutes up to 3 doses If prochlorperazine was previously given, chlorpromazine may have an additive sedative effect. Haloperidol lactate Age 6-12 years: 1-3 mg/dose IM up to q 4-8 hours. Maximum 0.15 mg/kg/day Age > 12: 2-5 mg/dose IM up to q 4-8 hours. If prochlorperazine was previously given, there is an increased risk of QT prolongation. Consider doing an EKG. Lorazepam 0.05-0.1 mg/kg/dose IV. Maximum 2-4 mg. Repeat only with MD order.