pharma 1
advertisement

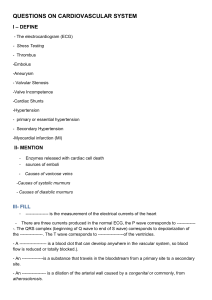
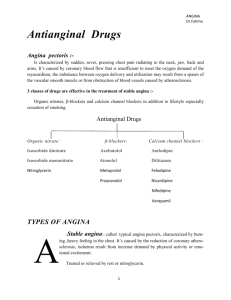
Drug type example Mechanism action Nitrates and nitrites Amyl nitrite 3-5 min 1-decrease cardiac demand Nitroglycerine From 10 mins to 2-decrease preload 10 hours(Depending upon route of administration) 3-increase cardiac delivery by remove coronary spasm Isosorbide mononitrate 6-10 h IS LONG ACTION AND TACK BY ORALLY Beta Blockers Propranolol 1-decrease cardiac demand Metoprolol 2-decrease afterload Atenolol 3- increase cardiac delivery by remove coronary spasm 4-decrease cardiac contractility and rate Calcium Channel Blockers Nifedipine 1-decrease cardiac demand Nicardipine 4-decrease cardiac contractility and rate Diltiazem Verapamil االلية المفصلة لعمل دواء النترات هي كالتالي ) glutathione S-transferase( ) حصل بواسطةdenitrated ( تصبحNitrates -1 )SH GROUB () عبر وجود مجموعةNO ( بعد ذلك سوف يتحرر عندنا ) هذه التحوالت كلها ال تتم اال بوجودguanylyl-cyclase ( ) تفعل دورةNO( لما يتحرر . بدونها لن تكمل العمليةSH GROUB مجموعة ) العضالت الملساءcGMP( سوف يتم زيادة توليف مركب-2 protein kinase G سوف يؤدي الى تنشيط مركبcGMP لما يتم صناعة هذا المركب-3 ) بعد ما حصل هذهdephosphorylation of myosin light chainوهذا يؤدي الى . العمليات كلها سوف ينتج بالنهاية ارتخاء في العضالت الملساء : نتائج هذه العملية كلها باختصار كالتالي 1-NO stimulates guanylyl-cyclase in platelets as in smooth muscle. 2- A decreased availability of tissue -SH groups reduces the action of nitrates ) سوف تقل من تنشيط النتراتSH groups( عندما تقل مجموعة Cardiovascular actions After therapeutic doses : 1- Marked relaxation of large veins بيكون من المنطق ان يحصل.. تخيل ماذا يحصل بالجسم..لما االوردة الكبيرة بالجسم تتوسع : مايلي a. Decreased preload and cardiac output b. Decreased blood pressure (slightly) الن االوردة اصبحت واسعة والضغط بيقل c. Improved perfusion of subendocardial regions (due to the lowering of left ventricular end-diastolic pressure, which reduces subendocardial compression التروية في طبقة تحت شغاف القلب سوف تتحسن بسبب انخفاض الضغط البطيني في نهاية . االنبساط لمن انخفض الضغط هذا ادت الى تقليل الضغط على منطقة تحت شغاف القلب 2- Relaxation of large arteries (less pronounced than vein relaxation) الشراين الكبيرة بالجسم ترتخي لكن بنسبة اقل من ارتخاء االوردة من المنطق لمن الشرايين :ترتخي ماذا يحصل ؟ سوف يزيد تدفق الدم في اماكن معينة بالجسم وهي Relaxation of large arteries which leads to increased blood flow in : a. The skin in (face and thorax) and the brain. b. Large epicardial vessels . c. Large collateral vessels perfusion of ischemic regions is increased) اذا تم اخذ الدواء بجرعات عالية ماذا سوف يحصل ؟ After higher doses: (Relaxation of all segment of the vascular system) which leads to: 1- Reflex tachycardia. 2- reflex increase in cardiac contractility. 3- Postural hypotension. Other actions in this drug : 1-Relaxation of smooth muscle of: a) b) c) d) the bronchi (small effect) the biliary system (rapid reduction of biliary pressure) the gastrointestinal tract (sphincteral and non sphincteral) the genitourinary tract (small effect) 2-Decreased platelet aggregation 3-Increased methemoglobin formation with nitrites, not with therapeutic doses of nitrates) due to the formation of nitrite ion that can oxidize the ferrous ion of hemoglobin to the ferric state. Methemoglobin is mean : تعني تحول الحديد( فيروس ايون) الموجود في الهيموجلوبين الى ( فيريك) وبالتالي تقل قدرته على .. حمل االكسجين ولذلك نالحظ جلد الشخص يكون ازرق …………………………………………………… *ABSORPTION the drug*: • Bioavailability: o Oral: generally low but isosorbide mononitrate > 95%) o Sublingual: 10-60 % o Transdermal 50-90 % DISTRIBUTION: In all body tissues including brain. BIOTRANSFORMATION: • > 99%, mainly in liver (by a high capacity nitrate-reductase). Half-life: very variable • Sublingual nitroglycerin: 2-3 min • Oral isosorbide mononitrate: 4-5 hours ………………………………………………………………………………………….. ))(( Nitrates Tolerance and Dependence ناخذ فكرة عامة عن معنى ): )Nitrates Tolerance لما يفرز الجسم NOعبر endotheliumيعمل ارتخاء للعضالت الملساء ويعمل vasodilationحتى يفرز الجسم ال NOالزم يكون عندنا مجموعة SHالن هي مفتاح خروج ال NOهذه المجموعة SHتكون موجدودة بكميات محددة في الخلية يعني مثال الجسم يفرزها وممكن تخلص ويفرزها مرة اخرى عندنا الحاجة وتخلص الكمية تكون كمية محدودة بالخلية فاذا خلصت مجموعة ال SHلن يتكون عندنا NOلذلك معنى كلمة Nitrates Toleranceهو ان الشخص لما ياخذ العالج اول مرة ياتي معه فائدة ولكن لما ياخذه مرة ثانية يشتكي ويقول الدواء ماله فايدة ولم يعالج االلم لماذا؟ الن مجموعة ال SHفي الجسم تكون استنفذت وحتى نعالج هذه المشكلة ننصح المرضى اما ان يقلل من جرعة الدواء الن كلما اكثر من الدواء سوف تقل ال SHوبالتالي الدواء لن يساعده وتستنفذ هذه المجموعة او نقول للشخص خذ الدواء مرة الفجر ومرة المغرب حتى يسمح للجسم ويعطي وقت للجسم ان يصنع مرة اخرى هذه المجموعة ال ...SH • Frequently repeated exposures to nitrates leads to a decrease in most of their pharmacological effects. • Tolerance to a nitrate results in tolerance (at least partial) to all other compounds of the class. • The amount of tolerance is a function of the dosage and the frequency of administration, and it exhibits a very high individual variability. • Since tolerance appears rapidly (24 hours) and disappears rapidly (6-10 hours), brief periods of no therapy (hours of overnight) can be sufficient to permit recovery. تذهب الن يكون، ساعات6 ساعة وتختفي بسرعة بعد22 المقاومة تظهر خالل الجسم كون عندنا االس اتش Nitrate can cause dependence. In fact sudden death or myocardial infarction have occurred after a few days' break in long-term exposure to an organic nitrate الننترات ممكن تسبب مثل االدمان عليه يعني نعتمد عليه بقوة الن الموت بسبب احتشاء القلب يحصل بعد . ايام قليلة من اخذ الدواء لفترة طويلة ثم قطعه وعدم اخذ الدواء Adverse effects of Nitrates 1-Central nervous system: • Throbbing headache…… 50%, can be severe • Dizziness, vertigo, lightheadedness • Syncope 2- Cardiovascular system • • • • Flushing of the face . Palpitations Postural hypotension Profound hypotension (if taken concomitantly with sildenafil, a specific cGMP phosphodiesterase-5 inhibitor. The inteaction can be life-threatening). Other systems: • Skin rashes, contact dermatitis • Methemoglobinemia (with nitrite, or with toxic doses of nitrates) • Withdrawal reactions (digital vasospasm, coronary spasms, myocardial ischemia, myocardial infarction) • Drug abuse (with amyl nitrite) Contraindications and Precautions: • • • • • • • Angina due to hypertrophic Cardiomyopathy Constrictive pericarditis Increased intracranial pressure Severe hypotension (systolic < 90 mm Hg) Hypovolemic states Hyperthyroidism Severe hepatic disease Therapeutic uses of nitrates 1- Angina pectoris 2. Heart failure 3. Myocardial infarction 4. Cyanide poisoning 1. Angina pectoris: 1-Treatment (or prevention) of the acute attack: Nitroglycerin (sublingual route) or amyl nitrite (inhalant route). [pain is relieved; protection lasts 30-40 min]. 2-Chronic prophylaxis: • Nitroglycerin (oral, transdermal), other nitrates (oral) [attacks are reduced or eliminated]. Main mechanisms of antianginal effects: A. In exertional angina: decreased myocardial O2 demand B. In variant angina: increased myocardial O2 supply (they are not the treatment of choice) C. In unstable angina: (decreased myocardial O2 demand, increased myocardial O2 supply, and decreased platelet aggregation, all might contribute to the therapeutic efficacy). High doses may cause undesirable effects due to: A. reflex tachycardia B. reflex increase in cardiac contractility 2- Heart failure • nitrates can increase stroke volume and cardiac output in patients with systolic heart failure (the decreased preload lowers the ventricular filling pressure, so allowing a more efficient ventricular contraction). They are not used routinely in heart failure but can be used when: 1- symptoms of pulmonary congestion predominate (redistribution of blood volume away from the chest relieves the congestion. This improves exercise tolerance even when cardiac output is not increased) 2- pulmonary edema occurs or is impending. 3- . Myocardial infarction • minor reduction in short-term mortality .انخفاض طفيف في معدل الوفيات على المدى القصير • not recommended for routine use, • but it is reasonable to use IV nitroglycerin in more complicated patients, such as those with impending heart failure or hypertension. مثل تلك التي،ولكن من المعقول أن استخدام النتروجليسرين الرابع في المرضى أكثر تعقيدا مع فشل القلب أو ارتفاع ضغط الدم وشيك . 4. Cyanide poisoning • Amyl nitrite and sodium nitrite are sometimes used to produce methemoglobin which can complex cyanide ion to form cyanomethemoglobin. • Then IV sodium thiosulphate is used to convert cyanomethemoglobin to thiocyanate and methemoglobin. Beta blockers Beta-blockers in Angina: They decrease cardiac O2 demand by: • Reducing heart rate • Reducing cardiac contractility • Lowering blood pressure b) They increase myocardial perfusion in certain parts of the heart >>>> subendocardial regions. Effective the Beta blockers: 1234- effective in chronic prophylaxis of exertional angina acute treatment of unstable angina. not effective in variant angina. High doses may cause undesirable effects due to: increased end diastolic volume increased ejection time Beta-blockers in Myocardial Infarction: Is reduce mortality in myocardial infarction. They should be given early and continued indefinitely. The mortality reduction is likely due to the following reasons: 1) They decrease myocardial oxygen demand 2) They decrease the risk of ventricular fibrillation 3) They limit the infarct size (so decreasing the risk of myocardial rupture) 4) They reduce myocardial remodeling اعادة ظهور Warning! withdrawal effects after chronic use of beta blockers in ischemic heart disease are well documented. In risk patients abrupt withdrawal may cause hypertension, angina, myocardial infarction, and sudden death Calcium Channels There are two types of calcium channels: 1- Ligand-gated (or "receptor-operated 2-Voltage-gated (or "potential-operated"): they open when the cell is depolarized. Voltage Gated Calcium Channels Type Location Properties of Ca++ current L (long-lasting) Smooth muscle, heart, neurons Long, high threshold T (Transiently opening) Heart, neurons Short, low threshold N Neurons Short, high threshold P Purkinje Long, high threshold Classification of Ca++ Channel Blocking Drugs Others Dihydropyridines Drug Vascular Selectivity Drug Vascular Selectiv Nifedipine High Verapamil Low Nicardipine Very High Diltiazem Low Bepridil Absent Mechanism of action: • Calcium channel blockers bind to the voltage-gated Ca++ channel of Ltype . • Verapamil and diltiazem block Ca++ channels both in the heart and in the vessels. • Dihydropyridines block Ca++ channels in the vessels only. • Blockade can be reversed by drugs that increase transmembrane flux of Ca++, such as beta-1 agonists. Cardiac actions: • • • • (Only verapamil and diltiazem can cause these effects) Decreased conduction (in "slow fibers"). Decreased automaticity . Increased refractoriness (markedly, but only in "slow fibers" or in fibers that fire frequently and are incompletely polarized at rest). Dose-dependent decrease of cardiac contractility. Vascular actions (All Ca++ channel blockers can cause these effects) • Vasodilation (mainly in arterioles) • Some dihydropyridines have a relative vascular selectivity (nicardipine for cerebral and coronary vessels) Other actions: • Relaxation of bronchiolar, gastrointestinal and uterine smooth muscle • Inhibition of insulin release (verapamil, nifedipine, after very high doses) • Inhibition of platelet aggregation (in vitro) • Blockade of P-glycoprotein which is a multidrug transporter associated with the development of drug resistance in cancer cells (verapamil). ABSORPTION: Oral bioavailability: variable (verapamil: 30% ) (amlodipine: 80%) Oral Tmax (time to reach maximum concentration): 30-60 min. DISTRIBUTION: In all tissues including brain. BIOTRANSFORMATION: > 99% in liver and other organs. Some metabolites are active. EXCRETION: < 1 % excreted by the kidney. Half-life: very variable (Diltiazem: . 3 hours; amlodipine . 40 hours) Adverse Effects: • • • • • • • • • • Central Nervous System Headache Dizziness, lightheadedness weakness Cardiovascular System Flushing (nifedipine ) Peripheral edema (nifedipine) Profound hypotension (mainly with immediate-release nifedipine) Tachycardia, palpitations (nifedipine) A-V block, bradycardia, arrhythmias (verapamil, diltiazem,) Ventricular fibrillation (verapamil, diltiazem) Aggravation of myocardial ischemia (nifedipine .) Other systems Constipation (verapamil ), gingival hyperplasia (verapamil ) nausea, heart burn, abdominal pain. • Contraindications and Precautions • Hypotension • Cardiogenic shock, systolic heart failure (verapamil, diltiazem) • SA and AV block, sick sinus syndrome (verapamil, diltiazem) • Arrhythmias associated with Wolff-Parkinson-White syndrome (verapamil, diltiazem) • Ventricular tachycardia (verapamil, diltiazem) • Myocardial ischemia (dihydropyridines) • Digoxin overdose • GERD, constipation, fecal impaction, intestinal obstruction, hemorrhoids Therapeutic Uses Angina pectoris: a) Exertional angina mainly because they decrease myocardial O2 demand (due to decreased afterload, heart rate and contractility) Verapamil and diltiazem are the preferred drugs. High doses may cause undesirable effects due to: increased end diastolic volume the increased ejection time b) Variant angina mainly because they increase myocardial O2 supply (due to coronary vasodilation) All calcium channel blockers are considered drugs of choice: High doses of dihydropyridines may cause undesirable effects due to: reflex tachycardia reflex increase in cardiac contractility Unstable angina and myocardial infarction: • During myocardial ischemia, an increase in Ca++ influx (due to membrane depolarization) can trigger a secondary cellular damage. • A cytoprotective effect, due to a decrease in the amount of necrosis in the heart tissue, has not been consistently supported by clinical studies, but these drugs can reduce the rate of reinfarction and death in patients without heart failure. Cardiac arrhythmias Hypertension • • • • • Hypertrophic cardiomyopathy and diastolic heart failure: Diltiazem (alone or in combination with beta-blockers) improves diastolic compliance by reducing myocardial contractility. Subarachnoid hemorrhage Dihydropyridines (especially nicardipine) dilate cerebral vessels at doses that have little effects in the periphery. Therefore they inhibit delayed reactive vasospasm arising from hemorrhage. Raynaud's phenomenon They are drugs of choice for relieving peripheral vasospasm. Migraine They are sometimes used for migraine prophylaxis (mechanism not established). Neuropsychiatric disorders Various neuropsychiatric disorders (rapid-cycling bipolar disorder, Tourette’s disease, Huntington’s disease). Long term-efficacy in these disorders remains to be established. Combination Therapy 1. Nitrates and B-blockers Each blocks the adverse effect of the other B-blockers – blocks the reflex tachycardia associated with nitrates Nitrates – attenuate the increase in the left ventricular end diastolic volume associated with B-lockers by increasing venous capacitance 2. CCBs and B-blockers -These two drugs produce decrease blood pressure -useful in the treatment of exertional angina that is not controlled adequately with nitrates and B-blockers -B-blockers – attenuate reflex tachycardia produce by nifedipine 3. Nitrates and CCB • Useful in severe vasospastic or exertional angina (particularly in patient with exertional angina with congestive heart failure and sick sinus syndrome) • Nitrates reduce preload • CCBs reduces the after load 4. CCB, BB, nitrates • Useful in patients with exertional angina not controlled by the administration of two types of anti-anginal agent