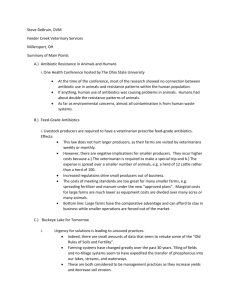
File - What is your food being fed? Antibiotics.
advertisement

http://www.nytimes.com/2013/12/12/health/fda-to-phase-out-use-of-someantibiotics-in-animals-raised-for-meat.html?pagewanted=all F.D.A. Restricts Antibiotics Use for Livestock By SABRINA TAVERNISE Published: December 11, 2013 252 Comments FACEBOOK TWITTER GOOGLE+ SAVE EMAIL SHARE PRINT REPRINTS WASHINGTON — The Food and Drug Administration on Wednesday put in place a major new policy to phase out the indiscriminate use of antibiotics in cows, pigs and chickens raised for meat, a practice that experts say has endangered human health by fueling the growing epidemic of antibiotic resistance. Brian C. Frank for The New York Times Pigs on a farm near Ralston, Iowa, where animals received antibiotics in their feed. Dark spots on their backs mean they are ready for market. This is the agency’s first serious attempt in decades to curb what experts have long regarded as the systematic overuse of antibiotics in healthy farm animals, with the drugs typically added directly into their feed and water. The waning effectiveness of antibiotics — wonder drugs of the 20th century — has become a looming threat to public health. At least two million Americans fall sick every year and about 23,000 die from antibiotic-resistant infections. “This is the first significant step in dealing with this important public health concern in 20 years,” said David Kessler, a former F.D.A. commissioner who has been critical of the agency’s track record on antibiotics. “No one should underestimate how big a lift this has been in changing widespread and long entrenched industry practices.” The change, which is to take effect over the next three years, will effectively make it illegal for farmers and ranchers to use antibiotics to make animals grow bigger. The producers had found that feeding low doses of antibiotics to animals throughout their lives led them to grow plumper and larger. Scientists still debate why. Food producers will also have to get a prescription from a veterinarian to use the drugs to prevent disease in their animals. Federal officials said the new policy would improve health in the United States by tightening the use of classes of antibiotics that save human lives, including penicillin, azithromycin and tetracycline. Food producers said they would abide by the new rules, but some public health advocates voiced concerns that loopholes could render the new policy toothless. Health officials have warned since the 1970s that overuse of antibiotics in animals was leading to the development of infections resistant to treatment in humans. For years, modest efforts by federal officials to reduce the use of antibiotics in animals were thwarted by the powerful food industry and its substantial lobbying power in Congress. Pressure for federal action has mounted as the effectiveness of drugs important for human health has declined, and deaths from bugs resistant to antibiotics have soared. Under the new policy, the agency is asking drug makers to change the labels that detail how a drug can be used so they would bar farmers from using the medicines to promote growth. The changes, originally proposed in 2012, are voluntary for drug companies. But F.D.A. officials said they believed that the companies would comply, based on discussions during the public comment period. The two drug makers that represent a majority of such antibiotic products — Zoetis and Elanco — have already stated their intent to participate, F.D.A. officials said. Companies will have three months to tell the agency whether they will change the labels, and three years to carry out the new rules. Additionally, the agency is requiring that licensed veterinarians supervise the use of antibiotics, effectively requiring farmers and ranchers to obtain prescriptions to use the drugs for their animals. “It’s a big shift from the current situation, in which animal producers can go to a local feed store and buy these medicines over the counter and there is no oversight at all,” said Michael Taylor, the F.D.A.’s deputy commissioner for foods and veterinary medicine. Some consumer health advocates were skeptical that the new rules would reduce the amount of antibiotics consumed by animals. They say that a loophole will allow animal producers to keep using the same low doses of antibiotics by contending they are needed to keep animals from getting sick, and evading the new ban on use for growth promotion. More meaningful, said Dr. Keeve Nachman, a scientist at the Johns Hopkins Center for a Livable Future, would be to ban the use of antibiotics for the prevention of disease, a step the F.D.A. so far has not taken. That would limit antibiotic uses to treatment of a specific sickness diagnosed by a veterinarian, a much narrower category, he said. Another skeptic, Representative Louise M. Slaughter, a Democrat from New York, said that when the European Union tried to stop companies from using antibiotics to make farm animals bigger, companies continued to use antibiotics for disease prevention. She said antibiotic use only declined in countries like the Netherlands that instituted limits on total use and fines for noncompliance. But another longtime critic of the F.D.A. on antibiotics, Dr. Stuart B. Levy, a professor of microbiology at Tufts University and the president of the Alliance for the Prudent Use of Antibiotics, praised the new rules. He was among the first to identify the problem in the 1970s. “I’m kind of happy,” he said. “For all of us who’ve been struggling with this issue, this is the biggest step that’s been taken in the last 30 years.” Mr. Taylor, the agency official, said the F.D.A. had detailed what veterinarians needed to consider when they prescribed such drugs. For example, use has to be for animals at risk for developing a specific disease, with no reasonable alternatives to prevent it. “It’s far from being a just-trust-them system,” he said. “Given the history of the issue, it’s not surprising that there are people who are skeptical.” He added that some food producers had already curbed antibiotic use. A spokeswoman for Zoetis, a major drug producer that said it would abide by the new rules, said the new policy was not expected to have a big effect on the revenues of the company because many of its drug products were also approved for therapeutic uses. (Dr. Nachman said that was an indication that overall use might not decline under the new rules.) The Animal Health Institute, an association of pharmaceutical companies that make drugs for animals, said that it supported the policy and “will continue to work with the F.D.A. on its implementation.” The National Pork Producers Council was less enthusiastic, saying, “We expect that hog farmers, and the federally inspected feed mills they purchase feed from, will follow the law.” “It is part of our ethical responsibility to utilize antibiotics responsibly and part of our commitment to public health and animal health,” the council said in a statement. The National Chicken Council said in a statement that its producers already worked closely with veterinarians, and that much of the antibiotics used in raising chickens were not used in human medicine. http://www.agweb.com/article/using_feedgrade_antibiotics_for_livestock_changes_are_coming_NAA_University_News_Release / Recently, livestock producers and veterinarians have been hearing about changes coming in the way antibiotics are used in food animals. In mid-December, the Food and Drug Administration (FDA) published a final "guidance for industry" that starts the clock running on some of these changes. Initially, it’s the animal health companies that will be adjusting their practices -- adjustments that will eventually make their way down to the people who prescribe and use the drugs: veterinarians and livestock producers. The role of livestock antibiotics in contributing to resistant bacterial infections in humans is complex and has been longdebated. Producer associations have seen the writing on the wall for a couple of years now that these changes were coming. But what do they actually mean for producers? What will change: The labeled uses of "medically important" antibiotics for growth promotion and improvements in feed efficiency will go away. The FDA is asking drug manufacturers to voluntarily take these uses off their products’ labels. Because extra-label use of feed grade antibiotics is illegal, these uses will no longer be legal as well. The companies have until mid-March to tell the FDA what products they plan to do this with. After that, they have three years to make the label changes, so livestock producers currently using antibiotics for growth promotion will have time to adjust, depending on how quickly the companies switch over. The list of what FDA considers "medically important" antibiotics is pretty long. It contains older drugs like tetracyclines and penicillin along with classes of drugs that are more critical to human medicine, such as cephalosporins and fluoroquinolones. When it comes to growth-promoting antibiotics that fall into this category, it’s drugs like tetracyclines, tylosin, and neomycin that will be affected. These "medically important" products will shift from over-thecounter to "Veterinary Feed Directive" (VFD) classification – possibly with new label indications for treatment, control, or prevention. The VFD is not a new classification; it’s currently being used for newer feed-grade drugs like Pulmotil® in pigs and cattle and Nuflor® in pigs and fish. This means that before a producer can obtain (for example) CTC (chlortetracycline) crumbles for his calves or pigs, he will have to obtain a VFD form filled out by his veterinarian. The form will specify the farm and animals to be treated, the duration of treatment, and which drug is to be used. The feed mill or distributor would need to have a properly completed VFD before they could supply the feed. The VFD won’t be able to come from just any veterinarian. A veterinarian would only be able to issue a VFD for use in animals "under his or her supervision or oversight in the course of his or her professional practice, and in compliance with all applicable veterinary licensing and practice requirements." Right now VFD’s have to be issued in the midst of a valid veterinary-client-patient relationship (VCPR) that’s spelled out by federal regulation. The new changes add some flexibility in that this relationship will be deemed appropriate by state and professional entities, such as the Board of Veterinary Examiners in South Dakota. This flexibility means that far-flung cattle enterprises may not need to be treated the same as an intensely managed hog operation, in regards to veterinary oversight. But it still means that a veterinarian needs to be involved – one that knows the operation and its needs well. The VFD forms will be easier to manage. Everyone’s recordkeeping requirement will be cut from 2 years to 1 year. The forms will be able to be transmitted and stored electronically. And thankfully for this veterinarian, they will no longer have to include an estimate of how much of the medication the animals will consume in the given time frame (this was hard to accurately guess a lot of times). The form will need to simply specify the inclusion rate of the drug, the number of animals to be fed, and the duration of the feeding. What won’t change: The ability to use feed-grade antibiotics to treat, control, or prevent bacterial diseases. The term "prevention" is used in the situation where there is a very high risk of illness if you don’t administer the antibiotic. However, producers will need to obtain a VFD for these products as explained above. How one uses and obtains non-"medically important" feed grade products. Examples of these include ionophores like Rumensin®, Bovatec®, most coccidiosis medications, and certain growth-promoting medications like bacitracin (BMD®). Since they’re not used very often if at all in human medicine, there will be no changes in their use. Uses of water and injectable antibiotics – yet. There are proposals out there that would move water medications to "prescription" status like many injectable antibiotics. Extra label uses of feed-grade medications. Any use of feed grade medications not in accordance with their label is illegal now, and it will remain so. The ability of current distributors and feed mills to supply these products. Yes, there will be more paperwork related to more VFD forms, but these new proposals do not limit these businesses in what they can carry or manufacture. The need for veterinarians to be involved in decisions about feedgrade antibiotics. There is no better source of information about the proper uses of these products in livestock populations than the herd veterinarian. A close relationship with a veterinarian means that producers may avoid wasting time and money on ineffective uses of these products. Better yet, it may result in practical advice on how to prevent illnesses that would necessitate the uses of these products. Antibiotic resistance is a complex and sometimes contentious topic among animal and human health professionals. The complexity of the issue means that a "silver bullet" solution is not going to present itself any time soon. All of us involved in using these products—in animals and people alike—play a role in ensuring that they continue to work for the sake of our animals and our family members. Understanding these proposed changes and proactively deciding how they will work into your operation is a great first step that we can all take. NOTE: Product trade names are used for purposes of illustration only and do not constitute an endorsement of those products. http://www.washingtonpost.com/national/health-science/fda-allows-antibioticsin-animal-feed-despite-potential-risk-to-human-health-reportclaims/2014/01/27/63a73a88-869e-11e3-916e-e01534b1e132_story.html The Food and Drug Administration has continued to allow dozens of antibiotics to be used in livestock feed, despite findings from its researchers that the drugs could expose humans to antibiotic-resistant bacteria through the food supply, an environmental advocacy group said in a report Monday. FDA officials reviewed about 30 animal-feed additives between 2001 and 2010, rating 18 of them “high risk” in terms of contributing to health problems in humans, according to records obtained through the Freedom of Information Act by the Natural Resources Defense Council. The remaining drugs the agency examined did not have adequate data to determine whether they were safe, the report said. According to the NRDC, at least 26 of the feed additives that FDA researchers reviewed — some of which have been in use since the 1950s — did not meet standards set by the agency in 1973 that required companies to submit scientific studies proving that the drugs were safe. The report comes amid increasing worries in the public health world about the problem of antibiotic-resistant infections, which sicken millions of Americans each year and kill an estimated 23,000. Public health officials across the globe have warned that the misuse and overuse of antibiotics are causing more and more of the drugs to lose their effectiveness, meaning that even routine infections could become untreatable. Carmen Cordova, an NRDC microbiologist and lead author of the analysis, called the FDA’s failure to act on its own findings “a breach of their responsibility and the public trust.” Avinash Kar, an NRDC lawyer, said it underscores a larger pattern of FDA inaction in combating the overuse of antibiotics in animals, something scientists and doctors widely believe is contributing to the proliferation of hard-to-treat infections. “They are not meeting their responsibility to protect public health,” Kar said. “They need to be doing better.” The penicillin- and tetracycline-based antibiotics at the center of the NRDC’s analysis were approved for “non-therapeutic” or “subtherapeutic” uses, such as bolstering growth in animals. In a statement Monday, the FDA said the review highlighted in the NRDC report was “part of the agency’s overall effort to assess available, current information regarding antimicrobial resistance concerns associated with the use of medically important antimicrobial drugs in food-producing animals.” Rather than focus on specific drugs, the agency said, it decided to pursue a broader strategy of trying to phase out non-therapeutic uses of antibiotics over time. It is unclear how many of the drugs the agency examined continue to be sold by manufacturers. NRDC researchers said they found evidence suggesting that at least nine of the feed additives continue to be marketed; aside from two that companies voluntarily withdrew, all others remain approved for use. Although the FDA did send letters to some companies seeking more information about concerns that the drugs might promote antibiotic resistance, the documents obtained by the NRDC did not show that the agency took further action or that the companies submitted additional safety studies, the report states. The vast majority of antibiotics sold each year in the United States — by some estimates as much as 80 percent — are used in agriculture rather than in human medicine. Consumer and environmental groups have pressed lawmakers and regulators to do more to limit the amount of antibiotics given to animals, particularly those classes of drugs also used to treat humans. Last fall, the Centers for Disease Control and Prevention issued an alarming report detailing the growing threat of antibioticresistant infections. Although most such infections arise in hospitals and nursing homes, officials underscored the widespread use of antibiotics in animals as a looming concern. “Resistant bacteria can contaminate the foods that come from those animals, and people who consume these foods can develop antibiotic-resistant infections,” the CDC report stated. “The use of antibiotics for promoting growth is not necessary, and the practice should be phased out.” The FDA seems to agree. In 1977, the agency said it planned to withdraw approval for some animal antibiotics, especially those used for nonmedical reasons. But for decades, the agency took no action, even as the NRDC sued in recent years, trying to force it to follow through. In December, the FDA took long-awaited steps aimed at scaling back the use of antibiotics in livestock. The agency asked animaldrug manufacturers to alter their labels so that farmers would no longer be allowed to use antibiotics merely to promote growth. It also wants farmers to get approval from a veterinarian before administering the drugs to livestock. The agricultural industry largely welcomed the move, saying it would lead to meaningful changes in how antibiotics are used on farms. Consumer advocates and some public health officials were less than impressed, saying the FDA didn’t go far enough and complaining that its recommendations were voluntary. The FDA said Monday it remains confident that its current approach, which will give animal-drug companies and the agricultural industry several years to adapt, “is the most efficient and effective way to change the use of these products in animal agriculture.” http://www.fda.gov/forconsumers/consumerupdates/ucm378100.htm The Food and Drug Administration (FDA) is implementing a voluntary plan with industry to phase out the use of certain antibiotics for enhanced food production. Antibiotics are added to the animal feed or drinking water of cattle, hogs, poultry and other food-producing animals to help them gain weight faster or use less food to gain weight. Because all uses of antimicrobial drugs, in both humans and animals, contribute to the development of antimicrobial resistance, it is important to use these drugs only when medically necessary. Governments around the world consider antimicrobial-resistant bacteria a major threat to public health. Illnesses caused by drugresistant strains of bacteria are more likely to be potentially fatal when the medicines used to treat them are rendered less effective. FDA is working to address the use of “medically important” antibiotics in food-producing animals for production uses, such as to enhance growth or improve feed efficiency. These drugs are deemed important because they are also used to treat human disease and might not work if the bacteria they target become resistant to the drugs’ effects. “We need to be selective about the drugs we use in animals and when we use them,” says William Flynn, DVM, MS, deputy director for science policy at FDA’s Center for Veterinary Medicine (CVM). “Antimicrobial resistance may not be completely preventable, but we need to do what we can to slow it down.” FDA is issuing a final guidance document that explains how animal pharmaceutical companies can work with the agency to voluntarily remove growth enhancement and feed efficiency indications from the approved uses of their medically important antimicrobial drug products, and move the therapeutic uses of these products from over-the-counter (OTC) availability to marketing status requiring veterinary oversight. Once manufacturers voluntarily make these changes, the affected products can then only be used in food-producing animals to treat, prevent or control disease under the order of or by prescription from a licensed veterinarian. “This action promotes the judicious use of important antimicrobials, which protects public health and, at the same time, ensures that sick and at-risk animals receive the therapy they need,” says CVM Director Bernadette Dunham, DVM, Ph.D. “We realize that these steps represent changes for veterinarians and animal producers, and we have been working to make this transition as seamless as possible.” back to top Drugs Primarily in Feed Flynn explains that all the drugs affected by this plan are antibacterial products. They have long been FDA-approved for production (e.g. growth enhancement) purposes as well as for the treatment, control or prevention of animal diseases. Even today, he says, it is not entirely understood how these drugs make animals grow faster. The drugs are primarily added to feed, although they are sometimes added to the animals’ drinking water. Bacteria evolve to survive threats to their existence. In both humans and animals, even appropriate therapeutic uses of antibiotics can promote the development of drug resistant bacteria. When such bacteria enter the food supply, they can be transferred to the people who eat food from the treated animal. In 2010, FDA called for a strategy to phase out production use of medically important antimicrobial products and to bring the remaining therapeutic uses under the oversight of a veterinarian. The guidance document that FDA is issuing on Dec. 11, 2013, which was previously issued in draft form in 2012, lays out such a strategy and marks the beginning of the formal implementation period. The agency is asking animal pharmaceutical companies to notify FDA within the next three months of their intent to voluntarily make the changes recommended in the guidance. Based on timeframes set out in the guidance, these companies would then have three years to fully implement these changes. To help veterinarians and producers of food-producing animals comply with the new terms of use for these products once the recommended changes are implemented, FDA is proposing changes to the Veterinary Feed Directives (VFD) process. This is an existing system that governs the distribution and use of certain drugs (VFD drugs) that can only be used in animal feed with the specific authorization of a licensed veterinarian. Flynn explains that feed-use antibiotics that are considered medically important and are currently available as OTC products will, as a result of implementation of the guidance document, come under the VFD process. The proposed changes to the VFD process are intended to clarify the administrative requirements for the distribution and use of VFD drugs and improve the efficiency of the VFD program. Such updates to the VFD process will assist in the transition of OTC products to their new VFD status. back to top Why Voluntary? Flynn explains that the final guidance document made participation voluntary because it is the fastest, most efficient way to make these changes. FDA has been working with associations that include those representing drug companies, the feed industry, producers of beef, pork and turkey, as well as veterinarians and consumer groups. "Based on our outreach, we have every reason to believe that animal pharmaceutical companies will support us in this effort," says Michael R. Taylor, FDA's deputy commissioner for foods and veterinary medicine. This article appears on FDA's Consumer Updates page, which features the latest on all FDA-regulated products. http://www.webmd.com/food-recipes/news/20100628/fda-antibiotics-inlivestock-affects-human-health Giving animals antibiotics in order to increase food production is a threat to public health and should be stopped, the FDA said today. The federal agency says it has the power to ban the practice, but it's starting by issuing "draft guidance" in hopes the food industry will make voluntary changes. After a 60-day public comment period, the guidance will become FDA policy. The guidance is based on two principles: Antibiotics should be given to food animals only to protect their health. All animal use of antibiotics should be overseen by veterinarians. "We are seeing the emergence of multidrug-resistant pathogens," FDA Deputy Commissioner Joshua Sharfstein, MD, said at a news conference. "FDA believes overall weight of evidence supports the conclusion that using medically important antimicrobial drugs for production purposes is not appropriate." Sharfstein said it's a public health issue when antibiotics important for human health are given to animals on a massive scale. Such use encourages the growth of drug-resistant bacteria that can cause hard-totreat human disease. Like humans, animals sometimes need antibiotics to fight or prevent specific infections. The FDA says it has no problem with this. But producers regularly give antibiotics to food animals because it makes them gain weight faster or makes them gain more weight from the food they eat. This is the practice the FDA wants to end. Sharfstein hopes that by offering the carrot of voluntary guidelines, industry will avoid the stick of new regulations. "We are not expecting people to change tomorrow. This is the first step in FDA establishing principles from which we could move to other steps, such as oversight," Sharfstein said. "This does not tell people what to do, it establishes principles and tells people how to achieve those principles." http://msutoday.msu.edu/news/2013/unchecked-antibiotic-use-in-animals-mayaffect-global-human-health/ The increasing production and use of antibiotics, about half of which is used in animal production, is mirrored by the growing number of antibiotic resistance genes, or ARGs, effectively reducing antibiotics’ ability to fend off diseases – in animals and humans. A study in the current issue of the Proceedings of the National Academy of Sciences shows that China – the world’s largest producer and consumer of antibiotics – and many other countries don’t monitor the powerful medicine’s usage or impact on the environment. On Chinese commercial pig farms, researchers found 149 unique ARGs, some at levels 192 to 28,000 times higher than the control samples, said James Tiedje, Michigan State University Distinguished Professor of microbiology and molecular genetics and of plant, soil and microbial sciences, and one of the co-authors. “Our research took place in China, but it reflects what’s happening in many places around the world,” said Tiedje, part of the research team led by Yong-Guan Zhu of the Chinese Academy of Sciences. “The World Organization for Animal Health and the U.S. Food and Drug Administration have been advocating for improved regulation of veterinary antibiotic use because those genes don’t stay local.” Antibiotics in China are weakly regulated, and the country uses four times more antibiotics for veterinary use than in the United States. Since the medicine is poorly absorbed by animals, much of it ends up in manure – an estimated 700 million tons annually from China alone. This is traditionally spread as fertilizer, sold as compost or ends up downstream in rivers or groundwater, taking ARGs with them. Along with hitching rides in fertilizer, ARGs also are spread via international trade, immigration and recreational travel. Daily exposure to antibiotics, such as those in animal feed, allows microbes carrying ARGs to thrive. In some cases, these antibiotic resistant genes become highly mobile, meaning they can be transferred to other bacteria that can cause illness in humans. This is a big concern because the infections they cause can’t be treated with antibiotics. ARGs can reach the general population through food crops, drinking water and interactions with farm workers. Because of this undesirable cycle, ARGs pose a potential global risk to human health and should be classified as pollutants, said Tiedje, an MSU AgBioResearch scientist. “It is urgent that we protect the effectiveness of our current antibiotics because discovering new ones is extremely difficult,” Zhu said. “Multidrug resistance is a global problem and must be addressed in a comprehensive manner, and one area that needs to be addressed is more judicious use and management of wastes that contain ARGs.” Additional MSU researchers contributing to the study include Timothy Johnson, doctoral researcher, Robert Stedtfeld, civil and environmental engineer, and Syed Hashsham, civil and environmental engineering professor. - See more at: http://msutoday.msu.edu/news/2013/unchecked-antibiotic-use-inanimals-may-affect-global-human-health/#sthash.HRUwjXaD.dpuf