NICU Resident Handbook: St. Paul Campus
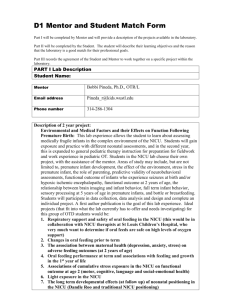
advertisement

Children’s Hospitals and Clinics of Minnesota NICU - St. Paul Campus CHAPTERS 1. Introduction 2. Respiratory Management 3. Fluid-Electrolytes-Nutrition 4. Pharmacology 5. Discharge Information 6. Clinical CHAPTER 1. GENERAL INTRODUCTION FOR RESIDENTS I. Introduction II. Goals of Resident Rotation III. Careteam Roles IV. Rounds V. Resident On-Call/Weekend Expectations VI. Neonatology On-Call VII. Notes VIII. Consultations IX. Conferences X. Supplemental curriculum XI. Infection Control XII. Miscellaneous NICU Information I. INTRODUCTION Welcome to the NICU at Children’s Hospitals and Clinics of Minnesota, St. Paul Campus. We are a regional perinatal center serving primarily the greater St. Paul area, as well as western Wisconsin. Although most of our babies are delivered at United/Children’s Perinatal Center, about 15% of our babies are transported in from other hospitals. We provide level II and level III neonatal diagnostic and supportive care including mechanical ventilation, high frequency ventilation, nitric oxide therapy and pediatric surgery. This does not include ECMO; for this therapy, patients are referred to the NICU at the Minneapolis campus. In addition, we are offer a regional Infant Apnea Program and staff the NICU developmental Follow-Up Clinic. II. GOALS OF RESIDENT ROTATION 1. Understand pathophysiology and treatment of common newborn diseases; 2. Develop procedural skills in newborn resuscitation and emergency intervention; 3. Recognize clinical and laboratory signs of a sick newborn and develop appropriate treatment plans; 4. Recognize common congenital malformations and syndromes; 5. Identify high-risk obstetrical factors. 6. Understand normal newborn physiology and examination findings. III. RESIDENT ROTATION OBJECTIVES A. Patient Care 1. Gather essential and accurate information regarding patients for daily rounds 2. Make informed clinical decisions about diagnostic and therapeutic interventions based on patient information and preferences, upt-to-date scientific evidence, and clinical judgment (in consultation with the attending neonatologist or neonatology fellow). 3. Develop and carry out patient management plans in daily rounds with attending neonatologist and neonatology fellow. 4. Counsel and educate patient families. 5. Use information technology to support patient care decisions and patient education. 6. Perform competently all medical and invasive procedures considered essential for Level II Nursery care including newborn resuscitation, endotracheal intubation, umbilical artery and vein catheterization, and lumbar puncture. 7. Provide health care services aimed at preventing health problems or maintaining health in the Level-II Nursery setting, including anticipatory guidance and teaching for parents. 8. Work effectively with a multidisciplinary team of NICU professionals to provide patient-and family-centered care. B. Medical Knowledge 1. Demonstrate an investigatory and analytic thinking approach to clinical situations. 2. Utilize core reading list, online media, and self-assessment tools provided at course website to develop core knowledge base for the practice of Level II Nursery care and management of common neonatal problems and conditions as described below: a. Recognize features of prematurity, common minor and major anomalies and birth defects, in contrast to normal newborn exam findings. b. Recognize special nutritional needs of the sick or preterm infant. c. Understand benefits of breast milk and breastfeeding. d. Recognize signs of feeding intolerance and intestinal obstruction and provide appropriate intervention. e. Understand the importance of neonatal jaundice and its timely evaluation and treatment. f. Describe the impact of maternal diabetes on the physiology of the fetus and newborn infant. g. Identify and manage common respiratory problems such as respiratory distress syndrome (RDS), transient tachypnea of the h. i. j. k. l. m. newborn (TTN), pneumonia, meconium aspiration, and pneumothorax. Recognize the signs and symptoms of congenital heart disease. Describe the epidemiology, signs and symptoms, and management of early- and late-onset neonatal sepsis. Describe the etiology and first line management of neonatal seizures. Understand the clinical associations and management of apnea of prematurity and other forms of newborn apnea as well as sudden infant death syndrome (SIDS). List newborn emergencies commonly encountered in the first month of life and describe typical management of each. Describe the correct technique for the placement of umbilical catheters, endotracheal intubation, and lumbar puncture. C. Communication Skills 1. Make daily contact with each patient family to create and sustain a therapeutic and ethically sound relationship. 2. Use effective listening skills and elicit and provide information using effective nonverbal, explanatory, questioning and writing skills. 3. Work effectively with others as a member of the health care team. 4. Facilitate learning of medical students. D. Professionalism 1. Demonstrate respect, compassion, and integrity along with a responsiveness to the needs of patients and society that supersedes selfinterest. 2. Demonstrate accountability for patient care. 3. Demonstrate a commitment to ethical principles pertaining to provision or withholding of clinical care and confidentiality of patient information. E. Systems-based Practice 1. Understand neonatal care within the larger context of the profession of pediatrics and practice within a pediatric hospital and health care community and effectively call upon available resources to optimize value. F. Practice-based Learning and Improvement 1. Continuously self-assess own patient care, appraisal and assimilation of scientific evidence, and improvements in patient care. III. ROLES A. Fellow and Attending In general, both the fellow and attending will make daily rounds on every patient. On occasion, rounds will be under the direction of the fellow. No significant change in plans made during rounds should be made without consultation with the fellow or attending. The on-call fellow or attending should be notified of all admissions (day or night). The fellow is available for supervision of all procedures during the daytime. There is an inhouse attending 24/7 that can provide supervision of all patient care and procedures. B. Neonatal Nurse Practitioners Neonatal nurse practitioners are nurses with advanced education/training and certification in neonatal resuscitation and stabilization. They function as care providers in collaboration with staff physicians. They are skilled at NICU invasive procedures. They are present 24 hours per day in-house and will assist you in attending all deliveries, providing daily patient care and performing procedures as needed. C. Pediatric Interns Pediatric interns are MDs in their first year of pediatric specialty training. They will provide care to patients in the NICU in collaboration with the fellow and staff physicians. They will attend deliveries as well as perform common neonatal procedures during their rotation in the NICU. Pediatric interns will work a 6 day/week rotation throughout their NICU month, with no overnight call responsibilities. Each intern will always have one day per week off, with the day off being scheduled on either Friday, Saturday, or Sunday. They will sign-out their patient population at 5:30pm each day to the overnight on-call coverage team. D. Charge Nurses The charge nurse decides where the infants will be placed in the NICU and makes the assignments for RN staffing of the unit. The charge nurses are the “go-between” for staff RNs and the providers. Charge nurses are extremely valuable in making sure the day-to-day operations run smoothly. E. Social Workers Social workers provide support to families while their babies are hospitalized in the NICU. In general, this includes emotional support as families adjust to having an ill or premature baby, assisting with finding resources in the hospital or community, and helping the families understand communications with the medical team. NICU social workers are also committed to supporting staff members, realizing that families’ experience is directly affected by the resiliency of those caring for their baby. F. Care Managers Care managers coordinates the pre-discharge, discharge and follow-up experience for the NICU patients. They deal with various insurance issues, and also is involved with predischarge education of families. They also coordinate transfers back to referral hospitals when medically appropriate. IV. ROUNDS AND PATIENT ASSINGMENT Residents should arrive at the NICU each morning in time to be updated on their patients by the previous on-call team, typically no later than 7:30am. It is expected that you will have examined all patients who are critically ill prior to rounds, with any noncritical patients to be examined during rounds. Rounds commence at 8:15 am in the Radiology Department where x-rays are reviewed prior to formal rounds in the NICU. On weekends, rounds begin in the NICU typically between 7:30 and 8:00 am and X-ray. rounds will take place once the on-call radiologist arrives. Patients will be added to interns’ census at the discretion of the neonatologist/fellow from appropriate patients admitted during the course of day and interns will have the opportunity to participate in the admission process including H&P and admission orders. Patients will also be assigned overnight after being admitted by the NNP for the intern to assume care the following morning. V. WEEKEND WORKLOAD EXPECTATIONS Each intern will be assigned to work one day of the weekend, with the other day being off. The weekend workday will function the same as the weekday, however, one intern will cover ALL of the resident patient population since the other resident will have the day off. VI. DAILY NOTES 1. “SOAP” format progress notes should be written in the EMR each day your patients. 2. A procedure note must be completed in the EMR for all procedures. 3. A “Change in Status” note must be written in the EMR any time a major change in patient status occurs. 4. A Post-Op note must be completed in the EMR when a patient returns from surgery. VII. CONSULTATIONS Only the attending neonatologist or fellow can decide to obtain a subspecialty consult, and choose the designated consultant. Typically, the attending or fellow will contact the consultant, however, this should be clarified during rounds regarding who will be responsible for making the call to the consultant, as occasionally, residents are asked to contact consultants. VIII. CONSENT/PARENT NOTIFICATION A general consent to treatment is signed by the parents upon admission to the NICU for all admission and subsequent NICU treatments and procedures. However, out of courtesy, all parents should be informed of any procedures that are happening to their baby. Parents should be notified of any consults, major test results, or significant changes in their infant’s condition. Parents should be informed prior to any blood transfusion (PRBC, FFP, Platelets, etc). The transfusion order will ask if consent has been obtained; once informed consent is obtained you do not need to obtain informed consent for each transfusion (unless that is an issue with that family), but out of courtesy, the family should still be informed that a transfusion will take place. IX. CONFERENCES/DIDACTIC TEACHING SESSIONS 1. On the third Thursday of each month there is a Mortality Conference where all NICU and delivery room deaths or adverse events will be discussed as well as review of all autopsies with Pathology 2. The NICU Fellows will give several didactic lectures in the afternoons, after rounds, on specific topics. X. SUPPLEMENTAL EDUCATIONAL CURRICULUM 1. A 4-week educational reading series is posted on our website, WWW.NEWBORNMED.COM, and it is the expectation that you read each week’s assigned readings during your rotation and complete the post-test after each reading to demonstrate completion. Completion of the reading series is mandatory and will be a part of your evaluation. The reading lists can be found under the resident/fellow tab on the website and the password is “meconium”. 2. OPTIONAL: It is recommended that you register for CLIPP Cases (computer assisted learning in pediatrics project). To register, go to www.clippcases.org, and click on “CLIPP Pediatric” cases. Click on “go to cases”. “You are new user?” click “register”. Fill in your information using your university x500 email address. Your user name and password will be emailed to you. a. The following Pediatric CLIPP cases should be reviewed during your month in the NICU: #1 (Eval of newborn infant), #2 (prenatal and newborn visits), #7 (newborn resp distress), #8 (jaundice), #9 (lethargy), #15 (vomiting), #18 (poor feeding), #25 (apnea), #26 (not gaining weight), #29 (hypotonia). The following Family Medicine CLIPP cases are pertinent: #24 (fussiness). XI. INFECTION CONTROL 1. Follow posted isolation procedures on the doors of patient rooms 2. Wash hands and arms up to elbows thoroughly upon entering the NICU each day. Foam-in and foam-out of all patient rooms (up to elbows). 3. Wear gloves for all patient contact (no exceptions!) 4. No rings, watches, bracelets are allowed in the NICU. 5. No painted or artificial fingernails are allowed in the NICU 6. There is no specific dress code in the NICU. However, parents and staff 7. appreciate a neat appearance if you wear street clothes. Arms should be bare below the elbow to promote good hand hygiene when examining patients. Feel free to wear scrubs daily, if you want. If you are attending deliveries you should wear scrubs or place appropriate gowns over your street clothes. XII. MISCELLANEOUS NICU INFORMATION 1. TPN orders need to be completed by 2:00 pm daily because the TPN is formulated in the Minneapolis campus central pharmacy and has to be couriered over to our campus in the late afternoon. 2. Routine “AM” labs are drawn between 0600-0700. Standing lab order times should be 1500, 2200, and 0300. Please try to place lab orders at the scheduled times, unless clinical status requires deviation. 3. When ordering labs, specify date and time of lab as well as if the nurse will obtain the specimen (eg. Patient has central access) or if laboratory will draw specimen (capillary stick or venipuncture). 4. When infant has a Broviac catheter labs should be ordered for 2000 as this is when the line will be “broken/opened” when new TPN is hung. 5. Weekly nutrition labs, when indicated, are ordered for Monday mornings. These typically include prealbumin, alkaline phosphatase, hemoglobin, and reticulocyte count. Occasionally, if the infant has severe osteopenia or malnutrition, assessment of Ca, Mg, Phos will be included. If the infant is on diuretics or TPN, a basic metabolic panel should be ordered. 6. By convention, we consider the birth date = day of life 1. 7. Drug dosing should be reported as mg/kg/day. 8. Intake should be reported as “XX” ml/kg/day and “XX” calories/kg/day. 9. Urine output should be reported as “XX” ml/kg/hr.