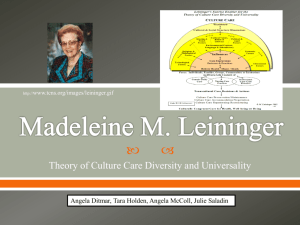
Cultural Healthcare: Leininger's Theory & Diversity
advertisement

CULTURAL HEALTHCARE 1 Cultural Healthcare Madeleine Leininger’s Culture Care Diversity and Universality Theory Kathie O’Dell Concordia University CULTURAL HEALTHCARE 2 Introduction Madeleine Leininger was born in 1925 in Sutton, Nebraska. She graduated from a Diploma Nursing program at St. Anthony’s School of Nursing in Denver, Colorado, and then went on to receive a Bachelor’s of biological science with a minor philosophy in Atchison, Kansas. She worked as an instructor, staff nurse, and head nurse in medical surgical unit, until she opened a new psychiatric unit and was the director of nursing at St. Joseph’s Hospital in Omaha, NE. Her background in child psychology helped her to realize that there was a lack of understanding among staff related to cultural factors. She noted differences in responses to treatment from children who had different cultural backgrounds. She return to school to study these differences and received a doctorate from the University of Washington, and began teaching the first ever course of transcultural nursing at the University of Colorado in 1966. Leininger’s theory is a product of 40 years of research, during which she studied 54 cultures and identified 172 care constructs for the use by nursing professionals (Zoucha and Husted, 2000). Madeleine Leininger’s Culture Care Diversity and Universality Theory is an area of study and practice that focuses on values, beliefs, and practices of individuals or groups that promote health and well-being. Culture is those behavior patterns that are socially acquired and transmitted by means of such symbols as customs, techniques, beliefs, institutions, and material objects (Zoucha and Husted, 2000). Cultural congruence and cultural imposition concepts were also described by Leininger. Cultural imposition is when a nurse imposes her own beliefs and values upon another culture because she believes it to be more superior to the patients. Cultural congruence is the care that is provided to the patient that is beneficial, CULTURAL HEALTHCARE 3 satisfying, and meaningful. Leininger’s goal was to make the patient the subject of care focusing on whom that person really is and how do they live, think, and feel. Analysis Madeleine Leininger did not start off in the nursing profession. She was a third grade school teacher in an elementary school in Nebraska. She however had a desire to continue that human caring to another level. During World War II she began her nursing career. She continued her nursing education obtaining a bachelor of science, master of science in psychiatric nursing, and was employed at the University of Cincinnati where she met Dr. Margaret Mead a visiting professor. Madeleine worked as a child guidance nurse where she began to observe the children of diverse cultural backgrounds responded differently to care and psychiatric treatments (Ray, 2012). After sharing her observation with Dr. Mead, she began examining the interrelationships between nursing and anthropology. She returned then to the classroom to pursue a doctorate of philosophy in anthropology focusing on cultural, social, and psychological content. During her doctorate study she went to New Guinea and studied the indigenous people of Gadsup. While studying the caring phenomena with the Gadsup people she could see the need for cultural care as a discipline of nursing study. There are three modalities that guide nursing judgments, decision, and actions according to Leininger. Masters (2012) states these as “cultural care preservation and /or maintenance, cultural care accommodation and/or negotiation, and cultural care repatterning or restructuring”. Leininger describes the patient as a person who is a human being, family, group, community or even and institution. These persons could be a product of an event like CULTURAL HEALTHCARE 4 those who experienced the destruction of the twin towers or be part of an isolated community like the Amish. They are defined by their social interactions in physical, ecological, sociopolitical, and cultural settings. There can be social boundaries that affect a particular patient for example, comforting touch, the French patient see it as a social norm where as a China patient sees it as a social taboo. Each cultural group outlines health as a state of wellbeing that is culturally defined, valued, and practiced. Nursing these individuals or groups must be congruent with their cultural values, beliefs, and life ways. Identifying these with a patient and their families will help initiate care that is supporting and patient centered. There are thirteen major assumptions that support Leininger’s theory of cultural care diversity and university. She begins with care being the essence of nursing, and then she reveals that cultural based care is essential for well-being, health, growth, and survival. Thirdly she states that culturally based care is a holistic means to guide a nurse’s decisions and actions, with then the next step being transcultural care with a central purpose of serving individuals, groups, communities, societies, and institutions. On the fifth assumption this statement appears, there can be no curing without caring, but caring can exist without curing. Varying concepts, meanings, expressions, patterns, processes, and structural forms of care make up number six, and the seventh is that every human culture has generic care knowledge and practices. By the eighth assumption we are acknowledging that care values, beliefs, and practices are influenced by worldview, language, philosophy, religion, kinship, social, political, legal, educational, economic, technological, environmental context of cultures. So now we know that for care to beneficial, healthy, and satisfying it needs to be culturally based. The tenth assumption is finding out knowing and using that knowledge for culturally congruent care CULTURAL HEALTHCARE 5 that is appropriate and safe. Worldwide culture care can differ and have similarities, and in the twelfth assumption cultural conflicts and impositions, stresses, reflect a lack of cultural care knowledge. Finally the thirteenth is the ethnonursing qualitative research method provides an important means to discover the diverse culture care data (Masters, 2012). We as a society continue to migrate and evolve, our cultural differences are also changing and as nurses our knowledge is challenged, seeking information becomes essential. Internet and social media are a new element to cultural understanding and plays a role in the new generation of patients. As nurses we need to consider many different aspects of our patients and their histories. Learning the history of the area that you work in is beneficial, but keeping up on current events and trends is crucial. Acquiring a skill in asking the right question can be a good tool to learn. Some individuals will not be able to share their needs, learning how to ask the right questions and learning our patient’s cultural diversity will be an art worth learning. Leininger (1996) stated in an interview “today, in a typical urban hospital, many nurses care for patients from as many as 20 different cultures. The diversity among cultures will continue to increase”. We as nurses need to consider our patient population and what cultures we have in our area. Not growing up in the area that you serve may have some challenges when you are learning patient backgrounds or histories. You may not know that they are of an ethnic decent that refuses to bath daily or that direct eye contact is considered being dominating to that patient. To be culturally congruent you would need to do some research of your area or that particular patient. We are living in society that is mobile. Having quick resources is CULTURAL HEALTHCARE 6 essential. Interpreters or access to phones that provide that service can mean the difference in patient care and outcomes. Malinowski and Stamler (2002) describes using the ethnonurse method and identified that “Philippine nurses value patients' physical comfort as an important aspect of nursing care. Securing comfort for their patients is a means of developing relationships”. This would be an expected part of nursing practice in the Philippines. Identifying patient needs and background is part of the nursing process of obtaining health history information. We as nurses need to ask is there any cultural practices you would like us to observe while you are in the hospital. The patient may not be able to list these at the time but by learning likes and dislikes is helpful in providing for their needs. This patient likes the room warm or needs to eat fish on Fridays is an example of following cultural practices. Discussion In our short time we have seen current events that have changed our world leading to population changes. We see foreign refugees seeking sanctuary from their oppressors or illegal immigrants seeking jobs. Each comes with their own stories, fears, and experiences. Seeking health care alone can be a stressful experience as not all countries have health care facilities like the United States. Sometimes just getting past the language barrier can be a struggle. As nurses we need to be prepared to care for these challenges. Having interpreters or access to multilingual teaching sheets and admission paper work is essential. Keeping an open mind about cultures that practice things we are not use to like circumcisions on females, or family dynamics where you can only talk to the patient’s husband. Not all practices are healthy. CULTURAL HEALTHCARE 7 Understanding some biological backgrounds can be as helpful as well, for instance there is a higher prevalence of hypertension and sickle cell anemia in black people. Working in healthcare you begin to see several interesting cultural practices and prevalence. Taking all those experiences and expanding on them will assist you with adjusting to a new cultural practice that you haven’t seen before. Don’t ever assume because an individual maybe Native American they practice all the cultural aspects of that background. Rajan (1995) states “one must develop an awareness of different cultures while keeping in mind individual differences”. You will not know this unless you ask. There is also a need to keep current on the new trends that are happening in your area or in the world. One current trend of piercing different parts of your body may cause some embarrassment when prepping a patient for surgery. Working in outpatient surgery you can see this frequently. By accepting this trend and being prepared for it makes the patient more comfortable about receiving nursing care and health care in general. Our outpatient services have learned to have a cup with a lid ready at bedside, for the keeping of the appliance, until surgery is over. However we do make a point to have them have a designated person to replace the appliance when they return from surgery. We do incorporate in the discharge teaching with the patient about caring for such areas, watching for infection, and when to seek medical care as to promote a healthy lifestyle. We are also caring for a large older population that grew up in the 1930’s and 40’s these are post war veterans and have a lot to share but also come with interesting health promotion ideas. We were surprised by a request while caring for a gentleman who said he needed to CULTURAL HEALTHCARE 8 eat 1 small piece of garlic each day to stave off respiratory infections. He was given garlic every morning with his breakfast. This was important to him and in doing so he felt comfortable in taking his other medication from us and respected the teaching we gave to him. Doing a thorough health assessment is critical to patient care. Knowing what is important to this patient and how they have cared for themselves in the past may alter or add to their plan of care while in the health care setting. Rajan (1995) states, “the person is a cultural being who cannot be viewed apart from his or her cultural background”. It is important to add in your health policy for admission this statement: Are there any cultural practices you would like us to observe while you are in the hospital? Conclusion Madeleine Leininger’s Culture Care Diversity and Universality Theory was a long term goal for her. She worked 30 years to fulfill an obvious need for patient and human care that was culturally congruent. Through her observations we are able to conduct incisive medical histories that include the diverse backgrounds that our patients generate from. With this background knowledge our healthcare systems can treat patients with the values, beliefs, and practices that are their own, promoting well-being in meaningful ways. As our patients evolve so do their cultural experiences, it could be an event, childhood upbringing, a community they live in, or a country they have come from. All of these experiences have an influence on their daily needs and beliefs and this in turn governs the health care they seek and the expectations of the nursing care they receive. CULTURAL HEALTHCARE 9 Reference List Leininger, M. (1996) Transcultural nursing: essential for excellence interview Madeleine Leininger. (1996). Nursing, 26(1), 76 Masters, K. (2012). Nursing Theories: a framework for professional practice. (pp. 213) Sadbury, MA: Jones and Bartlett Learning Malinowski, A., & Stamler, L. (2002). Comfort: exploration of the concept in nursing. Journal Of Advanced Nursing, 39(6), 599-606. doi:10.1046/j.1365-2648.2002.02329.x Rajan, M. (1995). Transcultural nursing: a perspective derived from Jean-Paul Sartre. Journal Of Advanced Nursing, 22(3), 450-455. doi:10.1046/j.1365-2648.1995.22030450.x Ray, M. (2012). Remembering Madeleine M. Leininger, PhD, LHD, DS, RN, CTN, FAAN, FRCNA, 1925-2012. International Journal For Human Caring, 16(4), 6-8. Zoucha, R., & Husted, G. (2000). The ethical dimensions of delivering culturally congruent nursing and health care. Issues In Mental Health Nursing, 21(3), 325-340. .