APAPAPER
advertisement

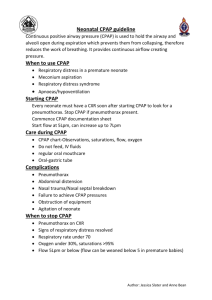
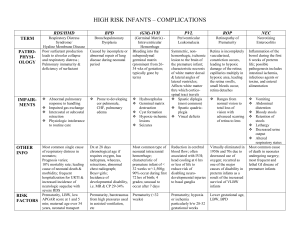
Running Head: CPAP IMPROVES THE LONG-TERM OUTCOME OF PREMATURE INFANTS CPAP Improves the Long-term Outcome of Premature Infants Kiel Bisceglia Concorde Career College English Composition 2 CPAP IMPROVES THE LONG-TERM OUTCOME OF PREMATURE INFANTS 2 Every year 500,000 infants are born prematurely, according to the Center for Disease Control (CDC). That means that one out of every nine births is premature; the CDC considers a birth premature when it occurs at least three weeks prior to full gestational age of 40 weeks. These infants endure a lifetime of problems including: mental disabilities, vision problems, cerebral palsy, digestion and nutrition issues, hearing loss, and respiratory problems. While many of these issues cannot be prevented, recent studies have shown that alternative management of respiratory distress in these premature infants can improve the long-term respiratory outcomes. Of the many therapies in common practice, non-invasive Continuous Positive Airway Pressure (CPAP) is showing great promise in reducing the occurrence of chronic lung disease and other respiratory ailments. CPAP combined with other therapies is proving to be low cost and more effective than traditional mechanical ventilator and prophylactic surfactant protocol. This paper will discuss the respiratory challenges facing premature infants and the standard protocol for these infants. It will then discuss CPAP therapy, including bubble CPAP and ventilator CPAP, and how it is improving long term clinical outcomes of these patients and reducing the associated costs. Respiratory distress is common in premature infants born before the gestational age of 28 weeks. This is due to underdeveloped lungs. Not only do the lungs lack the structure to operate properly, but they also have inadequate amounts of surfactant. Surfactant is a slippery substance that lines the alveoli in the lungs. It keeps the lung tissue stiff and prevents it from collapsing and sticking together. According to the National Institute of Health (2011), symptoms of respiratory distress in newborns can usually be seen within minutes of birth, although it may not be detected until several hours afterward. Symptoms include: bluish color of skin, breaks in regular breathing, grunting, rapid CPAP IMPROVES THE LONG-TERM OUTCOME OF PREMATURE INFANTS 3 breathing, nasal flaring, and decreased urine output. Infants with severe respiratory distress syndrome will often die within seven days. For those infants that survive, the type of respiratory management protocol they receive will generally determine their short and long-term outcome. Many of these infants will suffer from a chronic lung disease, most commonly bronchopulmonary dysplasia (BPD). BDP is defined in infants as the need for increased oxygen inspiration at 28 days or greater post birth. The lungs of an infant with BPD are often scarred and show inflammation. The standard method of care in these cases is mechanical ventilation and prophylactic surfactant (MVPS) with high volume of inspired oxygen (Bahman-Bijari , Malekiyan, Niknafs & Baneshi, 2011). Mechanical ventilation involves inserting an endotracheal tube into the infant’s lungs, which allows the ventilator to do the breathing for the infant. Today’s modern neonatal ventilators are specially designed to apply a high volume of inspired oxygen and pressure to the lungs. However, as the machine does the breathing for the infant, his or her lungs do not have enough surfactant to keep the alveoli fully inflated. As the alveoli collapse, the surfactant can get squeezed out of the alveolar sacs, which can potentially cause a full collapse. Therefore, it is necessary to supplement the lost surfactant, also called prophylactic surfactant. This is done by injecting the surfactant through the endotracheal tube into the lungs. This mechanical ventilation in combination the prophylactic surfactant is seen as a life saving procedure for many premature infants in respiratory distress. This has been the preferred protocol for neonatal respiratory distress, although there is much scientific data that shows negative side effects of the treatment. While MVPS can be lifesaving, the side effects and negative outcomes are numerous. Because this is an invasive procedure, it has inherent risks of damage to the lungs. The CPAP IMPROVES THE LONG-TERM OUTCOME OF PREMATURE INFANTS 4 damage it can cause often leads to the scarring and inflammation seen in patients with chronic lung disease. There is also a risk of ventilator-associated pneumonia. Atrophy of the diaphragm and cardiac output can also occur because the machine is doing the work for the infant. Furthermore, there is a major risk for oxygen toxicity, which is another major factor in chronic lung disease. In spite of these major drawbacks, MVPS has been commonly used for over 30 years. However, over the last ten years greater attention and studies have been directed toward noninvasive CPAP. Continuous Positive Airway Pressure, or CPAP, is a method of ventilation that supplies a continuous flow of oxygen into the patient’s respiratory system. This flow of oxygen maintains the integrity of the airway and keeps the alveolar sacs inflated in the absence of the proper amount of surfactant. CPAP was first introduced in 1971. It was shown that applying CPAP using an anesthesia bag could improve the oxygenation of an infant in respiratory distress (Polin, 2009). Although it was simple and low-cost, CPAP took a sideline to more advanced technology present in sophisticated and pricey new mechanical ventilators (Polin, 2009). Over the next couple of decades, after the first CPAP was administered via the anesthesia bag, there were a few other methods of delivery introduced: the face mask, the head box with neck seal, and the negative pressure box. The face mask fit completely around the nose and mouth of the infant. It was seen as beneficial because there was no loss of pressure through the infant’s mouth, and it was given to the infant right after birth. There were, however, a few long-term problems: the seal around the face was difficult to achieve without significant pressure on the face, when the mouth and nose needed to be suctioned the mask had to be removed and pressure was lost, and the seal could not be CPAP IMPROVES THE LONG-TERM OUTCOME OF PREMATURE INFANTS 5 formed when a feeding tube was inserted (Morley, 2012). The head box with neck seal was a box that fully enclosed the head and sealed around the neck. There were pop off valves that controlled the pressure in the box. There were several problems associated with this method including: difficulty with getting a seal around the neck, very limited access tothe infant’s face, a high flow of cooling gas around the baby’s face, and it was very noisy (Morley, 2012). The negative pressure box enclosed the baby’s thoracic cavity in a pressure controlled box. The box maintained a negative pressure so that the chest and lungs would not collapse. The issues with this system included: difficulty in getting a good seal, poor access to the baby’s body, and the body being surrounded in a cooling gas. None of these devices are in common use anymore (Morley, 2012). There are currently five methods of delivery being used due to their ease of use and lack of complications: short bi-nasal prongs, single nasal prong, long nasopharyngeal prongs, nasal mask, and endotracheal tube (Morley, 2012). Short bi-nasal prongs are inserted into the nostrils and are considered more effective than a single nasal prong. Both single nasal prongs and nasopharyngeal prongs show a higher resistance than bi-nasal prongs. The nasal mask can be effective, but it requires undue pressure to get a proper seal around the baby’s face and can cause damage to the nasal bridge. The endotracheal tube should not be used as a primary CPAP delivery system. It should only be used just before extubation to determine if the baby is capable of breathing on his or her own (Morley, 2012). Due to the noninvasive delivery methods available for CPAP, there has been renewed interest in this technique for respiratory management of premature infants. A study published in Pediatric Digest explored the benefits of the benefits of CPAP over traditional MVPS. The study was conducted at a tertiary level neonatal intensive care CPAP IMPROVES THE LONG-TERM OUTCOME OF PREMATURE INFANTS unit (NICU). While the hospital had been seeing significant survival rates of low weight, preterm babies, they were also seeing an increase in the number of cases of chronic lung disease in these infants. The significant increase occurred between the years of 1997 and 2002. At that time the standard method of respiratory management was MVPS. The hospital wanted to see if they could get better clinical outcomes if they used alternative respiratory management methods. They used two cohorts to conduct the study; the first cohort included premature infants born in 2002 that were managed with MVPS, and the second cohort included premature infants born in 2005 managed with an improved respiratory management protocol, which included CPAP. The study showed that while there was no significant reduction of short-term NICU outcomes, there was a significant decrease in occurrence of chronic lung disease. In the 2002 cohort, 46.5% of the infants developed chronic lung disease, while the 2005 cohort only 20.5% developed the disease. That is a 55.8% reduction. The study recognized the significance of an original hypothesis that mechanical ventilation can lead to oxygen toxicity, a probable cause of chronic lung disease. The study also pointed out that with use of CPAP there was an improved functional residual lung capacity, improved ventilation and oxygen perfusion, and a reduction in lung volutrauma, which occurs when the lungs are expanded beyond their capacity. Further, there was a reduction of ventilator-associated pneumonia (Birenbaum, et. al., 2009). This is among many studies that have shown improved clinical outcomes for infants who are placed on noninvasive CPAP respiratory management. While it seems clear that better outcomes can be secured by the use of CPAP, many questions remain as to which method of CPAP is best. There are several methods of providing CPAP, but ventilator-CPAP (vCPAP) and bubble-CPAP (bCPAP) are the most 6 CPAP IMPROVES THE LONG-TERM OUTCOME OF PREMATURE INFANTS 7 commonly used (Bahman-Bijari, et al, 2011). Each device works on the same principle, but have different pressure sources. VCPAP uses a traditional ventilator to generate the nasal CPAP, and a valve is used to adjust resistance to the flow of air. The bCPAP, however, uses the distal end of the exhalation tube immersed in a column of water to create a pressure gradient. As the tube is immersed deeper into the water, the pressure gradient increases (Bahman-Bijari, et al, 2011). There is little clinical data regarding the efficacy of either method, but preliminary studies have shown better outcomes from bCPAP. One such study was conducted at the level III neonatal care unit at Afzalipoor Hospital in Iran. The study was conducted between the years of 2009 and 2010. There were a total of 50 preterm infants involved. Twenty five of the infants received bCPAP, and 25 received vCPAP. Of the 25 infants in the bCPAP group, only one infant had respiratory failure during treatment requiring mechanical ventilation. Meanwhile, seven infants in the vCPAP experienced respiratory failure during treatment. Further, the study showed a reduction in the mean duration of treatment; the bCPAP group had a mean duration of 35.5 hours, and the vCPAP group had a mean duration of 57.5 hours. Also significant was a reduction of the mean duration of hospitial stay from 11.9 days in the vCPAP group to 8.7 days in the bCPAP group (Bahman-Bijari, et. al., 2011). The improved outcome from bCPAP may be due to the oscillatory vibrations created by the bubbles. These vibrations create a similar effect that is produced by high-frequency ventilation(HFV) (Bahman-Bijari, et. al., 2011). HFV delivers a higher than normal ventilator frequency, usually four times greater than normal, with low tidal volume. It is thought to reduce barotrauma to the lungs (Sykes, 1985). Therefore, bCPAP may have the same effects as CPAP and HFV being administered at the same time. Reports have shown CPAP IMPROVES THE LONG-TERM OUTCOME OF PREMATURE INFANTS 8 that combining these therapies improves hemodynamics of the preterm infants (BahmanBijari, et. al., 2011). There have been very few large-scale clinical studies of bCPAP, so the efficacy and future uses of the therapy are still not fully known. While the data regarding bCPAP is encouraging, there is not enough definitive data proving that it is the best mode of treatment. There have been no large randomized trials of the therapy because it is still not known what the optimal treatment protocol is with bCPAP. Doing a large trial at this stage would be far too risky (Bahman-Bijari, et. al., 2011). What is clear, however, is bCPAP and vCPAP can significantly lower the costs associated with preterm births. A study conducted in California and New York showed the costs of mechanical ventilation and after care of preterm infants costs a total of $4.4 billion annually. These costs do not include the high post discharge costs of continued oxygen therapies and readmission to the hospital, nor do they include the $5.8 billion spent on asthma care (Angus, Linde-Zwirble, Clermont, Griffin, Clark 2001). The cost of care is in direct relation with the time spent in the NICU and the hospital stay. Studies have shown that CPAP can significantly reduce the time spent on ventilators, as well as the overall stay in the hospital. If an infant can spend less time in the hospital, the costs associated with care go down. The reduction in cases of bronchopulmonary dysplasia will also reduce costs associated with aftercare of these preterm infants. Not only can CPAP treatments provide cost savings in developed countries, they can be essential in providing life support in low-resource settings. Low–resource settings in the underdeveloped world do not have access to basic life saving equipment, such as ventilators. Complications from respiratory issues account for 30% of infant mortality in these countries (Brown, et. al., 2013). A portable bCPAP machine was developed and tested in low-resource hospital in Malawi, Africa with encouraging CPAP IMPROVES THE LONG-TERM OUTCOME OF PREMATURE INFANTS 9 results. The study looked at the results of a $350 bCPAP device compared with a $6000 device used in developed countries. The study concluded that the low cost bCPAP devices performed just as well as the more expensive devices. The low cost devices were tested on 100 infants and children with no adverse effects. While the low cost bCPAP device does not have all the features compared with its more expensive counterpart, it proved to be a life saving and affordable treatment for infants who would normally not have access to mechanical ventilators or more expensive CPAP equipment (Brown, et. al., 2013). Although CPAP has been used as a treatment for over 40 years, it is only through the last decade that interest has been renewed in this non-invasive treatment. While early nasal CPAP does not significantly reduce the rate of death from respiratory distress, it is clear from the research and studies that CPAP can improve the long-term outcome of premature infants with respiratory problems (Morley 2008). BCPAP is of particular interest right now as it is a low cost and high value method of delivering CPAP. More research needs to be done with respect to the proper treatment protocols, but it is clear that the future outcome of respiratory distress in preterm infants can be greatly improved with the use of CPAP. CPAP IMPROVES THE LONG-TERM OUTCOME OF PREMATURE INFANTS 10 References Angus, D., Linde-Zwirble, W., Clermont, G., Griffin, M., Clark, R. (2001) Epidemiology of neonatal respiratory failure in the United States. American Journal of Respiratory and Critical Care Medicine, 164(7), 1154-60. Bahman-Bijari , B., Malekiyan, A., Niknafs, P., & Baneshi, M. (2011) Bubble-cpap vs. ventilator-cpap in preterm infants with respiratory distress. Iranian Journal of Pediatrics, 21(2), 151-158. Birenbaum, H., Dentry, A., Cirelli, J., Helou, S., Pane, M., Starr, K., Melick, C., & Upedegraff, L.,… (2009) Reduction in the incidence of chronic lung disease in very low birth weight infants: Results of quality improvement process in a tertiary level neonatal intensive care unit. Pediatrics Digest, 123(1), 44-50. Brown, J., Machen, H., Kawaza, K., Mwanza, Z., Iniguez, S., Lang, H., Gest, A., & Kennedy, N. (2013) A high-value, low-cost bubble continuous positive airwaypressure system for low-resource settings: Technical assessment and initial case reports. PLOS One, 8(1), 16. Morley, C., (2012). Manual of neonatal respiratory care. (3rd ed., pp. 237-245). New York, NY: Springer Science business Media. Morley, C. (2008) Nasal CPAP or intubation at birth for very preterm infants. The New England Journal of Medicine, (358), 700-708 Polin, R. (2009) Bubble cpap: A clash of science, culture and religion. The Journal of Pediatrics, (154), 633-634. Sykes, M. (1985). High frequency ventilation. Thorax: An International Journal of Respiratory Medicine, 40(3), 161-165