Path Chapter 10 p448-462[4-20
advertisement

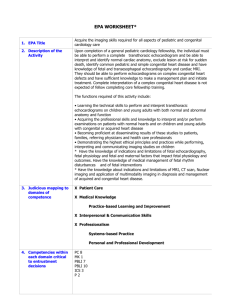
Path Chapter 10: Diseases of Infancy and Childhood (pages 448-462) Congenital anomalies – morphologic defects preset at birth - Some may not become apparent until years later Congenital – means born with 1 in 33 babies are born with a birth defect each year, and they’re the most common cause of death in the first year of life Malformation – primary errors of morphogenesis, where there is intrinsically abnormal development - Usually associated with multiple gene loci, called multifactorial Disruptions – happen from secondary destruction of an organ or body area that had previously developed normally - So unlike malformations, disruptions come from extrinsic disturbance in morphogenesis A classic example of disruption are amniotic bands, which are evidence of rupture of the amnion, which forms bands that encircle, compress, or attach to parts of the developing fetus Disruptions are not hereditary, so there’s no worry of passing it on to kids Deformations – extrinsic disturbance of development from localized or generalized compression of the fetus by abnormal biomechanical forces, leading to structural abnormalities - Deformations are common, and happen in 2% of newborns The most common cause of a deformation is uterine constraint o At the 35-38th weeks, the body size increases rapidly and in this case faster than the growth of the uterus o Also, the amount of amniotic fluid, which usually acts as a cushion, decreases o Even normal fetuses face a little bit of uterine constraint o Things that increase risk for constraint: Mom things – first pregnancy, small uterus, malformed (bicornuate) uterus, and leiomyomas Fetal things – oligohydramnios, multiple fetuses, & abnormal fetal presentation o Ex of deformation: clubfeet from oligohydramnios Sequence – several problems triggered by one original problem - Half the time, there’s just one congenital anomaly, & the rest has multiple congenital anomalies Sometimes, the group of problems are explained by a localized problem in organogenesis, like a malformation, disruption, or deformation, that then causes secondary effects o Ex: oligohydramnos (aka Potter sequence) – decreased amniotic fluid Can be caused by chronic leak of amniotic fluid from rupture of the amnion, uteroplacental insufficiency from mom hypertension or severe toxemia, and renal agenesis since fetal urine is the main part of amniotic fluid Fetal compression from olighydramnios causes a classic phenotype in the newborn of flattened face and abnormalities of the hands and feet The hips may be dislocated, and the lungs are usually hypoplastic from decreased growth of the chest wall and lungs Nodules in the amnion, called amnion nodosum, are common Syndrome – group of problems believed to be related, but can’t be explained by a single original initiating defect - Syndromes are most often caused by a single cause, like a virus or chromosome problem, that then affects several tissues Agenesis – complete absence of an organ and its associated primordium (so the parts to make it never showed up) Aplasia – absence of an organ from failure of development of the primodium (so the parts to make it didn’t get the job done) Atresia – absence of an opening Hypoplasia – incomplete development or decreased size of an organ, or decreased size of the organ with decreased #’s of cells Hyperplasia – enlargement of an organ or tissue from an increased #’s of cells Hypertrophy/hypotrophy – the organ enlarges or shrinks because individual cells enlarge or shrink, and don’t change in # Dysplasia – abnormal organization of cells The exact cause of a congenital anomaly is unknown in at least half-3/4 of cases – table page 450 Common known causes can be genetic, environmental, or multifactorial Genetic causes of anomalies – can be from chromosome problems, from single-gene mutations (“mendelian disorders”), or from multifactorial inheritance (2 or more genes interact with environmental factors) - - Up to 15% of live births have chromosome problems on karyotype, but only trisomy 21 (Down syndrome) is not rare – table page 451 o Most of these are caused by problems in gametogenesis, so they’re not familial o Rarely though, some can be passed on to kids Ex: Down syndrome from a Robertsonian translocation in the parent o 80-90% of fetuses with aneuploidy or other chromosome problems, die in utero, usually early in gestation 90% of the single gene mutations are inherited in an autosomal dominant or recessive way o o o So most of these mutations cause loss of function of genes involved in normal organogenesis and development, to cause a birth defect Ex: holopresencephaly is the most common developmental defect of the forebrain and midface Hedgehog signaling is important in morphogenesis of this stuff, so loss of function of the pathway happens in families that show holoprosencephaly Ex: achondroplasia – most common form of short-limb dwarfism Caused by gain-of-function mutation in fibroblast growth factor receptor 3 (FGFR3), whose protein is a negative regulator of bone growth, so activating it causes dwarfism Environmental stuff, like viruses, drugs, and radiation during pregnancy, can cause fetal malformations (technically disruptions) - - Rubella, CMV, herpes, varicella-zoster, flu, mumps, HIV, & enterovirus can cause malformations o The gestational age at time of infection is important Rubella is a hazard from just before conception to the 16th week, and more in the first 8 weeks Risk for malformation goes from half to 1/5 to 7% in each of the first 3 months Rubella malformations include cataracts, heart problems, deafness, and mental retardation, all together called congenital rubella syndrome o Intrauterine infection with CMV is mostly asymptomatic, and the most common fetal viral infection, and you’re most at risk in the second trimester Most organogenesis is done by the end of the first trimester, so congenital malformation don’t happen as often in rubella But when malformations do happen, they’re often severe, and usually involve the CNS to cause mental retardation, microcephaly, deafness, and hepatosplenomegaly Less than a % of congenital anomalies are caused by drugs or chemicals o Includes thalidomide, folate antagonists, androgenic hormones, alcohol, anticonvulsants, warfarin, acutane (13-cis-retinoic acid) o Thalidomide – causes limb abnormailities in most exposed fetuses Thalidomide downregulates WNT signaling in development Thalidomide is used for cancer o Alcohol – causes fetal alcohol syndrome The most severely affected fetuses have stunted growth, microcephaly, atrial septal defect, short palpebral fissures, and maxillary hypoplasia Alcohol messes up developmental pathways for retinoic acid and hedgehog o Cigarrete smoking causes lots of spontaneous abortions, premature labor, and placenta problems during pregnancy, and low birth weight and prone to sudden infant death syndrome (SIDS) - - Radiation is mutagenic, carcinogenic,a dn teratogenic o Exposure to high doses of radiation during organogenesis leads to malformation, like microcephaly, blindness, skull defects, and spina bifida Diabetes in mom during pregnancy causes malformations in up to 1/10 of cases o Mom’s hyperglycemia causes fetal hyperinsulinemia, causing increased body fat, muscle mass, and organomegaly, together called fetal macrosomia; as well as heart problems, neuroal tube defects, and other CNS stuff Multifactorial congenital anomalies happen from inheritance of multiple genetic polymorphisms that cause a “susceptibility phenotype” - This underyling phenotype then interacts with the environment, allowing the disorder to manifest Ex: congenital dislocation of the hip – you’re born with a shallow hip socket and lax ligaments, which then lead to dislocation when you flex the hip (environmental factor) The timing of the prenatal teratogenic insult is important for the occurrence and type of anamoly that happens – page 453 – table of stages of development and effect of teratogens - Development in the uterus has 2 phases: o Embryonic period – first 9 weeks of pregnancy Early embryonic period – first 3 weeks after fertilization Teratogens either injure enough cells to cause death or abortion, or it doesn’t hurt enough cells, and the embryo recovers with no problems Weeks 3-9 – the embryo is EXTREMELY susceptible to teratogenesis The peak period is between the 4th and 5th weeks This is the period organs are being “crafted” out of germ layers o Fetal period – follows organogenesis, and lasts up till birth In the fetal period, there is mainly growth and maturation of the organs Less susceptible to teratogens at this time Instead, during the fetal period the fetus is susceptible to growth retardation or injury to already formed organs o So an agent can cause different anomalies depending on when exposure is Cyclopamine - teratogen that inhibits hedgehod signaling, causing craniofacial problems like holoprosencephaly and “cyclopia” (single fused eye) Valproic acid – anti-epileptic drug, that is a teratogen during pregnancy - Valproic acid disrupts expression of homeobox (HOX) transcription factors HOX proteins work in patterning of limbs, vertebrae, and craniofacial structures All-trans-retinoic acid – vitamin A (retinol) derivative needed for normal development & differentiation - If it’s absent during embryogenesis, it affects the eyes, GU, cardiovascular, diaphragm, and lungs - So you have problems with them when mom has vitamin A deficiency Excess exposure to retinoic acid is also teratogenic o Retinoic acid is used for severe acne, and it causes retinoic acid embryopathy, which shows CNS, cardiac, and craniofacial problems, like cleft lip and cleft palate Babies born before completion of the normal gestation period or who have failed to grow normally, have higher morbidity and mortality rates than full-term infants - - If you’re born early, you’re more at risk for problems from organ immaturity, especially respiratory distress syndrome (RDS) Infants are classified by birth weight: o Appropriate for gestational age – birth weight in the 10th-90th percentile o Small for gestation age – below 10th percentile o Large for gestational age – above 90th percentile Infants born before 37 weeks are considered preterm, and those after 42 weeks are post-term Causes of prematurity and fetal growth restriction: - - Prematurity – gestational age less than 37 weeks o It’s the 2nd most common cause of neonatal death, behind congenital anomalies o 12% of all births are preterm Major risk factors for prematurity: o Preterm premature rupture of placental membranes (PPROM) – spontaneous rupture of membranes before 37 weeks gestation Happens in 3% of all pregnancies, and causes up to 1/3 of all preterm deliveries Rupture of membranes before labor can be spontaneous or induced Rupture after 37 weeks has less risk Risk factors for premature rupture of the placenta include history of preterm delivery, vaginal bleeding during the current pregnancy, mom smoking, being poor, and poor mom nutrition Mutations to genes in immune regulation, like TNF, or collagen breakdown, like matrix metalloproteinases, can cause PPROM Makes sense because PPROM often involves inflammation of the placenta and collagen breakdown by MMP’s Second trimester PPROM has an awful prognosis o Intrauterine infection – the major cause of preterm labor Happens in up to a ¼ of all preterm births, and the earlier the gestational age at delivery, the higher the frequency of intra-amniotic infections Intrauterine infection shows inflammation of the placental membranes (called chorioamnionitis) and inflammation of the fetal umbilical cord (funisitis) The most common infectious agent to cause preterm labor are ureaplasma urealyticum, mycoplasma hominis, gardnerella vaginalis (main cause of bacterial vaginosis), trichomonas, gonorrhea, and chlamydia - - In developing countries, malaria and HIV can cause preterm labor TLR4 activation is a main player in preterm infection, and may lead to smooth muscle contractions o Uterine, cervical, and placental structural abnormalities can cause prematurity Includes uterine distortion (like in uterine fibroids), loss of structural support of the cervix (called cervical incompetence), placenta previa and abruptio placenta o Multiple gestation (twins) can be a risk factor for prematurity Problems the newborn may have include sepsis, hyaline membrane disease (aka neonatal respiratory distress syndrome), necrotizing enterocolitis, intraventricular hemorrhage, or longterm stuff like developmental delay Premature babies are small, but their size often fits the gestational age Full term babies that are small often had fetal growth restriction (FGR, aka intrauterine growth retardation) o Can be detected by ultrasound before birth o Fetal things that can cause FGR are things that prevented growth, even though the fetus was getting enough nutrients from mom Includes chromosomal disorders, congenital anomalies, and congenital infections Chromosome problems include triploidy (most common cause), trisomies, deletions, and translocations Fetal infection should be considered in all cases of FGR Infections most commonly responsible for FGR are the TORCH group: o TOxoplasmosis, Rubella, CMV, Herpesvirus) FGR from fetal causes usually shows symmetric growth restriction (aka proportionate FGR) o Placental causes of FGR: During the 3rd trimester, intense fetal growth places a heavy demand on the uteroplacental supply line So uteroplacental insufficiency can lead to FGR Can happen from umbilical-placental vascular anomalies, placental abruption, placenta previa, placental thrombosis and infarction, placental infection, or multiple gestations Placental causes of FGR tend to cause asymmetric growth retardation, that spares the brain Placental FGR is messes up growth in the later half of gestation because of decreased availability of nutrients or oxygen Genetic mosaicism of the placenta (confined placental mosaicism) causes FGR Chromosomal mosaicisms happen from genetic mutations happening after zygote formation (page 455 visual) Genetic mutations at the time of the 1st or 2nd postzygotic division, cause generalized constitutional mosaicism of the fetus and placenta o o If the mutations happens later in dividing trophoblast or progenitors of the inner cell mass (happens most of the time), you get a genetic abnormality of only the placenta, causing confined placental mosaicism o Most often you see trisomies from this, especially trisomy 7 Maternal causes of FGR – the most common factor to cause a small for age infant Most often it’s a mom problem that causes decreased placental blood flow Often the underlying cause is preeclampsia or chronic hypertension Inherited thrombophilias, like factor 5 Leiden mutation can also cause FGR Avoidable mom things that can cause FGR are narcotic abuse, alcohol, and heavy cigarette smoking Drugs causing FGR include classic teratogens, like antimetabolites, and common drugs, like phenytoin (Dilantin) Mom malnutrition, especially prolonged hypoglycemia, can also affect fetal growth FGR often shows risk for handicap, cerebral problem, learning disability, or hearing or visual problems Neonatal respiratory distress syndrome (RDS): - - - - Causes of RDS in the newborn include excessive sedation fo the mom, fetal head injury during delivery, aspiration of blood or amniotic fluid, and intrauterine hypoxia from coiling of the umbilical cord around the neck The most common cause of RDS in the newborn is hyaline membrane disease, from deposition of a layer of hyaline protein-like material in the peripheral airspace of the infant Characteristics of RDS in the newborn: o The baby is almost always preterm but appropriate size for the gestational age o There is strong association with being male, mom diabetes, and C-section delivery o Usually within a few minutes after birth, the baby starts rhythmic breathing and gains normal color o After 30 minutes, breathing gets more difficult, and within a few hour you see cyanosis o At this point you can hear rales over both lungs o Chest x ray now will show small reticulogranular densities, causing a “ground-glass” picture o In full blown RDS, the respiratory distress persists, cyanosis increases, and even giving them oxygen doesn’t help o If you can keep them alive for 3-4 days, they have an excellent chance for recovery The most important part of RDS in the newborn is the lungs are immature o Can be seen in full-term babies, but is way more common in preterm The older the baby is (gestational age), the less likely it is to get RDS o Happens in over 1/2 before 28 weeks, 1/3 from 28-34 weeks, and less than 5% after 34 weeks The main problem in RDS is a deficiency of pulmonary surfactant o o - - Surfactant is made of mainly lecithin, with some phosphatidylglycerol and proteins Proteins include SP-A and SP-D (hydrophilic, and they work in innate immunity) and SP-B and SP-C (hydrophobic, and decrease surface tension in alveoli) o With decreased surface tension in the alveoli, there’s less pressure needed to keep the alveoli open and therefore filled with air o Surfactant is made by type 2 alveolar cells, and this speeds up in the 35th week of gestation o At birth, the first breath of life requires high inspiratory pressures to expand the lungs With normal levels of surfactant, the lungs retain up to 40% of residual air volume after the first breath, so following breaths require way less inspiratory pressures With decreased surfactant, the lungs collapse after the first breath, and with each following breath, so the baby has to work just as hard with each following breath as they did with the first o This problem of stiff atelectatic lungs is made worse by the soft thoracic wall that is pulled in as the diaphragm descends o Progressive atelectasis and decreased lung compliance lead to several events, resulting in a protein and fibrin-rich exudate into the alveolar spaces, with formation of hyaline membranes (page 457 – chart of events leading to this) These fibrin-hyaline membranes act as barriers to gas exchange, leading to carbon dioxide retention and hypoxemia The hypoxemia further impairs surfactant making, causing a vicious cycle o Surfactant making is regulated by cortisol, insulin, prolactin, thryoxine, and TGF-β Things that cause intrauterine stress and FGR that increase corticosteroid release will lower the risk of developing RDS High insulin suppresses surfactant release, like in mom diabetes, and will counteract the effect of steroids Labor increases surfactant making, so C-sections before onset of labor can increase risk for RDS In RDS of the newborn, the lungs are normal size, but solid, airless, and red/purple, and usually sink in water o Alveoli are poorly developed, and those that are there are collapsed o Eosinophilic hyaline membranes line the respiratory bronchioles, alveolar ducts and alveoli The membranes are made up of fibrin mixed with cell debris from necrotic type 2 pneumocytes o If they live 48 hours, you see reparative changes in the lungs To assess fetal lung maturity, you can look at amniotic fluid phospholipids, because pulmonary secretions are discharged into amniotic fluid Exogenous treatment with surfactant has made death by RDS of the newborn rare Oxygen therapy and surfactant are the treatment of choice after birth o Have to watch for oxygen toxicity, caused by free radicals from oxygen High concentrations of oxygen given for prolonged periods cause retrolental fibrplasia in the eyes, and bronchopulmonary dysplasia Retinopathy happens from expression of VEGF VEGF is strongly induced by hypoxia, and serves as a survival factor for endothelial cells and promotes angiogenesis During phase 1 hyperoxic phase of RDS therapy, VEGF is decreased, causing endothelial apoptosis (you have plenty of oxygen) VEGF then increases after return to hypoxic room air ventilation, causing retinal vessel proliferation (neovascularization/angiogenesis) characteristic of the lesions in the retina in phase 2 Bronchopulmonary dysplasia – caused by reversible impairment of the development of alveolar septation o Needs oxygen therapy for over 28 days of a baby with gestational age over 36 weeks o Shows airway epithelial hyperplasia, squamous metaplasia, alveolar wall thickening, fibrosis, less separation of alveoli that leads to large simple alveoli, and odd capillary arrangement o Things that cause BPD are hyperoxemia, hyperventilation, prematurity, inflammatory cytokines, and vascular maldevelopment o Oxygen can arrest septation of the lungs in the saccular stage of development o It also causes lots of proinflammatory cytokines, which can impair alveolar septation and arrest lung development o If you avoid oxygen poisioning, they usually recover after 3-4 days o BPD puts preterm infants even more at risk for preterm problems, like patent ductus arteriosus, intraventricular hemorrhage, and necrotizing enterocolitis Necrotizing enterocolitis – gut infection of newborn - - Most common in premature infants, and happens more the more preterm you are Happens in 1/10 of very low birth weight babies Most cases show enteral feeding, suggesting that some postnatal insult, like bacteria, start the cascade leading to tissue destruction Platelet activating factor (PAF) increases mucosal permeability by promoting enterocyte apoptosis and compromising intercellular tight junctions, making things worse o Kids with necrotizing enterocolitis will have higher PAF levels Breakdown of mucosal barrier function allows gut bacteria to get into the tissues, causing a vicious cycle of inflammation, mucosal necrosis, and more bacteria entry, eventually resulting in sepsis and shock - - Shows onset of bloody stools, abdominal distention, and circulatory collapse Abdominal radiographs show gas in the intestine wall (pneumatosis intestinalis) Necrotizing enterocolitis often involves the end of the ileum, cecum, and right colon, but any part of the intestines can be involved o The involved part is distended, friable, and congested, and can be gangrenous Microscopically, you’ll see coagulative necrosis, ulceration, bacteria, and gas bubbles Necrotizing enterocolitis has a high mortality, and those who survive often develop strictures from fibrosis from healing Infections of the fetus are acquired either transcervically (aka ascending) or transplacentally (hematologic) - - - Transcervical infections – most bacterial and a few viral infections of the fetus are gotten from spread from the cervicovaginal route o Can be gotten in utero or through labor o Fetus gets it by inhaling infected amniotic fluid into the lungs shortly before birth, or by passing through the infected birth canal o Preterm birth is often a consequence, and can be from damage of the amniotic sac by inflammation, or induction of labor by prostaglandins from infiltrating neutrophils o Inhalation of infected amniotic fluid usually leads to pneumonia, sepsis, & meningitis Transplacental infections – what most parasites and viral infections do o They get to fetal blood through the chorionic villi of the placenta o Can happen any time baby is in mom o Adverse effects of this are the minority, but include spontaneous abortion, stillbirth, hydrops fetalis, and congenital anemia o Parvovirus is common and likes erythroid progenitor cells in infected babies, causing erythema infectiosum aka “5th disease of childhood” o TORCH infections cause fever, encephalitis, chorioretinitis, hepatossplenomegaly, pneumonitis, myocarditis, hemolytic anemia, and vesicular or hemorrhagic skin lesions o Infections early in gestation can cause growth and mental retardation, cataracts, heart anomalies, and bone defects Sepsis is grouped as early onset (first 7 days of life) or late (7 days to 3 months) o Early sepsis is gotten at or shortly after birth, and causes pneumonia, sepsis, and meningitis within 4-5 days of life Group B strep is the most common organism for early onset-sepsis, and the most common cause of bacterial meningitis o Late-onset sepsis is usually listeria or candida Fetal hydrops – accumulation of edema fluid in the fetus - Before we started preventing it, the most common cause was hemolytic anemia from Rh blood group incompatibility between mom and baby, called immune hydrops o o o o o o o o o o Happens when the fetus inherits RBC antigens form dad that are foreign to mom, so mom immune system reacts to kill them, causing hemolysis Antibodies mom makes can freely pass through the placenta to the fetus Fetal RBCs can get to mom’s circulation in the last trimester, when the cytotrophoblast is no longer there to be a barrier, or during childbirth So mom sees the foreign antigen then and forms antibodies Only the Rh D antigen causes the incompatibility If there’s ABO incompatibility and these fetal RBCs enter mom circulation, mom coats them with anti-A or anti-B antibodies that remove them, and don’t cross the placenta Hemolytic disease for Rh incompatibility only happens when mom is exposed to a significant placental bleed Initial exposure of mom to the Rh forms IgM’s, so Rh disease is uncommon with the first pregnancy Exposure in future pregnancies leads to quick IgG responses, and risk for immune hydrops We’ve decreased the risk of this with Rhesus immune globulin (RhIg) with anti-D antibodies You give it to them at 28 weeks, and within 72 hours of delivery to Rh negative moms when they have Rh positive fetuses ABO incompatibility happens in about ¼ of pregnancies, but hemolysis only happens in 1/10 of those cases, and of those, way less actually are bad enough to need treatment Most IgM anti-A’s and anti-B’s don’t cross the placenta Neonates express RBC antigens A and B poorly Many cells other than RBCs express A and B antigens, so they absorb some of the immune attack if there is one ABO hemolytic disease happens pretty much only in babies with A or B antigens and an O mom Some O moms have IgG antibodies against A or B, even without ever seeing them before There’s no effective protection against ABO rxns, but usually disease is minmal 2 consequences of excessive destruction of RBCs in the neonate: Anemia – direct result of RBC loss If hemolysis is mild, the spleen and liver may be able to keep up and replace what you’re losing More severe hemolysis causes progressive anemia that can lead to hypoxic injury of the heart and liver Liver injury decreases plasma proteins Heart hypoxia can cause decompensated heart failure, leading to increased systemic pressure Low plasma proteins and high pressure cause generalized edema(anasarca), causing hydrops fetalis - - Jaundice – hemolysis produces unconjugated bilirubin The bilirubin can also get through the blood-brain barrier to cause CNS damage called kernicterus Since that’s treated well, nonimmune hydrops is the main cause of fetal hydrops o The 3 major causes of nonimmune hydrops are cardiovascular problems, chromosome problems, and fetal anemia o Cardiovascular problems lead to intrauterine heart failure and hydrops fetalis o Chromosome problems like turner syndrome (45, X), and trisomies 21 and 18 cause fetal hydrops In the Turner phenotype, problems with lymphatic drainage from the neck can cause postnuchal fluid accumulation, called cystic hygromas o Fetal anemia can happen, most often from homozygous α-thalassemia o Parvovirus B19 can cause hydrops fetalis It gets into erythroid precursors (normoblasts), replicates, causing apoptosis of the RBC progenitor, and isolated RBC aplasia o Twins can cause hydrops fetalis Hydrops fetalis is the most severe manifestation of intrauterine fluid accumulation If you see dysmorphic features, it suggests a chromosome problem In hydrops with fetal anemia, the fetus and placenta look pale, and often have enlarged liver and spleen from heart failure and congestion The bone marrow shows compensatory hyperplasia of the RBC precursors, except in parvovirus aplasia RBC making also happens int eh liver, spleen, and lymph nodes, and other places outside the bone marrow The increased hematopoietic activity causes lots of immature RBCs in circulation, including reticulocytes, normoblasts, and erythroblasts (in erythroblastosis fetalis) The most serious threat in fetal hydrops is CNS damage, called kernicterus o The brain is enlarged and edematous, and looks bright yellow from bilirubin Mild hydrops causes pallor with possible hepatosplenomegaly leading to jaundice More serious hydrops shows intense jaundice, generalized edema, and neuro problems