The Dynamic Nature of Infectious Disease
advertisement

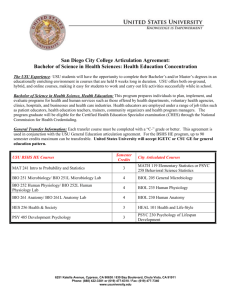
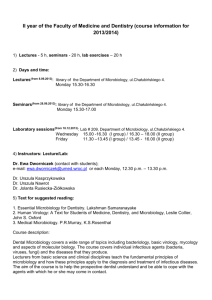
BIO 580 Medical Microbiology Unit 1 – The Adversaries 1 The Dynamic Nature of Infectious Disease Lecture 1 Objectives: Understand that infectious disease is dynamic; diseases emerge and disappear, and perhaps reemerge over time. The major diseases of our past may not be the major diseases of today. New diseases will continue to emerge in the future. Understand the major factors that influence why a new disease emerges, especially factors that can be influenced by human activity. Overview of human history with infectious disease: Year 1876 1885 191819 1928 1944 1952 1962 1967 1969 1975 1976 1977 June 1981 1983 1984 1990 1991 1993 1996 1997 1999 2002 2003 2009 Event Koch proves that a specific microbe (Bacillus anthracis) causes a specific disease (Anthrax) Pasteur treats a boy post-exposure, with attenuated rabies Pandemic of Influenza A H1N1 (Spanish Flu) kills 500,000 Americans, 50 million worldwide Penicillium discovered to kill Staphylococcus Penicillin introduced into general clinical practice Staphylococcal strains demonstrate resistance to penicillin Machupo emerges in Bolivia Marburg terrorizes Germany Emergence of Lassa in Nigeria Global vaccination campaign eradicates smallpox Emergence of Ebola in Zaire Emergence of Lyme disease (Borrelia bergdorferi) 182 American Legionnaires get sick in Philadelphia, 29 die (Legionella pneumophilia) Emergence of penicillin resistant Neisseria gonorrhoea Gonorrhea triple antibiotic resistant CDC’s Morbidity and Mortality Weekly Report describes a curious new health problem in American homosexuals 1,000th official AIDS case documented Causative agent of AIDS identified - HIV Jim Henson is killed by a new stain of Streptococcus Drug resistant tuberculosis surfaces in the US 4 children die of E. coli hemorrhagic syndrome Sin Nombre emerges in the Four Corners area Recognition of BSE and nvCJD Vancomycin-resistant S. aureus reported in Japan Vancomycin-resistant S. aureus reaches Michigan “Bird flu”(Influenza A H5N1) in Hong Kong West Nile seen in U.S. for first time West Nile reaches west coast SARS-CoV emerges Influenza A (H1N1) – first Influenza pandemic in 40 yrs Homework – ID microbial agent of disease as virus (V), bacterium (B), protozoa (P), Fungi (F) BIO 580 Medical Microbiology Unit 1 – The Adversaries 2 Preparation for next class meeting: Write the take home message from today in a single sentence in the space below: Read in the text – Introduction and Chapters 1, 2, and 3 (We will discuss the info in order Ch. 1, 3, 2). Terminology – Find definitions for these terms. You may use one of the on-line medical dictionaries on our course web site http://www.cst.cmich.edu/users/alm1ew/MM%20Index%20Page.html Used in Lecture 1 Infectious disease - any change from a state of health in which part or all of the host body is not capable of carrying on its normal functions due to the presence of a parasite or its products. Parasite Attenuated – Pandemic – Eradicate - BIO 580 Medical Microbiology Unit 1 – The Adversaries 3 UNIT ONE - THE ADVERSARIES Unit One - Outline of Topics I. Review of Microbes (viruses, bacteria, fungi, protozoa, helminths, arthropods, normal microbiota) II. Host Defenses A. Nonspecific Defenses 1. Defenses against entry a. Physical b. Chemical c. Biological 2. Defenses of the interior a. Complement cascade b. Acute phase proteins c. Interferons d. Phagocytic cells i. polymorphonuclear leukocytes ii. monomorphonuclear leukocytes e. Nonspecific cytolytic cells B. Specific Defenses 1. T lymphocytes a. Recognition of specific antigen (TCR and MHC) b. Activation against a specific antigen (role of APC and TH) c. Response to specific antigen i. T helpers ii. T cytotoxic iii. T regs 2. B lymphocytes a. Recognition of specific antigen (BCR) b. Activation against a specific antigen (role of APC and TH) c. Response to a specific antigen i. Plasma cells 3. Memory cells (primary vs secondary response) BIO 580 Medical Microbiology Unit 1 – The Adversaries 4 Unit One - Background Terminology/Concepts – will not be covered in lecture Obligatory Steps For Infectious Microbes: Phenomenon 1. Entry Step attach and enter into body 2. Spread local or general spread in body multiply 3. Multiplication 4. Evasion evade host defenses 5. Transmission exit from body 6. Pathology cause damage in host How evade host's natural protective and cleansing mechanisms evade natural barriers and immediate local defenses but many offspring will die in host evade phagocytic and immune defenses long enough for full cycle in host to be completed leave body at a site and on a scale that ensures spread to fresh host not strictly necessary but often occurs Pathogen - agent capable of causing disease Pathogenicity – ability to cause disease Frank pathogen= obligate pathogen– causes disease in a healthy host by direct interaction Opportunistic pathogen- may cause disease under the right conditions Virulence – degree or intensity of pathogenicity. Dependent on: 1. Invasiveness – ability of organism to spread 2. Infectivity – ability of organism to leave point of entry 3. Pathogenic potential – degree pathogen causes damage Virulence factors – individual characteristics of a specific strain of microbe that confer virulence Colonization (esp. by bacteria/yeast) – establishment of a site of replication – dependent on attachment BIO 580 Medical Microbiology Unit 1 – The Adversaries 5 Symbiosis - an association of two different species of organisms. Commensalism - one species uses the body of another species as a habitat and possibly as a source of nutrition. Mutualism - a reciprocal relationship between two species. Parasitism - one species in a relationship benefits and the other does not. ------ Respiration - use electron transport chain with an external e- acceptor (like O2 or NO3) as the terminal e- acceptor Fermentation - no external e- acceptor, one of the substrates involved accepts the eFacultative fermenter – will respire in the presence of external electron acceptors and ferment in their absence (Ex. Escherichia coli) Obligate aerobe - must have O2 because only O2 can serve as the terminal e- acceptor (Ex. Bacillus spp.) Facultative anaerobe - will use O2 for aerobic respiration if it’s present but will switch to fermentation or anaerobic respiration if no O2 (Ex. E. coli) Aerotolerant anaerobe - can't use O2 as an external e- acceptor, but not killed by it. Strict or obligate anaerobe - killed by exposure to O2 (Ex. Bacteroides fragilis) Microaerophilic - grows optimally in presence of oxygen concentrations that are below atmospheric concentrations (ex. the streptococci) BIO 580 Medical Microbiology Unit 1 – The Adversaries 6 UNIT ONE – THE ADVERSARIES I. THE MICROBES Objectives: To Review: 1. important structural features of viruses 2. sequence of steps during viral infection 3. consequences of viral infections at a cellular level 4. important structural features of bacteria 5. key differences between Gram positive and Gram negative cell walls 6. clinical significance of LPS, capsules, flagella, fimbriae, and pili 7. important features of eukaryotic pathogens: fungi, protozoa, helminths, arthropods 8. distribution and significance of normal microbiota by way of clinical cases A. VIRUSES - Obligate intracellular parasites Common structural features 1. Genetic material - DNA or RNA, ss or ds 2. Outer coat - capsid - composed of subunits called capsomers Nucleic acid + capsid = nucleocapsid Only nucleocapsid = naked Nucleocapsid surrounded by a lipid and protein envelope = enveloped *Outer surfaces (capsids or envelopes) impt cause they 1st make contact w/ host cells. BIO 580 Medical Microbiology Unit 1 – The Adversaries 7 Viral infection of host proceeds through several steps: 1. Entry into body of host - 4 routes 1) inhalation of droplets 2) ingestion 3) direct transfer 4) bites of arthropod vectors 2. Adsorption to target cell(s) in host – specific interaction between virus surface molecules and receptors on target cells *** 3. Entry into target cell - 3 mechanisms 1) Fusion (enveloped) 2) Receptor-mediated endocytosis (RME) (naked & enveloped) Entry step ends with release of viral nucleic acid inside host target cell. 4. Multiplication w/in the target cell (obligate intracellular) – complex process 1) synthesis of viral mRNA DNA viruses may use host RNA polymerase -- viral DNA viral mRNA RNA viruses have to use viral RNA polymerases 2) translation of viral proteins in host cytoplasm using host ribosomes – viral mRNA can displace host mRNA 3) replication of viral nucleic acid 4) assembly of nucleic acid & capsomers into new nucleocapsids (= viral progeny) 5. Release from host cell (immediate or delayed) – 2 mechanisms 1) lysis 2) budding (acquisition of envelope) – BIO 580 Medical Microbiology Unit 1 – The Adversaries 8 Pathology - effects of viral infection on the targeted cell 1) lysis – 2) persistence – 3) latency ( lytic) – 4) transformation – BIO 580 Medical Microbiology Unit 1 – The Adversaries 9 CONCEPT CHECK - Viruses In the space below, in your own words, describe in complete detail: 1) the significance of surface projection – target cell receptor interactions in viral infections 2) the two mechanisms by which an enveloped virus may enter into a target host cell BIO 580 Medical Microbiology Unit 1 – The Adversaries 10 B. BACTERIA - prokaryotes Common structural features 1. Genetic material – ds, circular DNA = “chromosome” 2. Ribosomes are only organelle – 70S (30S + 50S) 3. Cell membrane – site of many metabolic functions (e.g., respiration) 4. Cell wall – shape, rigidity, strength; impt in virulence and immunity Compound responsible for strength of cell wall is peptidoglycan (hexose sugars + amino acids) – unique to bacteria BIO 580 Medical Microbiology Unit 1 – The Adversaries 11 Differences in cell wall structure - Gram positive vs. Gram negative Gram positive peptidoglycan layer is thick highly polar hydrophilic surface Lipoteichoic acids = LTA resists activity of bile digested by lysozyme synthesis is disrupted by penicillin and cephalosporin antibiotics (more in Unit 4) Gram negative peptidoglycan layer is thin, overlaid by outer membrane that contains lipopolysaccharide and lipoprotein outer membrane is polar, but lipids are hydrophilic Lipopolysaccharide = LPS o carbohydrates antigenicity o lipid A is toxic = endotoxin induces fever, increases vascular permeability, may result in shock. etc. (more Units 2 & 3) BIO 580 Medical Microbiology Unit 1 – The Adversaries 12 5. Structures exterior to the cell wall in some bacteria (more common in pathogens) a. Capsule – high molecular weight polysaccharides slimy and sticky clinically relevant for 2 reasons 1) attach to a wide variety of surfaces * 2) more resistant to engulfment by host defense cells ** b. Flagella 1) allow bacteria to move 2) proteins are strongly antigenic/immune stimulating c. Fimbriae (aka “common pili”, esp. in the Neisseria) 1) attachment (fimbriae adhesins to target cell membranes) 2) evading engulfment d. Pili (aka “sex pili”) 1) exchange of genetic info, incl. antibiotic resistance (more in Unit 4) Bacterial infection of host proceeds through several steps: 1. Entry into body of host – 3 routes 1) direct contact 2) ingestion 3) fomites (inanimate objects) 2. Adhere to, colonize, (and possibly invade) host tissues or cells (infection may be extracellular or intracellular) 3. Evasion of host defenses (more in Unit 2) 4. Multiplication in the host (extracellular or intracellular) 5. Pathology (more in Units 2 and 3) 1) toxins 2) host immune response 6. Transmission to new hosts – usually passive in body fluids BIO 580 Medical Microbiology Unit 1 – The Adversaries 13 EUKARYOTIC PATHOGENS C. FUNGI 1. Morphology cell wall contains chitin; plasma membrane contains ergosterol yeast vs mold hyphae mycelium Dimorphic - 2 forms – yeast and mold 2. Reproduction mold vs yeast spores division budding 3 types of fungal infections = mycoses 1) superficial – 2) subcutaneous – 3) systemic or deep Infections are most serious in immunocompromised. D. PROTOZOA 1. Infection may be extracellular or intracellular 2. Evasion of host defenses 3. Reproduction asexual in humans, sexual absent or in insect vector. 4. Transmission bites of insects ingestion sexually transmitted BIO 580 Medical Microbiology Unit 1 – The Adversaries 14 E. HELMINTHS – multicellular worms 1. Exs. tapeworms, flukes, nematodes 2. Have complex life cycles 3. Transmission fecal-oral ingestion of larvae in tissues active penetration by larvae bites of insects F. ARTHROPODS 1. Exs. mosquitoes, biting flies, fleas, ticks, lice 2. increases potential for infection with viruses and protozoa NORMAL MICROBIOTA = Indigenous microbiota (= Normal flora) 1012 eukaryotic cells in adult human - 1013 prokaryotic Clinical significance 1. common contaminants of clinical specimens Fig 8.1 and Fig 8.2 2. opportunistic pathogens In class mini clinical cases BIO 580 Medical Microbiology Unit 1 – The Adversaries 15 Objectives: 1. understand the multiple lines of defenses against microbial infection 2. recognize the signs of acute inflammation when presented in a clinical context and describe how each sign of acute inflammation is generated at a cellular/tissue level 3. know why/how the alternate complement cascade is activated, what the important molecules formed are, what their function is, and what the consequences of complement activation are 4. understand how complement and phagocytosis are integrated processes 5. compare and contrast PMNs and macrophages 6. understand the importance of direct cell-cell contact in phagocytosis and the relationships between capsules, opsonins, and phagocytosis Terminology: Inflammation - the body’s response to injury or infection, which may be acute or chronic. Acute inflammation - the immediate defensive reactions to any injury. It involves swelling, redness, heat, and pain. Edema - excessive accumulation of fluid in the tissues. Erythema - abnormal flushing of the skin caused by dilation of the blood capillaries. Opsonin - a molecule that attaches to cells, provides a bridge to receptors on phagocytic cells, and enhances the rate of phagocytosi BIO 580 Medical Microbiology Unit 1 – The Adversaries 1 Cells of the Immune System (White Blood Cells = WBC = leukocytes) Monocytes Mononuclear Macrophages (differentiated monocytes, found in tissues) leukocytes (agranulocytes) Phagocytes Neutrophils Eosinophils Basophils Mast cells (differentiated basophils, found in tissues) Natural Killer (NK) cells Killer (K) cells Lymphocytes Polymorphonuclear leukocytes (granulocytes) Large Granular Lymphocytes (LGL) Cytotoxic T cell (TC) Helper T cell (TH) Regulatory T cell (Tregs) T lymphocytes (T cells) Effector B cells/ Plasma cells B lymphocytes (B cells) BIO 580 Medical Microbiology Unit 1 – The Adversaries 1 Origins of Cells of the Immune System BIO 580 Medical Microbiology Unit 1 – The Adversaries 18 II. HOST DEFENSES The immune system is composed of 2 arms innate = nonspecific – already in place, response is rapid, not as efficient adaptive = specific – must be induced, response is slower, highly efficient, enhances nonspecific. Has “memory” A. Nonspecific Defenses 1. Defenses against entry into the host (1st line defenses) a. Physical defenses (examples) 1. epithelial cells 2. turbulence 3. shedding, scraping, flushing (saliva, urine) 4. muco-ciliary clearance (1-3 cm/hr) b. Chemical defenses (exs) 1. acids (e.g. gastric, fatty acids) 2. enzymes (e.g. lysozyme in saliva, tears, perspiration, urine) 3. other microbicidal chemicals (e.g. zinc, dermicidin) c. Biological defenses (exs) 1. normal microbiota – physical, competition, inhibitory substances 2. immune defense cells and molecules 2. Defenses of the interior of the host (2nd line defenses) Inflammation a. phagocytic cells b. cytolytic cells c. acute phase proteins i. CRP ii. interferon iii.complement BIO 580 Medical Microbiology Unit 1 – The Adversaries 19 Inflammation - a process that coordinates and regulates all aspects of non-specific interior defense. Acute inflammation is characterized by: 1. increased blood supply to the area 2. increased capillary permeability 3. accumulation of neutrophils Signs of acute inflammation – 4 signs 1. 2. 3. 4. Triggers of acute inflammation – 2 triggers 1. cell/tissue damage/injury chemical “alarms” 2. cell wall components of bacteria (peptidoglycan, LTA, LPS) How Signs of Acute Inflammation are Produced 1. release of Inflammatory Mediators (=IM; see table 9.3) 2. vaso-dilation & blood flow 2. endothelial cells of vessels contract 3. plasma leaks out of vessels & into tissues = exudation 4. swelling pressure on nerve endings bradykinin ***Increased blood flow & capillary permeability - a mechanism for white blood cells and critical soluble factors to enter the tissues to combat microbial invaders. BIO 580 Medical Microbiology Unit 1 – The Adversaries 20 The Critical White Blood Cells (WBC = leukocytes) a. Phagocytes – professional engulfing cells 2 main roles for phagocytes 1. engulf and destroy foreign matter 2. secrete chemicals (esp. cytokines) Cytokines: (see table 11.2) small secreted proteins that mediate and regulate inflammation, immunity, and hematopoiesis act over short distances, short duration, and low conc. receptor binding induces signal transduction and transcription and translation 2 main kinds of professional phagocytic cells 1. polymorphonuclear leukocytes (= PMN = polymorph = neutrophils) – are granulocytes 2. mononuclear leukocytes - monocytes & macrophages – are agranulocytes 1. polymorphonuclear leukocyte dominant cell type in early stages acute inflammatory response made in the bone marrow - 80 mil/min dominant WBC, ~5,000/ul of blood - ↑15,000-20,000/ul live for 2-3 days - function in anaerobic environments abundant cytoplasmic granules contain loads of antimicrobial enzymes and chemicals, esp. lysozyme best with extracellular pathogens, esp. bacteria 2. mononuclear leukocyte majors players later in inflammatory process made in bone marrow in the blood - monocytes (~600/ul); in tissues - macrophages (~60,000) conc. in lung, liver, lymph nodes, spleen live for months-years fewer granules (acid hydrolases, peroxidase) one of the antigen presenting cells secrete lots of different proteins (incl. lysozyme, nitric oxide, cytokines, complement factors) best with intracellular pathogens BIO 580 Medical Microbiology Unit 1 – The Adversaries 21 BIO 580 Medical Microbiology Unit 1 – The Adversaries 22 Process of Phagocytosis – 6 steps 1. Activation – phagocytes are circulating with the bloodstream, need to move to the site of inflammation. a. margination b. pavementing c. diapedesis 2. Migration via chemotaxis – phagocytes have receptors for chemoattractant molecules, will track a concentration gradient of these molecules to the site where they are being produced. 3-6. – illustrated in diagram 3. Attachment – phagocytosis cannot happen until the phagocyte makes direct contact with the surface of the microbe. That direct contact is mediated by receptors on the surface of the phagocyte. Pathogen-Associated Molecular Patterns Microbe - PAMP – PRR – phagocyte Pattern Recognition Receptors PAMP incl. LTA & LPS (table 9.2) After PAMP-PRR interaction, macrophages secrete pro-inflammatory cytokines (TNF, IL-1) enhance antigen-presentation leads to activation of Th1. We’ll talk about this later. 4. Engulfment 5. Phagosome-lysosome fusion and intracellular killing 6. Expulsion of debris Phagocytosis - Diagram BIO 580 Medical Microbiology Unit 1 – The Adversaries 23 Role of Opsonins in Process of Phagocytosis - Diagram (review definition of opsonin) Microbe +phagocyte Opsonin none present Interaction Rate of Phagocytosis BIO 580 Medical Microbiology Unit 1 – The Adversaries 24 Phagocyte Intracellular Killing Mechanisms 1. Oxygen-dependent killing (see box 9.2, p. 83) – PMN and macrophages “oxidative burst” Reduction O2 NADPH NADP superoxide anion hydrogen peroxide singlet oxygen hydroxyl radicals O2H2O2 1 O2 OH Reactive Oxygen Intermediates (ROI) Other reactive intermediates reactive nitrogen (nitric oxide = NO) (macrophages) reactive chlorine (OCl) + myeloperoxidase (PMN) phagosome membrane 2. Oxygen-independent killing compounds contained in cytoplasmic granules (see Table 14.2, p. 153) acid hydrolases (PMN) cathepsin G (PMN) cationic proteins (PMN, eosinophils) defensins (PMN) lactoferrin (PMN) lysozyme (PMN, macrophage) – peroxidase (eosinophils) BIO 580 Medical Microbiology Unit 1 – The Adversaries 25 b. Cytolytic Cells 1. natural killer cells (NK) (LGL) target - intracellular pathogens, primarily viruses attach – by way of receptors to glycoproteins on infected cells release - perforins (membrane channels) granzyme (apoptosis) also secrete TNF also – secrete -IFN, impt early source, can activate macrophages 2. basophils and mast cells target – parasites can be triggered to discharge cytoplasmic granules release histamine, heparin, anaphylactic factors 3. eosinophils target - large parasites (e.g. helminthes) can be triggered to discharge cytoplasmic granules release basic proteins, perforins, ROI chemical burns BIO 580 Medical Microbiology Unit 1 – The Adversaries 26 c. The Critical Soluble Factors Acute Phase Proteins Plasma proteins – proteins that increase in concentration 2-100X during the acute phase of an infection, in response to cytokines (IL-1, TNF). i.. C-reactive protein (CRP) – produced by liver - uses pattern recognition to bind to bacteria acts as an opsonin activates complement cascade often used to monitor inflammation ii. Interferons Interferons – first recognized because they interfere w/ viral replication 3 classes of Interferons: 1. - produced by leukocytes (WBC) – anti-viral - prod w/in 24h 2. - produced by fibroblasts and other cells – anti-viral - prod w/in 24 h 3. - produced by NK and esp. T lymphocytes – anti-viral and involved in cell-cell communication. BIO 580 Medical Microbiology Unit 1 – The Adversaries 27 iii. Complement - activation of the alternate cascade (= properdin pathway) - A group of 20 serum proteins – form an enzymatic cascade C3 (most abundant, prod. by liver cells) C3a C3b Factor B C3bB Factor D C3bBb = C3 convertase --------------------------------------------------------------------------------------------------------------------C3 C3a C3 C3b C3a C3b C5 (prod by macrophages) C5a C5b C5b678 multiple C9 cell lysis Microbe +phagocyte Opsonin none C3b CRP Interaction Rate of Phagocytosis BIO 580 Medical Microbiology Unit 1 – The Adversaries 28 Integration of Nonspecific Defenses 1. Stimulus a. cell/tissue injury inflammatory mediators released b. microbial surface polysaccharides 2. Within seconds to minutes a. acute inflammation begins vaso-dilation of capillaries increases blood flow to/volume at the site increased vascular permeability exudation of plasma, cells, and proteins b. acute phase proteins increase in concentration c. alternate complement cascade is activated C3a and C5a mast cell degranulation maintains vaso-dilation/vascular permeability C5a attracts phagocytes from vasculature C3b and C5b bind to cell surfaces C3b opsonin 3. Minutes to hours a. PMNs arrive in huge number and encounter cells opsonized by C3b and CRP phagocytosis is enhanced. 4. Hours to days a. Interferons are produced b. NK arrive c. Macrophages arrive BIO 580 Medical Microbiology Unit 1 – The Adversaries 29 SUMMARIZE – Nonspecific Defenses List the Nonspecific Interior Defenses important against Bacteria List the Nonspecific Interior Defenses important against Viruses BIO 580 Medical Microbiology Unit 1 – The Adversaries 30 CONCEPT CHECK – Nonspecific defenses Bubble Map Characteristics unique to PMN PMN Shared characteristics Characteristics unique to macrophages Macrophage BIO 580 Medical Microbiology Unit 1 – The Adversaries 31 CONCEPT CHECK – Nonspecific defenses Draw a concept map that illustrates the integration of complement and phagocytosis BIO 580 Medical Microbiology Unit 1 – The Adversaries 32 CONCEPT CHECK - Nonspecific Host Defenses Steve, a college student, was backpacking in a remote wilderness region with some friends. While pitching a tent, he tripped and fell. In an attempt to break his fall, he extended his arms and sustained a puncture wound to his right palm. Although the wound was painful and bled for a short time, it didn’t appear to be serious, and Steve fell asleep that night unconcerned. By the next morning, however, Steve noticed that the tissues immediately surrounding his wound were red, swollen, and warm. A round area about 1 inch in diameter really looked abnormal compared to the rest of his hand. The affected area was also painful, especially when he touched it or bumped it. After hiking all day, the sore hand was even more painful, and a thick yellow discharge oozed from the open wound. Steve felt unusually tired, his body ached, and a brief chill made him aware that he was getting a fever. His friends helped him elevate his arm and applied warm compresses to his palm, hoping that he would feel better in the morning. 1. List the nonspecific defenses against entry that are relevant to skin. 2. How were Steve’s skins defenses against entry overcome? 3. List the nonspecific interior defenses that would become activated in this case of bacterial invasion. 4. What are the signs in the case history that Steve is experiencing an inflammatory process? List them. 5. Describe the mechanisms at the cellular/tissue level that cause each of the signs of inflammation listed in 4 above? BIO 580 Medical Microbiology Unit 1 – The Adversaries 33 Supplemental information FYI Blood (modified from Wikipedia) Blood accounts for 8% of the human body weight. The average adult has a blood volume of roughly 5 liters (1.3 gal), composed of plasma and several kinds of cells; these formed elements of the blood are erythrocytes (red blood cells; RBC), leukoytes (white blood cells; WBC), and thrombocytes (platelets). By volume, the red blood cells constitute about 45% of whole blood, the plasma about 54.3%, and white cells about 0.7%. Cells: One microliter of blood contains: 4.7 to 6.1 million (male), 4.2 to 5.4 million (female) erythrocytes. The proportion of blood occupied by red blood cells is referred to as the hematocrit, and is normally about 45%. 4,000–11,000 leukocytes. White blood cells are part of the immune system; they destroy and remove old or aberrant cells and cellular debris, as well as attack infectious agents and foreign substances. 200,000–500,000 thrombocytes: Platelets are responsible for blood clotting (coagulation). They change fibrinogen into fibrin. This fibrin creates a mesh onto which red blood cells collect and clot, which then stops more blood from leaving the body and also helps to prevent bacteria from entering the body. Plasma: About 55% of whole blood is blood plasma, a fluid that is the blood's liquid medium, which by itself is straw-yellow in color. The blood plasma volume totals of 2.7–3.0 liters (2.8–3.2 quarts) in an average human. It is an aqueous solution containing 92% water, 8% blood plasma proteins, and trace amounts of other materials. Plasma circulates dissolved nutrients, such as glucose, amino acids, and fatty acids (dissolved in the blood or bound to plasma proteins), and removes waste products, such as carbon dioxide, urea, and lactic acid. Other important components include: Serum albumin Blood-clotting factors (to facilitate coagulation) Immunoglobulins (antibodies) lipoprotein particles Various other proteins Various electrolytes (mainly sodium and chloride) The term serum refers to plasma from which the clotting proteins have been removed. Most of the proteins remaining are albumin and immunoglobulins. BIO 580 Medical Microbiology Unit 1 – The Adversaries 34 Constitution of normal blood Parameter Value hematocrit 45 ± 7 (38–52%) for males 42 ± 5 (37–47%) for females pH 7.35–7.45 base excess −3 to +3 PO2 10–13 kPa (80–100 mm Hg) PCO2 4.8–5.8 kPa (35–45 mm Hg) HCO3 21–27 mM oxygen saturation Oxygenated: 98–99% Deoxygenated: 75% Saliva (modified from Wikipedia) - Produced in salivary glands, human saliva is 98% water, but it contains many important substances, including electrolytes, mucus, antibacterial compounds and various enzymes It is a fluid containing: Water Electrolytes: (sodium, potassium, calcium, magnesium, chloride, bicarbonate, phosphate, iodine) Mucus. Mucus in saliva mainly consists of mucopolysaccharides and glycoproteins; Antibacterial compounds (thiocyanate, hydrogen peroxide, and secretory IgA) Epidermal growth factor or EGF Various enzymes. There are three major enzymes found in saliva. o α-amylase - starts the digestion of starch and lipase fat. o lingual lipase o Antimicrobials that kill bacteria: ** Lysozyme Salivary lactoperoxidase Lactoferrin o Proline-rich proteins (function in enamel formation, Ca2+-binding, microbe killing and lubrication) o Minor enzymes Cells: Possibly as much as 8 million human and 500 million bacterial cells per mL. The presence of bacterial products (small organic acids, amines, and thiols) causes saliva to sometimes exhibit foul odor. Opiorphin, a newly researched pain-killing substance found in human saliva. BIO 580 Medical Microbiology Unit 1 – The Adversaries 35 Lysozyme, also known as muramidase or N-acetylmuramide glycanhydrolase, are a family of enzymes that damage bacterial cell walls by catalyzing hydrolysis of 1,4-beta-linkages between N-acetylmuramic acid and N-acetyl-D-glucosamine residues in a peptidoglycan and between Nacetyl-D-glucosamine residues in chitodextrins. Lysozyme is abundant in a number of secretions, such as tears, saliva, human milk, and mucus. It is also present in cytoplasmic granules of the polymorphonuclear neutrophils (PMN). Urine is approximately 95% water. The other components of normal urine are the solutes that are dissolved in the water component of the urine. These solutes can be divided into two categories according to their chemical structure (e.g. size and electrical charge). Organic molecules These include: Urea – Makes up 2% of urine. Urea is an organic compound derived from ammonia and produced by the deamination of amino acids. The amount of urea in urine is related to quantity of dietary protein. Creatinine - Creatinine is a normal constituent of blood. It is produced mainly as a result of the breakdown of creatine phosphate in muscle tissue. It is usually produced by the body at a fairly constant rate (which depends on the muscle mass of the body). Uric acid - Due to its insolubility, uric acid has a tendency to crystallize, and is a common part of kidney stones. Other substances/molecules - Example of other substances that may be found in small amounts in normal urine include carbohydrates, enzymes, fatty acids, hormones, pigments, and mucins (a group of large, heavily glycosylated proteins found in the body). Ions These include: Sodium Magnesium Sulfates Potassium Calcium Phosphates Chloride Ammonium BIO 580 Medical Microbiology Unit 1 – The Adversaries 36 Objectives: 1. understand how the appropriate lymphocytes are selected and activated and amplified 2. understand how immune cells “talk” with each other via cytokines 3. compare and contrast activation and response of T and B lymphocytes 4. compare and contrast the activation and response of Th1, Th2, and TC 5. understand the interactions between nonspecific and specific host defenses 6. understand how the specific immune response focuses the nonspecific response 7. understand the power of the secondary (anamnestic) immune response B. Specific Defenses = adaptive = acquired 3rd line of defense – only one with antigenic memory based on lymphocytes feedback into the nonspecific defenses – enhance the effectiveness of the non-specific defenses Specific immune system has to: 1. recognize 2. activate 3. respond 1. Overview a. Recognition of antigen A specific interaction between an antigen and a receptor Anti gen Antigens incl: ***proteins (incl. proteins + carbos or lipids) (T and B) ***complex polysaccharides (B only) ***nucleic acids (B only) BIO 580 Medical Microbiology Unit 1 – The Adversaries 37 Full activation of the specific defenses involves several different types of immune cells working in concert: non-specific cells (antigen-presenting cells) specific cells (lymphocytes) Antigen-Presenting Cell (APC) Specialized cells that present microbial peptides (antigenic determinants) in a way that can be recognized by lymphocyte receptors. Most significant: dendritic cells (tissues) > macrophages > B cells Antigenic determinant (= epitope) – a certain stretch of peptides from a larger microbial antigen linear or conformational small in size 2 main types of Lymphocytes T lymphocytes (T cells) B lymphocytes (B cells Lymphocyte receptors (R) constant region – transmembrane variable region – interacts with microbial peptide General Overview of Antigen Presentation - Diagram Presentation of antigenic determinant by an APC to a lymphocyte occurs in draining lymph nodes (surfaces, tissues) or spleen (blood) Initiates a chain of events that transforms a small, resting, naïve lymphocyte into a highly active, functional lymphocyte (more later) BIO 580 Medical Microbiology Unit 1 – The Adversaries 38 b. Activation – from all the antigen naïve lymphocytes, selection of lymphocytes with complementary receptor that matches specific microbial antigenic determinant 1. receive and secrete cytokines 2. undergo proliferation = clonal expansion 1104 – 105 - occurs in lymphoid organs Results in an expanded population of immature effector lymphocytes 3. differentiate into functional sub-types effectors – fight this time memory – reserves, to be deployed in the future c. Response – of activated effector sub-types activated (= primed) effector T lymphocytes either: 1. kill infected cells 2. coordinate and regulate immune response activated effector B lymphocytes (called plasma cells) secrete antibodies BIO 580 Medical Microbiology Unit 1 – The Adversaries 39 2. Add in specifics T Lymphocytes 2 categories of T cells by surface marker called Cluster Determinant 1. CD4 - 2 functional types 1) T helper cells = TH - regulate the immune system by increasing the response ( by activating other immune cells). a) Subset Th1 b) Subset Th2 2) T regulatory cells (=Tregs) - regulate the immune system by the response 2. CD8 =T cytotoxic cells =TC = CTL- kill cells infected w/ intracellular pathogens a. Antigen Recognition by Antigen-Naïve, Resting T lymphocytes *T cell receptor interacts with microbial (foreign) antigenic determinant complexed with a self antigen Self antigens – Major Histocompatibility Complex (MHC) proteins – protein molecules on the surface of cells that mark them as “cells”. 2 classes of MHC Class I - on the surface of all nucleated host cells Class II – on the surface of APC THR - recog. antigenic determinant complexed w/ Class II MHC + co-stimulatory interactions (depend on who the APC is) TCR - recog. antigenic determinant complexed w/ Class I MHC + co-stimulatory interactions b. Activation of T lymphocytes – 3 steps 1. Receive cytokines from APC ex. IL-1 from macrophage 2. ↑ # of IL-2R and secrete/receive IL-2 proliferation Results in an expanded set of immature effector lymphocytes, all with same receptor for antigenic determinant complexed to MHC II (will all recognize the same microbial threat) 3. Differentiation into effector and memory T cells Tc, and NK BIO 580 Medical Microbiology Unit 1 – The Adversaries 40 c. Response of Effector T Lymphocytes Each category of effector T cell has a unique response: regulating the immune response = immunoregulation enhance response - TH subset Th1 – secretes IL-2 – stimulates Tc proliferation & maturation. Secretes -IFN – activates effector TC , activates macrophages and NK to kill their intracellular pathogens; (down regulates Th2) subset Th2 – secretes IL-4 – stimulates B cell proliferation & differentiation into plasma cells; (down regulates Th1) suppress response - Tregs OR direct cell killing = cytotoxicity – TC secrete perforin transmembrane channels secrete granzyme apoptosis also secrete TNF also secrete -IFN (activates NK and macrophages) BIO 580 Medical Microbiology Unit 1 – The Adversaries 41 Integration via Lymphocyte Recognition, Activation, and Response - Diagram BIO 580 Medical Microbiology Unit 1 – The Adversaries 42 B Lymphocytes a. Antigen Recognition by B Lymphocytes Receptor interacts with microbial (foreign) antigen alone – receptor does not interact with MHC. Can present antigen to Th2 b. Activation of B Lymphocytes 1.IL-2 from subset Th2 clonal expansion (= proliferation) 2.IL-4 from subset Th2 differentiation into effector (= plasma) and memory B cells c. Response of Effector B lymphocytes (=Plasma Cells) Secrete Antibody (Ab) at the rate of 1,000 molecules/min. BIO 580 Medical Microbiology Unit 1 – The Adversaries 43 Antibody Structure - Diagram BIO 580 Medical Microbiology Unit 1 – The Adversaries 44 Actions of Antibody Molecules – focus the non-specific 1. bind to microbial antigen – interfere with receptor interaction for any microbe that uses specific attachment sites = neutralizing ***2linking a bacterium to a phagocyte = opsonization (followed by phagocytosis) Microbe +phagocyte Opsonin none C3b CRP Ab C3b + Ab Rate of Phagocytosis -/+ + + 3. linking many small antigens together = agglutination (followed by phagocytosis) 4. complement activation - classical pathway (followed by either opsonization and phagocytosis or lysis) (notes p.45) 5. ADCC - antibody dependent cellular cytotoxicity (notes p. 47) BIO 580 Medical Microbiology Unit 1 – The Adversaries 45 Activation of Classical Complement Cascade - Diagram C1 C2 C2b C4 C2a C4b C4a C2a4b C3 C3a C3 C3b C3a C3b C5 C5a C5b C5b678 multiple C9 (MAC) Fill in: Triggers – Important molecules – Consequences Timing – Complement activation enhances phagocytosis and inflammation and leads to cell lysis. BIO 580 Medical Microbiology Unit 1 – The Adversaries 46 Classes of Antibody Molecules Antibody = Immunoglobulin (Ig) – proteins found in fluids in the body 5 Classes: Class Structure % IgG monomer 75-80 IgA 15-21 IgM monomer dimer pentamer IgD monomer <1 IgE monomer 0.01 6-7 Location serum, extra vascular spaces, crosses placenta serum, tears, saliva, mucus, colostrum serum, 1st made by virgin B cells, 1st made by fetus low levels in serum B cell surface skin RT fluid Roles fix complement opsonin neutralizing fix complement agglutinating ? regulate clonal expansion? bind to mast cells & basophils Feedback into the non-specific defenses; esp. complement, phagocytosis Function of Memory Lymphocytes – the reserves - stronger response on secondary exposure to antigen 1. are more memory cells then there were naive cells at the beginning of the primary response 2. were primed to antigen during primary response so are able to bind more strongly to APC 3. antigen-primed memory B cells differentiate into plasma cells more quickly 4. memory is usually long-lasting, years Primary versus Secondary (= anamnestic) Response BIO 580 Medical Microbiology Unit 1 – The Adversaries 47 Misc. Killer (K) cells Rely on antigen specific antibodies BUT interact with antibody in a nonspecific way, by way of the Fc. Participate in the non-specific interior defenses: K cells include: NK macrophage eosinophil All K cells have receptors for Fc of antibody molecules K cells bring about lysis of the antibody-coated cell in a process called antibody-dependent cellular cytotoxicity (ADCC); for pathogens that are too big to phagocytize. BIO 580 Medical Microbiology Unit 1 – The Adversaries 48 SUMMARIZE – Specific Defenses Fill in table Cytokine or proinflammatory mediator IL-1 IL-2 IL-4 IFN IFN IFN TNF Complete: TH function – recognition – activation – response – Th1 -- Th2 – TC function – recognition activation – response – Treg function – recognition activation – response – B Lymphocyte recognition – activation – response – Secreted by: Acts on: Functions to: BIO 580 Medical Microbiology Unit 1 – The Adversaries 49 SUMMARIZE – Specific Defenses List the Specific Interior Defenses important against Bacteria List the Specific Interior Defenses important against Viruses CONCEPT CHECK – Specific defenses Concept Map Draw a concept map that illustrates the connections between the specific and nonspecific immune responses BIO 580 Medical Microbiology Unit 1 – The Adversaries 50 CONCEPT CHECK – Specific Defenses Continuation of the Case of Steve When Steve. awoke on the second morning, his condition was clearly deteriorating. The first thing he noticed was that the small area of redness and swelling had extended to include his entire hand, with the margin of redness now visible just above his wrist. Faint red streaks had appeared along the inner part of his arm and tender lumps were noticeable below his elbow and under his arm. His fever seemed higher than the night before, and he felt too weak to walk. Steve was too sick to travel, and his friends figured that it would take several days to return with medical help. They decided to stay in camp and let Steve rest. Over the next couple of days Steve and his friends were relieved to find him gradually improving. The red area did not advance past his forearm. Although the hand remained painful and swollen, he felt less tired and the fever was gone. Four days after the first presentation of inflammation, when he was a little better, they headed back and took Steve to the nearest emergency room. The doctor diagnosed a presumed bacterial infection and prescribed a broad-spectrum antibiotic that was likely to be effective against the unknown infecting bacterium. The medication was taken orally, and Steve was sent home. The redness and swelling of the hand subsided gradually over the next two weeks. 1. What were the tender swellings that Steve noticed behind his elbow and under his arm and why were they swollen? 2. Steve began to improve within 4-5 days of initial infection. How could antibody have played a role in resolving Steve’s symptoms within this time frame? 3. What functions did these antibodies play in the immune response to Steve’s bacterial infection?