Clinical review of ambulance response time targets
advertisement

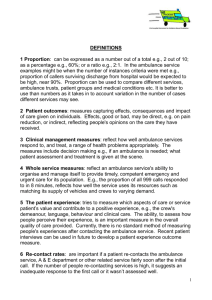
WRITTEN STATEMENT BY THE WELSH GOVERNMENT TITLE DATE BY Clinical review of ambulance response time targets 29 July 2015 Vaughan Gething AM, Deputy Minister for Health In a written statement in February about progress made in transforming the Welsh Ambulance Service since the publication of the McClelland review, I committed to update Assembly Members about a clinical review of the way we measure the timeliness and quality of delivery of emergency ambulance services. The clinical review was led by Dr Brendan Lloyd, medical director of the Welsh Ambulance Services NHS Trust working with the trust’s clinical services team and Dr Grant Robinson, Wales’ national clinical lead for unscheduled care. The review was set up to respond to the McClelland review recommendation that the Welsh Government should consider moving from a primary focus on the eight-minute response time target to a more intelligent suite of targets and measures, across the whole unscheduled care system. Professor Siobhan McClelland advised this should include a greater emphasis on patient outcomes and experience. Following the review, Dr Lloyd has written to me, on behalf of NHS Wales medical directors, outlining proposals to move from the time-based performance measures to an evidence-based approach, which focuses on quality of clinical care and patient experience. The eight-minute response time target was introduced 41 years ago and is based on evidence, which suggests it only improves outcomes for people who have suffered an out-of-hospital cardiac arrest. The clinical review has shown there is no evidence an eight-minute response will make a difference to the vast majority of people’s outcomes following treatment – about 95% of people who access the Welsh Ambulance Service. The rising and more complex demands placed on the ambulance service are well known – if we are to meet these demands and ensure the best outcomes for patients, we need to transform the way we deliver and measure emergency ambulance services. Dr Lloyd has therefore advised that a new clinical response model should be implemented in Wales. This will be similar to the approach piloted in two areas of England earlier this year, which has recently been expanded following encouraging results. Under the new model, which will be tested for 12 months from October 1, everyone who is in imminent danger of death and needs an immediate, lifesaving response will receive one in the fastest time possible. All other patients will receive a bespoke clinical response based on their health needs, rather than a generic response based solely on the 41-year-old eight-minute response model. The new model will give clinical contact centre call handlers extra time to triage those calls, which are not instantly identified as being an immediate threat to life, before dispatching an ambulance resource – this is similar to the English “dispatch on disposition” pilot. Call handlers will have up to 120 seconds extra to ask important questions about a patient’s symptoms; to accurately identify the nature of their condition and dispatch the correct type of response needed – this may be an advanced paramedic who can provide treatment at the scene or an emergency ambulance manned by a paramedic crew to assess and treat at scene and transport the patient to the most appropriate treatment centre as quickly as possible This new system will help to remove what clinicians describe as the “unnecessarily high and unevenly-distributed clinical risk”, which leads to the way the service currently dispatches ambulances to chase the response time target. The Welsh Ambulance Service regularly dispatches multiple vehicles to try and achieve the eight-minute target – in the Cardiff and Vale of Glamorgan area, for example, an average of two vehicles are dispatched to every call. Sending a faster rapid response car to the majority of 999 calls means the ambulance service can stop the clock and achieve the target but if a patient needs to go to hospital they must then wait for a larger emergency ambulance vehicle capable of transporting them. The new model will introduce three new categories of calls – red, amber and green: Red calls are immediately life-threatening calls –someone is in imminent danger of death, such as a cardiac arrest. There is compelling clinical evidence to show that an immediate emergency response will make a difference to a person’s outcome. The eight-minute target will be retained for this group of calls with an initial target of 65% receiving an eight-minute response. Amber calls are from patients who will often need treatment to be delivered on the scene and may then need to be taken to hospital. Evidence suggests that for this type of patient timely transport to the most appropriate care facility and clinicians has far more impact on their quality of life once they are discharged from hospital than a response within a defined time-frame. Patients in this category will continue to receive a fast blue light and sirens response from the Welsh Ambulance Service but there will be no time-based target for this group. Instead a range of clinical outcome indicators will be introduced to measure the quality and timeliness of care being delivered by ambulance clinicians alongside patient experience information, which will be published every quarter. These new indicators will build on measures, which have been tested over the last year and are already published by the Welsh Government, including how ambulance clinicians care for patients with stroke; fractured hips and a type of heart attack, known as STEMI. Green calls are non-serious incidents, which could often be managed by other health services, including healthcare advice or through self-care. This category also includes calls from healthcare professionals, which will be handled in a different, planned way in the future – this approach has been successfully tested in the Cwm Taf University Health Board area. The McClelland review also recommended the development of a wider suite of targets and standards, which incentivise change and provide a greater focus on patient experience and outcomes. To support this, the Emergency Ambulance Services Committee has developed a quality and delivery framework and an innovative five-step ambulance patient care pathway. This describes the Welsh Ambulance Service as a clinical service and a key part of the wider integrated healthcare system. It includes indicators, targets and measures for each of the five steps – how it helps people to choose the right service for their needs; how their call is dealt with; how a response is provided; treatment is delivered; and – if appropriate – how people are taken to hospital. These quality indicators will form part of a new suite of information, to be published quarterly, making the Welsh Ambulance Service among the most transparent in the world. We know from the latest National Survey for Wales that 97% of people who used the ambulance service had trust and confidence in the skills of ambulance clinicians. This striking result shows we must focus more on the care, compassion and continuity provided by our highly-skilled ambulance clinicians than simply measuring the worth of the service by the time it took an ambulance to respond to a 999 call. This pilot leads the way for the ambulance service to be at the forefront of future developments for patients and frontline clinicians and will put the Welsh Ambulance Service at the heart of the unscheduled care system. I will make an oral statement to the Assembly at the first opportunity in the autumn to update Assembly Members further. This statement is being issued during recess in order to keep members informed. Should members wish me to make a further statement or to answer questions on this when the Assembly returns I would be happy to do so.