I`m a new patient and need to fill out my initial paperwork
advertisement

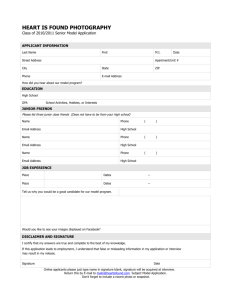
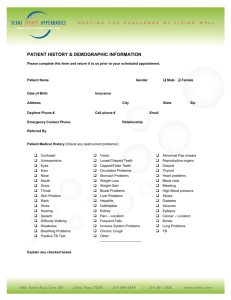
New Patient Information Packet Please: 1) Review “Payment Terms and Agreements”, “Notices of Privacy Practices for Protected Health Information” and “Online Communications Policy” located on this website 2) Print the 2nd and 3rd pages of this packet to fill out 3) Sign the following Consent/Signature sheet and the New Patient History form 4) Arrive 10 minutes prior to your scheduled appointment 5) Call at least 24 hours in advance if you need to cancel or reschedule 6) Be sure to bring both the Consent/Signature sheet and New Patient History form with you to your appointment. 7) You will also need to bring your insurance card, any applicable co-pay and a photo ID. Summit Gastroenterology Barcode Patient Consent, Contact and Signature sheet PLEASE PRINT: Patient Name: ___________________________________________ Date of Birth: _____________________ Social Security #: _________________________________ Present Address: _________________________________________________ Apartment #: _________ City ______________________ State ____________ Zip ___________________ Telephone (#1) ________________________ This is how we will contact you to provide results and appointment reminders (#2) ________________________ This is our backup number to reach you Primary Language______________________ Race ______________________ Ethnicity ____________________ ……………………………………………………………………………………………………………………… In case of emergency please notify: Emergency contact name ____________________________________ Relation _______________________ Telephone _____________________________ ……………………………………………………………………………………………………………………… *PLEASE PROVIDE YOUR INSURANCE CARD AND PHOTO ID TO THE RECEPTIONIST NAME OF PRIMARY INSURED (if different from above) _______________________________________________ SS# OF PRIMARY HOLDER (if different) ___________________DOB OF PRIMARY HOLDER ______________ RELATIONSHIP TO PATIENT ____________________________ ……………………………………………………………………………………………………………………… (Please review the Patient Information Packet before signing below. Please note that we will leave normal lab or test results on your answering machine unless you specifically ask us not to) 1) I have reviewed the document, “PAYMENT TERMS AND AGREEMENTS, V 2/11/2011” and my signature here indicates that I agree to the terms set forth: X__________________________________ Signature of patient or patient representative 2) I have reviewed the document, “Notice of Privacy Practices for Protected Health Information”: X__________________________________ Signature of patient or patient representative 3) I authorize the exchange of pharmacy information between my pharmacy and Dr. Aaron Burrows, MD P.C.: X__________________________________ Signature of patient or patient representative 4) I have reviewed the “Online Communications Informed Consent” and “Patient Portal Info”: X__________________________________ Signature of patient or patient representative My email address is: __________________________________ (This allows us to notify you of test results and allows you access to the patient portal.) CONFIDENTIAL PATIENT INFORMATION Your Name: Your Age: Your Referring Doctor: Patient barcode goes here (do not write in this section) What is your Chief Complaint? Regarding this illness, do you have or have you had: Abdominal pain Heartburn/reflux Nausea Vomiting Blood in vomit Difficulty swallowing Loss of Appetite Constipation Diarrhea Fever Red Blood in stool Black/tarry stools Unintended weight loss Regurgitation of food Yellow skin/eyes Have you ever had a COLONOSCOPY: Yes -when?____________ No Have you ever had an Upper Endoscopy (EGD) : Yes- when?___________ No Please list your past medical history: Please list all your previous surgeries (and approximate dates): Please list all your current medications. Include birth control, aspirin, over-the-counter, or homeopathic medicines: Drug allergies and type of reaction: Which Vaccinations have you had?: □Hepatitis A-Year completed: □Hepatitis B-Year completed: Family Health (please list any health problems or cancers for your immediate family): Mother: Father: Siblings: Grandparents: Is there a history of colon polyps in your family? Yes No I don’t know Smoking? Yes No Former Recreational Drugs? Yes No Type:_________ How many years did you smoke? :______ How Much?: ______ Alcohol? None Occasional Moderate Heavy Caffeine use: None Moderate Heavy Occupation: Diet: Regular Vegetarian Sexual History: Sexually active? Yes No Heterosexual Homosexual Bisexual Your Height: ___________ Weight: _______________ Review of Systems (Please circle only those conditions below that you have or have had in the past) Constitutional: Fatigue Fever Night sweats Weight gain (________lbs) Weight loss (________ lbs) Hearing loss Nose bleeds Sinus Problems Sore throat Bleeding gums Snoring Mouth ulcers Cardiac: Chest Pain/Pressure Arm pain on exertion Shortness of breath Palpitations Heart Murmur Angina /Heart Attack Heart valve infection CHF Leg Edema Abnormal EKG Respiratory: Cough COPD/Emphysema Wheezing Shortness of breath Asthma ABNORMAL Digestive: Abdominal pain Vomiting ABNORMAL Change of Appetite Black or tarry stools Celiac Sprue/Gluten sens Lactose Intolerance Hepatitis C Hemorrhoids Diverticulosis Hiatal Hernia Ulcers Pancreas problems Liver disease Gallbladder problems Inflammatory Bowel Disease Irritable Bowel Syndrome GI Cancers:_________ Sensitivities to foods _________________ Infection Fatty Liver Reflux/GERD Colitis Urinary: Urinary loss of control Incomplete emptying Difficulty urinating Urinary frequency Kidney Stones Urinary Infections Chronic Kidney Disease Muscles/Bones: Muscle aches/weakness Osteoporosis Neuro: Loss of consciousness Weakness Joint pain Back pain Numbness Seizures Dizziness Psychiatric: Depression Schizophrenia Headaches Stroke Anxiety Hair falling out Chronically tired Thyroid Disease Reproductive Problems Diabetes Multiple Sclerosis Sleep disturbances Mania Feeling unsafe in a relationship Anorexia Bulemia Endocrinology: Increased thirst Alcohol abuse Increased hair growth Pituitary Problems Adrenal Problems Hematology: Swollen glands Bruising Bleeding problems Anemia (low red blood cell count) Low platelets High/low white blood cells Blood Cancers HIV+ Blood transfusions STD Skin/Allergy: Skin rashes Jaundice Eczema Bruising Itching Hives Sneezing