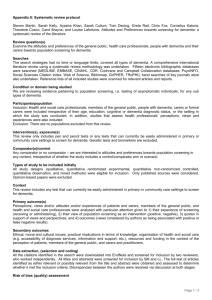
Student Information Pack

T Y S IRIOL U NIT
County Hospital
Coed-y-Gric Road
Griffithstown
Bwrdd lechyd
Aneurin Bevan
University
Health Board
T
Y
S
IRIOL
U
NIT
County Hospital
Coed-y-Gric Road
Griffithstown
Pontypool
NP4 5YA
D
EPARTMENT OF
P
SYCHIATRY FOR
O
LDER
A
DULTS
Tel: 01495 765773 Fax: 01495 765791
STUDENT INTRODUCTION PACK
Please accept a warm welcome from the staff at Ty Siriol and we hope you enjoy your placement with the Community Mental Health Team.
During this experience you will be given the opportunity to gain firsthand knowledge of the day to day work carried out within the team.
Depending on your level of experience and under the supervision of a qualified nurse you will be involved in assessing risk, care planning, evaluations and patient reviews. Within the CMHT we have an allocated emergency responder system where an allocated Community Psychiatric
Nurse make themselves available to respond to any urgent referral that comes in via our duty desk. Members of the team also make themselves available for out of hour’s visits with our Medical staff.
On arrival you will be allocated a mentor who will be responsible for all your educational needs during your time with us. You will be encouraged to become involved in the daily practice of the team which should enable you to fulfil the requirements of the placement.
During your time with us we hope that you will take advantage of the learning opportunities we have to offer. You will soon realise that the
CMHT is only part of the process and that there are many other departments involved in the care of older adults within Torfaen. We would hope that you will take advantage of this, and arrange to spend time with other professionals within Ty Siriol.
We are involved in the care of both Organic and Functional illnesses and also offer support to carers during this difficult period of their lives.
The aim of the CMHT is to provide patient centred care, treating each person as an individual, taking into account their physical, social, psychological, spiritual and cultural needs. Promoting independence wherever possible, freedom of choice, dignity and respect all form part of the ethos of the CMHT. We aim to treat people how we ourselves and our relatives would expect to be treated. We work closely with relatives and families in the delivery of care to our patients.
T HE MEMBERS OF THE C OMMUNITY M ENTAL H EALTH T EAM ARE :-
C
ONSULTANT
P
SYCHIATRIST
D R V B APUJI R AO
A
SSOCIATE
S
PECIALIST
D
R
M K
YAW
C
ONSULTANT
C
LINICAL
P
SYCHOLOGIST
D
R
J
IMMY
J
ONES
S
ENIOR
N
URSE
D
AWN
M
ORGAN
T
EAM
M
ANAGER
D AVID E DWARDS
H
OSPITAL
L
IAISON
A NDY H AMILTON
I N R EACH T EAM
D EBBIE P OWELL
S ARAH E VANS
C
OMMUNITY
O
CCUPATIONAL
T
HERAPIST
S ARAH Y OUNG
C
OMMUNITY PSYCHIATRIC NURSES
(CPN’S)
K AY D ESMOND
B RYAN D AVIES
C ERI M ORGAN
D AVID P HILPOTT
C HRIS R EES
C
OMMUNITY PSYCHIATRIC NURSING ASSISTANTS
(CPNA’
S
)
J AN C OLLIER
S UE E VANS
K AY S HORTHOUSE
M
EMORY
A
SSESSMENT
S
ERVICE
T
EAM
K EVIN J AMES ( MANAGER )
K EITH W HEELER (D EMENTIA C O ORDINATOR )
K IM E VANS (R EGISTERED N URSE )
S HELIA G INGELL (R EGISTERED N URSE )
A NNE W ITCHARD (R EGISTERED N URSE )
G AIL H ERN ( MAS HCSW)
Community Mental Health Team
The CMHT is primarily a secondary care service consisting of 4.6 Band 6
CPN’s one of whom is a nurse prescriber and is supported by the CPNA’S who also carry a caseload and provide support for our Memory assessment services. We provide a service between the hours of 08.30 and 16.30 hours Monday to Friday. Our emergency responders work from 09.00 to 17.00 hrs to correspond with Duty Desk.
Community Nurses conduct assessments and offer help to people primarily in their home environment, but people living in the Torfaen area may also be seen at the team base at Ty Siriol Hospital. The community nurse role is to support and counsel patients through periods of declining mental health, to provide a range of specific psychological therapies and to administer certain types of medication and monitor its subsequent affect. They also monitor the mental state of the patient who has been identified to be at risk of relapse, self neglect or self harm. A collaborative care approach is central to the CPN role, this encourages the patient and others involved with that person to have fuller participation in their programme of care.
CPNA’s
We have three CPNA’s attached to our team who work under the supervision of the qualified team members. Most frequently, support workers were engaged in social and practical support; for example, accompanying clients on shopping trips to build their confidence, or assisting with household management matters. Occasionally they had also been called upon to provide short periods of concentrated input, visiting a client several times per week to avert a breakdown or crisis, before the situation was reappraised. However, their roles continue to develop and we are in the process of looking at utilizing their expertise in the nursing / residential homes and in MAS. There is an eagerness to
assert their intended role in intensive interventions thus supporting our colleagues with difficult clients in the community.
Service Description
The Older People’s Community Mental Health Team offers assessment, diagnosis, treatment and support for people over 65 who present with functional mental health illnesses; deterioration in cognition and/or dementia. Access to the service is via a single point of access, whereby all referrals are discussed by the multi-disciplinary team and the most appropriate range of assessment/treatment and support offered. Within the team we have a medical team, mental health nurses, occupational therapists, psychologists, social care practitioners and support workers.
The team works closely with other Statutory Services, Care and also with the voluntary sector, particularly the Alzheimer’s Society to provide positive support for people using services and their carers ensuring effective forward signposting where appropriate. A range of options are available depending on the needs of the person using services, these options will be discussed fully with individuals who present to these services.
Referral Process
We accept written referrals from GPs, virtual wards, and other secondary care services all of which are screened and logged via duty desk. Once screened all referrals for our Memory Assessment service goes directly to them for discussion at their MDT. All other referrals are discussed at the main MDT and allocated accordingly. Referrals from other agencies are via GP. Individuals can self refer back to the service for up to 3 years following discharge under part 3 of the Mental Health
Measure.
Referral Criteria
The service accepts referrals for people over 65 with concerns about their memory, including mild cognitive impairment, functional mental health problems (for example depression, anxiety, psychosis, bipolar disorder) whose needs cannot be met in Primary Care. We are also seeing an increasing number of younger people with a cognitive impairment coming through our memory clinics which I’m sure will require support from secondary care services in the immediate future.
T
Y
S
IRIOL
U
NIT
Ty Siriol unit provides a range of services and provisions for mental health patients including a memory assessment services, psychology, social workers, Occupational Therapy both community and ward based and a Community Mental Health Team with emergency responders.
Listed below are other areas and disciplines you may wish to arrange time with during your stay with us:-
M
EMORY
A
SSESSMENT
S
ERVICES
Torfaen Memory Service is an organic mental health service that operates on a referral only basis, whereby referrals are generally received from a patients G.P. Through the use of a number of established assessment tools, the service aims to highlight possible memory problems currently experienced by patients, and enable the successful diagnosis of possible conditions and the successful establishment of appropriate medication therapy by our experienced medical team.
Our team currently consist of a manager, staff nurses, a dementia care coordinator and experienced nursing assistants. Clinics generally operate 3 day a week - Mondays, Wednesdays and Fridays. Multidisciplinary team (MDT) meetings are held on a Thursday, which generally enable the collaboration of disciplines to identify patient needs, problem solve and generally work together to ensure a holistic approach to care is executed. There will be an opportunity for you to attend these meetings, enabling an observational insight into the management of patients for which the service is provided. Within the clinic, E.C.G’s, blood pressure and bloods are taken from new patients to the service, which provide general baseline information, and enable an opportunity to identify any possible physical issues that could contribute towards possible memory problems. This ensures correct and effective diagnosis can be made, and appropriate treatment can be undertaken to best meet the needs of the patient.
H
AFAN
D
EG
W
ARD
Hafan Deg Ward consists of 19 acute beds, 6 are for frail adults with functional mental health issues whilst 13 beds are for the treatment of older adults with an organic mental health illness.
Functional mental health issues can be defined as relating to a mental health illness such as schizophrenia or depression, an individual’s day to day functioning may be temporarily affected due to mood but there is no physiological reason for loss of functioning.
Organic mental health issues can be defined as physical changes occurring in the brain due to a dementia type illness that causes impairment to functioning and day to day activities.
Clinical Psychology
Jimmy Jones is our Clinical Psychologist who will provide a range of assessments which include neuropsychological assessment (usually requested via Torfaen MAS), assessments to aid diagnosis or as a second opinion, assessment of mental capacity for specific decisionmaking, assessment of patients referred for psychological therapy.
The Clinical Psychologist sees patients both in and out of the hospital setting. Clinical Psychologists have a broad psychological training and are able to draw from a multiple theoretical base to help the patient, their GP and key worker within the team, to gain a clear psychological understanding of the patient’s difficulties. They assist the patient by devising an individual programme to their needs. This may involve the use of a combination of different psychological therapies to help a given individual. Clinical Psychologists therefore work through the most complex and severe cases. The team Psychologist also offers a consultancy service for professionals within the Torfaen Community
Mental Health Team, providing advice, support and/or supervision and a psychological management of their patients. Staff training on specific psychological approaches can also be provided.
H
OSPITAL
L
IAISON
The Torfaen CMHT psychiatric Liaison service comprises of one full time
Band 6 Nurse. The Liaison Nurse provides a service to older people with mental health problems within Nevill Hall Hospital and the local district general hospitals, namely County hospital Pontypool and on occasions the Liaison Nurse may be called upon to visit Ysbyty Aneurin Bevan,
Ebbw Vale and Ysbyty Ystrad Fawr in Ystrad Mynach.
This service provides assessment and or treatment with additional support/advice to other healthcare professionals involved in the care of
the specified client group. Following assessment a programme of care is developed identifying priorities and realistic goals involving patient’s relatives and the multidisciplinary team. The Liaison Nurse works closely with this programme of care is evaluated following implementation.
Nursing/Residential Home In Reach Team
The Torfaen CMHT In Reach Liaison service is presently a job share and comprises of one part time Band 7 and a part time Band 6 nurse. The In
Reach team provide information and advice to the homes in our catchment area. They are involved in the instigating of cases for more appropriate placements if a person is out of category and the home can no longer meet their needs. This often leads to their involvement in the
Continuing Health Care process. They help to improve direction on clinical pathways offering advice and support when needed. They have medical support provided by Dr Kyaw who has one session per week with the team.
Occupational Therapy
The occupational therapy team consists of:-
One full time community O.T. who has responsibility for the assessment and treatment of individuals over 65 years with a mental health problem or dementia. The community O.T. also provides a service to the Torfaen
Memory Clinic. Most O.T. assessments and treatment programmes are carried out in the clients own home often with support of their family or carer. One full time ward based O.T. who has responsibility to deliver an
O.T. service to Hafen Deg assessment ward. The ward is divided into six beds for the assessment and treatment of in-patients with an acute mental health problem and thirteen beds for the assessment and treatment of patients acutely ill due to their dementia. The ward O.T. takes responsibility for discharge planning, assessment of patient’s functional ability and an individual treatment plan for the improvement or maintenance of function during the hospital admission.
One full time O.T. technician who supports the ward and community
O.T.s to carry out individual and group programmes of activity designed by the qualified O.T.s to improve or maintain function. Also to work autonomously to encourage independence and prevent dependency during the in-patient stay.
Gwent Frailty/Community Resource Team
Gwent Frailty brings together Health and Social care across the regions of Gwent in an integrated approach focussing on providing short term intervention and support for frail vulnerable people to remain happily independent as possible at home or within the community.
The team provides services 8am to 8 pm seven days a week for a range of health needs, including assessment and treatment of acute conditions and active management of chronic conditions. The team comprises of
Rapid Response, Reablement, Falls Team, a Specialist Mental Health
Practitioner, Emergency care at Home of multi-disciplinary staff including Nurses and Medical Staff, Occupational Therapists,
Physiotherapists, Support /Health and Wellbeing Workers , Social
Workers and Administrative staff. The integrated nature of the team allows the service to maximise possible positive impact on the individual’s unique health and well being working closely with other
Services and Agencies to ensure person and their family are placed at the centre of appropriate care delivery.
All referrals must be to be made via the Single Point of Access SPA
0845 601 6363
Frailty aims to:-
Ensure patients have access to the right care at the right time.
Focus on preventative care, wherever possible avoiding unnecessary hospital admission.
Reduce length of hospital stay when admission is necessary.
Reduce need for complex care pathways.
Avert crises by providing the right amount of care when needed.
The Torfaen Specialist Mental Health Practitioner within Frailty (SMHP) offers short term advice, support, assessment, intervention and signposting to help people experiencing mild to moderate mental health difficulties who meet the specific eligibility criteria. The SMHP aims to work collaboratively with all Frailty multi disciplinary staff, other
Primary care colleagues and the Secondary Mental Health Services to work together to deliver effective, comprehensive short term care.
The SMHP only receives referrals internally from Frailty Staff and if the individual is not already receiving care from Secondary Mental Health
Services, unless referred for adjunctive short term support from the
Older Adult Mental Health Team. The SMHP will signpost appropriately to Ty Siriol and attend CMHT’s when necessary.
Social Services
The Mental Health Team are base here at Ty Siriol and are our link to social care provision for our client group. There are a number of AMP’s
(Approved Mental Health Professional’s) within the team who are trained to implement elements of the Mental Health Act (1983), as amended by the Mental Health Act (2007).
The Mental Health team are generally involved in the more complex cases that require their expertise. The less complex cases remain with the Older Adult Team who we also work closely with the regularly attend our MDT’s to discuss Patients we have in common.
Carer Support Groups
We run a number of carer support groups from Ty Siriol and Keith
Wheeler our Dementia Care Coordinator is at the forefront in providing this valuable resource. He is involved in the running of the Dementia
Carers Educational Support Course which helps carers in developing coping strategies when caring for a loved one with Dementia. Keith also supports carers groups outside Ty Siriol and I’m sure he would be delighted to discuss these with you during your stay.
DEMENTIA CARERS EDUCATIONAL AND
INFORMATION SUPPORT COURSE
What are carers educational/information support course?
Dementia is a chronic condition that more often than not adversely has an impact on family carers.64% of carers have identified that lack of support is a contributing factor to poor health. (Carer’s Wales 2012.)
However, the information and support needs of carers often go unrecognised. This is acknowledged in various government documents recommending the need to provide carers with information advice and support; however this does not always translate into practice.
Why was the course set up?
There were several reasons for setting up Torfaen’s first Dementia course. First by the compelling evidence base, research has thus shown that carers needs include, information support, and contact with other carers, in an empathic setting. Secondly through clinical work we were finding that carers were asking for more advice on the illness, its progression and how to manage symptomsThe review to the NSF for older people in Wales published in 2012 through the lens of someone with dementia reports” carers we spoke to sometimes felt forgotten and struggled to get agencies to communicate and coordinate with them”
The Dementia intelligent targets, aims to support carers and advocates the use of multi component carer support programmes and that training for carers to be available on a regular basis. The carers Wales strategy
2011 places a responsibility on ABUHB to deliver effective relevant up to date and targeted information to carers. There was a clear link between the strategy action plan and dementia intelligent targets for carers.
Setting up the course
The course runs every Thursday afternoon 2 till 4 .Between 8 and 19 carers attend each session. We aim to run 4 courses yearly. We allow half an hour for carers to arrive have a chat with refreshments before the session starts at 2 30.Many carers use this time to catch up with each other or members of staff. Most carers are identified via the post diagnostic work undertaken by TMC staff. The sessions are jointly facilitated by the Clinical Psychologist Dementia Service Coordinator and the TMC Nurse Manager.
Format of the sessions
The course runs for 8 weeks and each week a different topic is covered.
Although the topics are set there is room to accommodate arising advice or support needs. Topics covered are:-
Week 1. Introductions, course content and discussion around the different types of dementia. Also how the diagnosis is made.
Week 2. Links to this in addressing the understanding off and managing symptoms.
Week 3. Carers rights, carer assessments and overview of benefit entitlements.
Week 4. Medical information and drug treatments.
Week 5. Legal issues, LPA and capacity assessments.
Week 6. Telecare creating safe environments.
Week 7. Meaningful activities and person centred care.
Week 8. Ongoing support representative from the Alzheimer’s society.
Each week a specialist in that topic area, a psychiatrist, occupational therapist, legal adviser, social worker and assistive technology manager are invited to present.
We keep the sessions as informal as possible .We have noted empathic listening produces closeness in the group. Some of the sessions can be very moving with a mixture of tears laughter and resilience when sharing experiences, there is a natural empathy.
After the session is over invariably discussion takes place involving carers and staff, often in preparation for the next session.
Is it useful? The carers perspective.
At the end of each course we carry out a questionnaire. See appendix
1.The overwhelming consensus is the course is of great benefit to cares in developing peer support, acquiring knowledge of support services and developing coping strategies in caring for someone with dementia.
Some of the comments from cares include “I really enjoyed it and learned a lot” also “It was a good opportunity to get advice from professionals and to meet others with similar worries and experiences all in a friendly atmosphere”
The future
Given the positive feedback and attendance we intend to continue this service provision. From this group a carers information leaflet has been produced .To enable the support to be continued a weekly dementia support group held at the local carers centre has been set up with regular updates from some of the presenters.
An ABHB working group has been set up to look at replicating the course. This simple yet innovative provision has been enthusiastically received by carers and has been running since August 2011.Such a course could be replicated across other services.
Cognitive Stimulation Therapy Groups
We are providing twice weekly CST Groups which is a stimulating programme for use with people suffering with Dementia. CST is designed to run for seven weeks providing a person centred approach which is both inclusive and stimulating.
What is expected of our Student Nurses?
There are a number of opportunities available to you as a student nurse within our service. First and foremost, we expect you to observe and
gain an understanding of what the service is, what it achieves and how it works. We actively encourage development, so if there is anything that you are unsure of, anything that you are particularly interested in or anything you need explained – just ask! There are a number of resources within the unit, which you are welcome to use to enhance understanding and knowledge!
If there is anything that you feel could prove beneficial to you, or anything that you feel you would benefit from undertaking – speak to us. This placement is your opportunity to learn as much as you can from the experience, and we actively encourage you to source and identify areas that will enhance your learning and development.
Our Expectations of You …
Be polite and professional at all times. We provide a service for very vulnerable people, and ask that you respect the need for professionalism, and the compliance with confidentiality at all times.
Adhere to the policies and procedures that govern the practice area. These are available using the Aneurin Bevan Health Board staff intranet, which you are able to access on one of the office computers.
If you are running late, we would appreciate a phone call just so that we know your ok.
If you are ill, please follow your individual university policy of contacting us (we will only worry!), and contacting the sick line as required by the school.
Other Useful Information
Forms Of Dementia
Alzheimer’s Disease
Alzheimer’s disease was first described by Dr Alois Alzheimer around 1907. It is an irreversible disease due to the degeneration of brain cells. There is impairment of memory, judgement and orientation, together with physical, emotional and personality changes.
There is a degree of brain ‘shrinkage’ due to nerve cell atrophy
(wasting away).
Senile plaques are formed. Exactly what they are is uncertain but they appear to represent collections of degenerating brain substance or fine nerve tangles or filaments. This disrupts the passage of neurochemical signals, which in turn leads to memory loss or impaired thought process.
There is also a depletion of acetylcholine, which is a neurotransmitting brain substance.
Vascular Dementia
Vascular dementia is widely considered to be the second most common type of dementia. It develops when impaired blood flow to parts of the brain deprives cells of food and oxygen.
The diagnosis maybe clearest when symptoms appear soon after a major stroke blocks a large blood vessel, and disrupts the blood supply to a significant portion of the brain.
There is also a form in which a series of very small strokes or infarcts, block small blood vessels. Individually these strokes do not cause major symptoms, however over a period of time their combine’s effect becomes noticeable.
The person may have a past history of heart attacks. Within cases of; high blood pressure, high cholesterol, hardening of the arteries, diabetes or other risk factors, heart disease is often present.
Memory problems may or may not be a prominent symptom, depending upon the area of the brain affected. Physical symptoms associated with strokes include weakness, difficulty with speaking and confusion.
Lewy Body Dementia
Lewy Body disease is a dementia caused by damage to the brain.
It is similar to Alzheimer’s however symptoms are typically different.
The disease gets its name as a result of the abnormal deposits of a protein called alpha-synuclein, which are found in the body following death. Lewy Body are round deposits which contain damaged nerve cells.
Lewy body dementia affects; memory, language, ability to judge distance, ability to carry out simple actions, the ability to reason.
People with this particular form of dementia additionally suffer with hallucinations.
The abilities of the affected person often fluctuates form hour to hour, and over weeks and months. This sometimes results in carers believing that the patient is ‘putting on’ their confusion.
Creutzfeldt - Jakob disease (CJD)
CJD was first reported in 1920 and commonly effects people over the age of 55. It is one of the small group of fatal diseases caused by the infectious agent which invades the brain and causes mental and physical collapse. This agent may exist within the body for a number of years before symptoms begin, however death may result within a year.
Differing forms of this disease exist in humans and animals, but all result in spongiform encephalopathy, so called because areas of the brain where the cells have died, appear like a sponge under the microscope.
Picks Disease
Picks disease is a cause of dementia similar to Alzheimer’s
Disease. It occurs less frequently and takes effect between the ages of 40-65. Damage is more localised and effects personality and behaviour more commonly than memory.
Frontal Lobe Dementia
This is the name given to any dementia caused by damage to this particular part of the brain. The individual’s mood and behaviour may become fixed and difficult to change, making them appear selfish and unfeeling.
The affected individual usually does not have the sudden memory lapses, which are characteristic of Alzheimer’s Disease.
Dementia Medication
There are 4 types of drugs used within dementia management;
Donepezil / Aricept
Rivastigmine / Exelon
Galantamine / Reminyl
Memantine / Ebixa
Aricept, Exelon and Reminyl are known as cholinesterase inhibitors. This group of drugs work by reducing the breakdown of acetylcholine within the brain.
Acetylcholine is a chemical substance that occurs naturally within the brain, and enables brain cells to pass messages to each other.
Research has shown that many people with dementia have a reduced amount of acetylcholine.
Memantine / Ebixa
NMDA (N-Methyl-D Aspartate works differently to other drugs, in the way that it works to modify the function of the nmda receptor.
This is involved with the chemical transmitter glutamate and research suggests that too much glutamate is damaging or toxic to the nerve cells. It is the first drug available to people in the latter stages of the disease. Other treatments – complementary and alternative medications include;
Vitamin E
Ginko Bilboba – which improves cerebral blood flow
Good Diet – Stabilising weight, minimising weight fluctuations, prevents falls.
It is important to realise that these drugs are not a cure and can only stabilise some of the presenting symptoms for a limited time.
Side effects may include;
Diarrhoea
Nausea
Insomnia/Vivid Dreams
Fatigue
Poor Appetite.
Electro Convulsive Therapy
Occasionally we will have patients admitted to the ward who are undergoing a course of Electro Convulsive Therapy (ECT). These treatments take place at Maindiff Court Hospital, Abergavenny. If the opportunity arises you may be able to attend a treatment and follow a patient’s care whilst undergoing ECT, this is a valuable learning experience.
Assessment Tools
Addenbrookes
Addenbrookes Guide
WARRN(Wales Applied Risk
Research Network)
Addenbrookes
Assessment tool.pdf
Addenbrookes guide.pdf
WARRN.doc
CTP Front Sheet
01. CTP Front
Sheet.doc
CTP Assessment
02. CTP
Assessment.doc
Care and Treatment Plan
03. Care and
Treatment Plan template.doc
Assessment Report
04. Summary assessment report.doc
Care & Treatment Plan
Amendments
05.
Amendements.doc
Discharge from Secondary
Mental Health Services
Continuing NHS Healthcare
The National Framework for
Implementation in Wales
CHC Decision Support Tool
06. Discharge Care
Plan.doc
Continuing NHS
Healthcare The National Framework for Implementation in Wales 2014.pdf
Capacity Assessment Form
Decision support tool for NHS continuing healthcare Wales 2014 - WORD WITHOUT Text Boxes.docx
MCA Capacity
Assessment and Best Interests Record Form.doc
Nursing Assessment for
Placement
Nursing Assessment
Blank.doc
Location of Policies, Procedures & Guidelines
These can be accessed via the Trust intranet on the computer and also in the Policies and Procedures file kept in the nursing office.
Clinical Nursing Procedures can be studied using the Royal Marsden
Hospital Manual, a copy of which is kept in the nursing office.
Current NMC guidelines can also be accessed on the computer.
Please see Policies below all of which may be of help to you during this placement……….
CMHT Operational Policy
CMHT Operational
Policy 2014.docx
Lone Worker Policy
ABHB_H&S_0434
Lone Working Policy and Guidance_Issue 2.pdf
Consent Policy
ABHB0004 Consent
Policy - Issue 1 (3).pdf
Mental Capacity Key Principles
MCA Key
Principles.pdf
Assessment of Mental Capacity
ABHB_Clinical_0168
Assessment of Mental Capacity Procedure_Issue 2.pdf
Mental Capacity & DoLS Policy
ABHB0275 Managing
Authority Policy Proecdure for MCA 2005 DoLS - Issue 1.pdf
Section 117 Procedure
ABHB_MHLD_0593
Gwent Section 117 Procedure_Issue 1.pdf
Medicines Management Policy
ABHB0010 Medicines
Management Policy - Issue 3.pdf
Medication Administration in
Community Settings using
(MAR)
ABHB_Clinical_0616
Medication Administation in Community Settings using MAR LES Policy_Issue 1.pdf
Use of Injectable Drugs Policy
Depot Medication
Guidance for the Management of Confused Older Adult Patients in General Hospital Settings
Safer Manual Handling Policy
ABHB_Clinical_0099
Use of Injectable Drugs Policy_Issue 1.pdf
Depot
Medication.docx
GHT DIV 6037 MH
LD - Guidance for Confused Older Adult - Issue 4.pdf
ABHB_H&S_0231
Safer Manual Handling Policy_Issue 5.pdf