ONLINE SUPPLEMENTAL MATERIALS Glossary Unless otherwise
advertisement

ONLINE SUPPLEMENTAL MATERIALS
Glossary
Unless otherwise specified, all units of pressure, volume, flow, time, weight, and
resistance are in mmHg, mL, mL/s, seconds, kilograms, and mmHg s mL-1, respectively.
Pressure references mentioned in the paper are as labeled in Online Figure 1.
BSA
Body surface area in m2
HR
Heart rate in beats per minute
LPN
Lumped-parameter network
MET
Metabolic equivalent in units of 3.5 mL-O2 kg−1min−1
Sinit
Scaling factor of the initial pressures and volumes in Online Table 2
tsvs, tc
Systolic and cardiac time period
Vsv, Vsa, Vsvo, Vsao
Ventricular and atrial volume and reference volume
TVR, SVR, PVR
Total, systemic, and pulmonary vascular resistance
Section A: Lumped-parameter Network
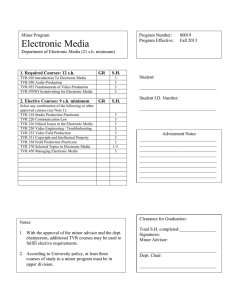
Online Figure 1 shows the lumped-parameter network (LPN) we use to model the Fontan
circulation 13. The LPN consists of several major blocks describing the atrium, ventricle, upper
body, lower body, and pulmonary circuits. The lower body block consists of circuits describing
the major blood vessels, abdominal organs (liver, kidneys, and intestine), and legs. The heart
blocks and the intrathoracic pressure (Pith) generate active pressure sources for the system, where
the rest of the circuit is made up of passive elements including resistances, compliances,
inertances, and diodes, which model the viscous vascular resistance to flow, compliance of blood
vessels, momentum of flowing blood, and venous valves, respectively. Each compliance and
inertance element is governed by a differential equation:
𝑄=𝐶
𝑑𝛥𝑃
𝑑𝑡
𝛥𝑃 = 𝐿
𝑑𝑄
𝑑𝑡
where C, L, ΔP, Q are the compliance value, inertance value, pressure drop across the element,
and flow into the element, respectively.
We implemented a time-varying elastance approach23 using a ratio between the transmyocardial ventricular pressure and ventricular volume (ie. elastance) which varies over the
cardiac cycle to model the ventricular contraction. A normalized elastance waveform was
constructed based on the data from Senzaki et al. 20 with smoothing applied to the diastolic part
of the waveform to remove any ripples that were likely due to low signal-to-noise ratio in the
experimental measurements. The waveform is zeroed according to the value at the onset of
systole and normalized to its peak, which is a similar approach that has been utilized in previous
ventricular model implementation19. The equation below describes the mathematical
construction of the normalized elastance function, using the k-th coefficients “Cr” and “Ci” listed
in the Online Table 1.
19
𝐸𝑛(𝑡) = ∑{𝐶𝑟𝑘 cos(2𝜋𝑘𝑡) − 𝐶𝑖𝑘 sin(2𝜋𝑘𝑡)}
𝑘=0
Un-normalizing the waveform returns a simulation-specific elastance curve:
𝐸𝑜𝑓𝑓𝑠𝑒𝑡 ,
𝐸(𝑡) = {
𝐸𝑚𝑎𝑥 𝐸𝑛 (0.3
𝑡
𝑡𝑠𝑣𝑠
) + 𝐸𝑜𝑓𝑓𝑠𝑒𝑡 ,
𝑡 > 3.33 𝑡𝑠𝑣𝑠
𝑒𝑙𝑠𝑒𝑤ℎ𝑒𝑟𝑒
where En(t) and E(t) are the normalized and un-normalized time-varying elastance, Emax and
Eoffset are constants reflecting measures of contractility and ventricular filling, respectively, and
tsvs is the length of the systolic time period. Note that 0 ≤ t < tc, where tc is the cardiac period.
The trans-myocardial ventricular pressure is then given by:
𝑃𝑡𝑠𝑣 (𝑉𝑠𝑣 , 𝑡) = 𝐸(𝑡)(𝑉𝑠𝑣 − 𝑉𝑠𝑣𝑜 )
where Vsv and Vsvo are the ventricular volume and reference volume, respectively.
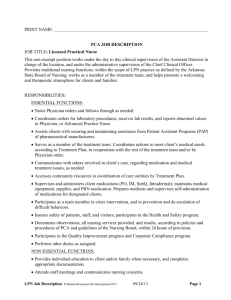
The atrial behavior is modeled using a combination of a passive pressure-volume
relation, an active pressure-volume relation, and an activation function3,14,21. The passive
behavior describes the passive compliance of the atrial wall and how it responds to filling; the
active behavior captures the effect of the Frank-Starling mechanism; and the activation function
simulates atrial wall depolarization which determines the contribution of the active behavior to
the overall atrial pressure. The atrial activation function is a construction of piecewise cosine
functions as shown in Online Figure 2a, and described by the equation6,12:
1
𝑡−𝑡1 +𝑡𝑠𝑎𝑠
1
𝑡𝑠𝑎𝑠
𝑡−𝑡𝑠𝑎𝑑 −𝑡1
[1 − cos (2𝜋
2
𝐴𝐴(𝑡) =
2
[1 − cos (2𝜋
𝑡𝑠𝑎𝑠
)] , 𝑡 ≤ 𝑡1
)] , 𝑡1 + 𝑡𝑠𝑎𝑑 ≤ 𝑡 < 𝑡𝑐
0, 𝑒𝑙𝑠𝑒𝑤ℎ𝑒𝑟𝑒
{
where t1=0.2 tc, and tsas= 0.9 tsvs.
The active and passive pressure-volume relations are described by the equations:
𝑃𝑠𝑎,𝑎𝑐𝑡𝑖𝑣𝑒 =
𝑉𝑠𝑎 −𝑉𝑠𝑎𝑜
𝐶𝑠𝑎
𝑃𝑠𝑎,𝑝𝑎𝑠𝑠𝑖𝑣𝑒 = 𝑃𝑠𝑎𝑟 {𝑒 𝐷𝑠𝑎 (𝑉𝑠𝑎−𝑉𝑠𝑎𝑜 ) − 1}
where Vsa and Vsao are the atrial volume and reference volume, respectively. Csa, Psar, and Dsa
are constants which reflect atrial wall and contractile properties.
The trans-myocardial atrial pressure is then given by:
𝑃𝑡𝑠𝑎 (𝑉𝑠𝑎 , 𝑡) = 𝑃𝑠𝑎,𝑎𝑐𝑡𝑖𝑣𝑒 𝐴𝐴(𝑡) + 𝑃𝑠𝑎,𝑝𝑎𝑠𝑠𝑖𝑣𝑒
Blood flow through the atrial-ventricular and aortic valves is described by the following
equations 18:
𝑑𝑄𝑎𝑣
𝑑𝑡
0, 𝑃𝑠𝑎 < 𝑃𝑠𝑣 𝑎𝑛𝑑 𝑄𝑎𝑣 ≤ 0
= {𝑃𝑠𝑎 − 𝑃𝑠𝑣 − 𝐾𝑎𝑣𝑄𝑎𝑣2
, 𝑒𝑙𝑠𝑒𝑤ℎ𝑒𝑟𝑒
𝐿𝑎𝑣
𝑄𝑎𝑜 = {
0,
𝑃𝑠𝑣 < 𝑃𝑎𝑜
1
√4 𝐾𝑎𝑜 (𝑃𝑠𝑣 − 𝑃𝑎𝑜 ),
2 𝐾𝑎𝑜
𝑃𝑠𝑣 ≥ 𝑃𝑎𝑜
where the terms in these equations are defined in the glossary, Online Figure 1, and Online Table
2.
In the case of AV valve insufficiency, the backflow through the AV valve during systole is
described by the equation:
𝑄𝑎𝑣 = −√
𝑃𝑠𝑣 − 𝑃𝑠𝑎
𝑅𝑎𝑣
where Rav is the regurgitation valve resistance.
We approximate the time-varying intrathoracic pressure due to breathing using a
piecewise cosine waveform as shown in Online Figure 2b. The intrathoracic pressure acts as an
extravascular pressure to the large blood vessels in the thorax, the pulmonary vasculature, and
the heart, and thus is connected to the corresponding elements in the LPN.
The system of algebraic and ordinary differential equations derived from the LPN is
solved using a fourth order Runge–Kutta method implemented in a custom Fortran code.
Section B: Exercise & Body-size Dependent Parameters
Parameter values are defined according to exercise intensity and patient body size.
Exercise intensity is expressed in terms of metabolic equivalent (MET), where 1 MET is defined
as an oxygen consumption of 3.5mL O2·kg−1·min−1. Inputs of patient height in centimeters, and
weight in kilograms, return the body surface area (BSA) in square meters via the commonly used
clinical equation:
𝐻𝑒𝑖𝑔ℎ𝑡∗𝑊𝑒𝑖𝑔ℎ𝑡
𝐵𝑆𝐴 = √
3600
(1)
Using clinical data collected in 9 Fontan patients who underwent exercise testing 9, we
established correlations between exercise intensities and HR, total vascular resistance (TVR),
and aortic pressure. We identified mathematical fits to the clinical data and derived the
following relationships:
𝐻𝑅 =
1
𝑊𝑒𝑖𝑔ℎ𝑡 0.25
(212.4 𝑀𝐸𝑇 0.3016 )
(2)
1
𝑇𝑉𝑅 = 𝐵𝑆𝐴 (−8.882 ln(𝑀𝐸𝑇) + 33.00)
(3)
Using the same clinical data, we also provide the correlation (R2=0.87) between exercise
levels expressed in terms of MET versus power to weight ratio (PWR) in watts/kg to enable
translation between the two common measures of exercise level, allowing other investigators to
utilize the methods presented in this study in wider ranges of scenarios.
(4)
𝑀𝐸𝑇 = 3 𝑃𝑊𝑅 + 1
The pulmonary vascular resistance (PVR) in Fontan patients affects the pressure
measured in the Fontan pathway, and has been speculated to be an important factor limiting
exercise tolerance8,10. Using previous literature data22, we define a relationship between the
change in TVR (relative to resting condition) due to exercise, and the corresponding change in
PVR:
𝑃𝑉𝑅𝑓 = 0.4329 ln(𝑇𝑉𝑅𝑓) + 1
(5)
where PVRf and TVRf are the factors that scale the resting values of PVR and TVR,
respectively, to their corresponding exercise values.
The systolic time interval (tsvs) is one of the parameters used to un-normalize the
elastance function. The systolic fraction is typically one third of the cardiac cycle at rest, and
can increase to about one half of the cardiac cycle at exercise. We implemented the tsvs
calculation based on measurements reported by Gemignani et al. which showed a linear increase
of systolic / diastolic time ratio with HR up to 120 bpm7:
𝑡𝑠𝑣𝑠 = {
[0.5 −
0.2
60
(120 − 𝐻𝑅)] ∗ (
60
𝐻𝑅
60
), 𝐻𝑅 ≤ 120
(6)
0.5 ∗ (𝐻𝑅), 𝐻𝑅 > 120
The Emax parameter is a measure of contractility, which is known to increase with
exercise15. Utilizing reported measurements of Emax made by Alpert et al. in healthy children at
rest and two intensities of exercise1 (which had similar values as those reported by Bombardini et
al.4), and tuning to the cardiac output measurements in our clinical data, we defined the
following equation to describe the value of Emax at different intensities of exercise for different
body sizes:
𝐸𝑚𝑎𝑥 = 𝐵𝑆𝐴 (0.326 𝑀𝐸𝑇 + 1.32)
(7)
The Eoffset parameter dominates the ventricular pressure-volume relationship during
diastole and affects ventricular filling. We defined this parameter using the following equation
to achieve proper filling of the ventricle at various exercise intensities:
𝐸𝑜𝑓𝑓𝑠𝑒𝑡 = −0.016 𝑀𝐸𝑇 + 0.215
(8)
The ventricular reference volume (Vsvo) is a parameter affecting the horizontal location of
the pressure-volume loop. Based on literature data of end diastolic and systolic volume
measurements in humans4,5,16, we define an equation for Vsvo:
𝑉𝑠𝑣𝑜 = 67 𝐵𝑆𝐴 − 100
(9)
Using measurements reported by Grimby et al. of intrathoracic pressure in adult humans
at rest and two intensities of exercise11, we derived equations to describe the amplitude and offset
of the thoracic pressure at different exercise intensities:
𝐴𝑃𝑖𝑡ℎ = −3.9 𝑀𝐸𝑇
𝑃𝑖𝑡ℎ𝑜𝑓𝑓𝑠𝑒𝑡 = 1.92 ( 𝑀𝐸𝑇 − 1) − 3.7
(10)
(11)
These parameters are used to define the thoracic pressure waveform described in the
previous section.
Online Table 2 provides the constant parameter values in the LPN.
Section C: Work Flow for Derivation of LPN Parameter Values
This section describes the work-flow for deriving a full set of LPN parameters to perform
simulation representing any particular combination of patient body-size and exercise intensity.
Tuned based on previous LPN modeling work 6,12, Online Table 3 lists a set of generic reference
values serving as the starting point for the LPN parameters. This generic reference provides the
distributed resistance and compliance values, and initial pressures in the capacitors, to be scaled.
Using Online Table 3 together with equations in section B, we derive the parameters needed to
fully define a patient-specific simulation of Fontan exercise.
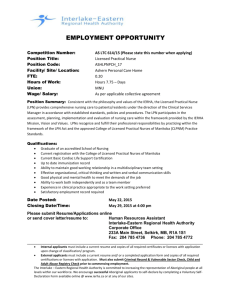
Online Figure 3 shows a flow diagram of the process to appropriately define the
resistance values in the LPN. Entering the BSA and MET levels into Equation 3 enables
calculation of the patient-specific resting and exercise TVR. A network analysis of the LPN
with the generic reference resistances in Online Table 3 returns the generic TVR, which is then
compared to the patient-specific resting TVR (calculated from Equation 3) to return a TVR
scaling factor. The patient-specific resting resistances are then calculated by scaling the generic
resistances by the TVR scaling factor. In addition, using the resting and exercise TVR found
from equation 3, equation 5 returns the PVR scaling factor at exercise. We then scale the
pulmonary resistances in the patient-specific resting resistances according to this scaling factor
and obtain the exercise pulmonary resistances.
The exercise systemic vascular resistance (SVR) is found from the exercise pulmonary
resistances together with the exercise TVR derived from equation 3 (Note that
TVR=SVR+PVR). The resting SVR is found via a network analysis of the patient-specific
resting resistances. The changes in the systemic resistances from resting to exercise are not
uniform across the body, as the cardiovascular system adapts to exercise by increasing flow
specifically to the active muscles, with little to no increase of blood flow to other parts of the
circulation2. The effect of the muscle pump is incorporated as an “effective resistance” of the
relevant circuits, which is greatly reduced from its resting values. To modify the systemic
resistances in our computational model for the exercise condition, we start from the patientspecific resting resistances, and first scale the resistances in the aorta blocks (Rthao, Rabao)
according to the ratio of exercise to resting SVR; we then iteratively scale the leg resistances and
evaluate the SVR via an LPN network analysis, until the desired exercise SVR is achieved.
According to the TVR scaling, we scale all of the compliances to adjust for body size
using the equation 6,12,17:
𝐶
𝐶𝑖
−4
=
𝑇𝑉𝑅 3
𝑇𝑉𝑅𝑖
(12)
where C/Ci and TVR/TVRi are the compliance and TVR scaling ratio. Terms with subscript “i”
indicate the parameter prior to scaling.
According to the resulting scaling of resistances due to exercise, we further scale
compliances in the corresponding blocks using the equation 6,12,17:
𝐶
𝐶𝑖
𝑅
= (𝑅 )
−3
4
𝑖
(13)
where C/Ci and R/Ri are the compliance and resistance scaling ratios, respectively. The
compliances in the leg circuit are not scaled since the exercise “effective resistances” largely
represent the consequences of the muscle pump, rather than vasodilation alone.
Lastly, we scale the initial pressures and volumes in Online Table 3 by the scaling factor
“Sinit” according to exercise level:
𝑆𝑖𝑛𝑖𝑡 = 0.058 𝑀𝐸𝑇 + 0.942
(14)
The remaining parameters of the LPN model are set according to equations 6-11.
REFERENCES
1. Alpert, B. S., L. Benson, P. M. Olley. Peak left ventricular pressure/volume (emax) during exercise in
control subjects and children with left-sided cardiac disease. Cathet Cardiovasc Diagn 7:145-153, 1981
2. Armstrong, R. B., M. D. Delp, E. F. Goljan, M. H. Laughlin. Distribution of blood flow in muscles of
miniature swine during exercise. Journal of applied physiology 62:1285-1298, 1987
3. Avanzolini, G., P. Barbini, A. Cappello, A. Cevese. Time-varying mechanical properties of the left
ventricle-a computer simulation. Biomedical Engineering, IEEE Transactions on:756-763, 1985
4. Bombardini, T., E. Nevola, A. Giorgetti, P. Landi, E. Picano, D. Neglia. Prognostic value of leftventricular and peripheral vascular performance in patients with dilated cardiomyopathy. J Nucl Cardiol
15:353-362, 2008
5. Carroll, J. D., O. M. Hess, H. O. Hirzel, H. P. Krayenbuehl. Dynamics of left ventricular filling at rest and
during exercise. Circulation 68:59-67, 1983
6. Corsini, C., C. Baker, E. Kung, S. Schievano, G. Arbia, A. Baretta, G. Biglino, F. Migliavacca, G. Dubini, G.
Pennati, A. Marsden, I. Vignon-Clementel, A. Taylor, T. Y. Hsia, A. Dorfman, Mocha. An integrated
approach to patient-specific predictive modeling for single ventricle heart palliation. Comput Methods
Biomech Biomed Engin, 2013
7. Gemignani, V., E. Bianchini, F. Faita, M. Giannoni, E. Pasanisi, E. Picano, T. Bombardini. Assessment of
cardiologic systole and diastole duration in exercise stress tests
with a transcutaneous accelerometer sensor. Computers in Cardiology:153-156, 2008
8. Gewillig, M., S. C. Brown, B. Eyskens, R. Heying, J. Ganame, W. Budts, A. La Gerche, M. Gorenflo. The
fontan circulation: Who controls cardiac output? Interactive Cardiovascular and Thoracic Surgery 10:428433, 2010
9. Giardini, A., A. Balducci, S. Specchia, G. Gargiulo, M. Bonvicini, F. Picchio. Effect of sildenafil on
haemodynamic response to exercise and exercise capacity in fontan patients. European Heart Journal
29:1681-1687, 2008
10. Goldstein, B. H., C. E. Connor, L. Gooding, A. P. Rocchini. Relation of systemic venous return,
pulmonary vascular resistance, and diastolic dysfunction to exercise capacity in patients with single
ventricle receiving fontan palliation. Am J Cardiol 105:1169-1175, 2010
11. Grimby, G., M. Goldman, J. Mead. Respiratory muscle action inferred from rib cage and abdominal
vp partitioning. Journal of applied physiology 41:739-751, 1976
12. Kung, E., A. Baretta, C. Baker, G. Arbia, G. Biglino, C. Corsini, S. Schievano, I. E. Vignon-Clementel, G.
Dubini, G. Pennati, A. Taylor, A. Dorfman, A. M. Hlavacek, A. L. Marsden, T.-Y. Hsia, F. Migliavacca.
Predictive modeling of the virtual hemi-fontan operation for second stage single ventricle palliation: Two
patient-specific cases. Journal of Biomechanics 46:423-429, 2013
13. Kung, E., G. Pennati, F. Migliavacca, T.-Y. Hsia, R. S. Figliola, A. Marsden, A. Giardini. A simulation
protocol for exercise physiology in fontan patients using a closed-loop lumped-parameter model. J
Biomech Eng, 2014. DOI:10.1115/1.4027271
14. Lau, V.-K., K. Sagawa. Model analysis of the contribution of atrial contraction to ventricular filling.
Annals of biomedical engineering 7:167-201, 1979
15. Mitchell, J. H. Mechanisms of adaptation of the left ventricle to muscular exercise. Pediatrics
32:660-670, 1963
16. Nevsky, G., J. E. Jacobs, R. P. Lim, R. Donnino, J. S. Babb, M. B. Srichai. Sex-specific normalized
reference values of heart and great vessel dimensions in cardiac ct angiography. AJR Am J Roentgenol
196:788-794, 2011
17. Pennati, G., R. Fumero. Scaling approach to study the changes through the gestation of human fetal
cardiac and circulatory behaviors. Annals of Biomedical Engineering 28:442-452, 2000
18. Peskin, C. S. The fluid dynamics of heart valves: Experimental, theoretical, and computational
methods. Annual review of fluid mechanics 14:235-259, 1982
19. Segers, P., N. Stergiopulos, N. Westerhof, P. Wouters, P. Kolh, P. Verdonck. Systemic and pulmonary
hemodynamics assessed with a lumped-parameter heart-arterial interaction model. Journal of
Engineering Mathematics 47:185-199, 2003
20. Senzaki, H., C. Chen, D. Kass. Single-beat estimation of end-systolic pressure-volume relation in
humans - a new method with the potential for noninvasive application. Circulation 94:2497-2506, 1996
21. Snyder, M. F., V. C. Rideout. Computer simulation studies of the venous circulation. IEEE Trans
Biomed Eng 16:325-334, 1969
22. Stickland, M. K., R. C. Welsh, S. R. Petersen, J. V. Tyberg, W. D. Anderson, R. L. Jones, D. A. Taylor, M.
Bouffard, M. J. Haykowsky. Does fitness level modulate the cardiovascular hemodynamic response to
exercise? J Appl Physiol 100:1895-1901, 2006
23. Suga, H., K. Sagawa, A. A. Shoukas. Load independence of the instantaneous pressure-volume ratio
of the canine left ventricle and effects of epinephrine and heart rate on the ratio. Circulation Research
32:314-322, 1973
ONLINE FIGURE CAPTIONS
Online Figure 1. Closed-loop Lumped-parameter Network of the Fontan Circulation
Rsubscript, Lsubscript, and Psubscript are labels for resistor components, inductor components, and nodal
pressures.
Online Figure 2. a) Atrial Activation Function and b) Intrathoracic Pressure Waveform
Note that values of APith and Pithoffset are typically negative during natural, non-mechanically
ventilated breathing.
Online Figure 3. Flow Diagram for Computing Resistance Values in the LPN
Highlighted items contain the necessary target information for defining all of the resistances in
the LPN for a simulation.
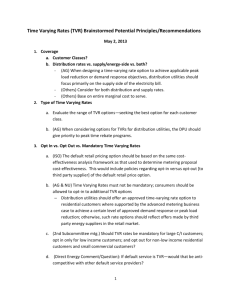
Online Figure 4. LPN Sensitivity Analysis at a) 1 MET and b) 5 MET
Simulated patient weight=70kg, height=160cm