Freytag, Jennifer L. Investigating the role of matrix
advertisement

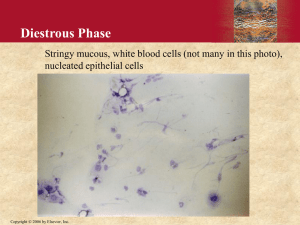
Freytag, Jennifer L. Investigating the role of matrix metalloproteinases in growth factor-induced migration and invasion of epithelial cells Principle Investigator: Jennifer L. Freytag, Ph.D. Sage College of Albany Department of Biology Office SCA: x1754 Office RSC: x2280 Cell: (518) 859-4837 Email: freytj@sage.edu 1 Freytag, Jennifer L. ABSTRACT Skin cancer is the most prevalent form of cancer in the United States, and one in every five Americans will develop skin cancer in the course of their lifetime. One type of nonmelanoma skin cancer, squamous cell carcinoma (SCC), is a highly lethal in its aggressive form, particularly because it can gain the ability to invade surrounding tissues, eventually metastasizing to a distant organ. If the cancer remains at its original site, it is considered benign and is easily removed. It is the gain of the ability to move from the original cancer site to a distant one that proves problematic for currently available treatments. Emergence of an aggressive form of many different types of cancers is frequently accompanied by increases in specific growth factors. These growth factors bind to receptors on the cell surface and activate specific signaling pathways inside the cell of the tumor. Activation of these pathways ultimately culminates in changes in gene expression of the cancer cells, allowing them to achieve their altered, cancerous state. In order to study the progression to an invasive carcinoma, a model system using transformed epithelial cells grown in a controlled cell culture environment has been developed. Previous research has determined that cells must become highly motile and highly invasive in order to develop a metastatic cancer. This study will use a method for quantification of cell migration and invasion. SPECIFIC AIMS OF THE STUDY Two growth factors that have been identified to be increased in aggressive SCC are transforming growth factor- (TGF-) and epidermal growth factor (EGF). Previous research performed by this investigator and others indicates that TGF- and EGF will elicit an altered phenotype in cell culture when added to a human keratinocyte cell line for two days. This altered phenotype and 2 Freytag, Jennifer L. behavior is documented in Figure 1. Most notably, the cells change drastically in shape (which mirrors what has been observed in aggressive cancers in the body) and the cells become highly motile, which is necessary for a cancer cell to move from its original site to a distant organ. While this motile phenotype is apparent, a need to quantify how much a cell moves is imperative. Research previously done by this investigator implicated several key proteins that whose activity is required to get this observed change in growth factor-treated cells. It is therefore important to quantify the effects these proteins have on development of this highly aggressive, motile phenotype, which will be addressed in the following specific aims. Specific Aim 1: Using a physiologically relevant model system for studying the motile response of epithelial cells, identify the requirement of matrix metalloproteinases in epithelial cell migration. Various small molecule inhibitors have been known to block the function of specific proteins. Of importance to our study is a large family of proteins termed matrix metalloproteinases (MMPs). We have preliminary data indicating that the level of several of these proteins is increased by addition of growth factors, leading to cancer progression, so here we aim to identify which MMPs are critical for epithelial cell migration. Specific Aim 2: Using a physiologically relevant model system for studying the invasive response of epithelial cells, identify the requirement of matrix metalloproteinases in epithelial cell invasion. Not only must cells move during the metastatic process, but cells must also gain the ability to degrade through thick protein layers in order to metastasize from the site of the original tumor. Several players thought to be responsible for this process are found in the MMP family. Using a 3 Freytag, Jennifer L. model system to measure the capability for a cell to degrade proteins, we aim to determine which MMPs are required for this process. Control + Growth Factors Figure 1: TGF-β1+EGF stimulation induces cell scattering and altered phenotype in HaCaT cells BACKGROUND INFORMATION Nonmelanoma skin cancers (NMSCs) are the most common human malignancies (Eide and Weinstock, 2005; Lang and Maize, 2005). In North America alone, greater than 50% of all neoplasms arise in the skin (Dlugosz et al., 2002) and the incidence of NMSC in Australia for the year 2002 was more than five times the incidence of all other cancers combined (Staples et al., 2006). One type of NMSC is squamous cell carcinoma (SCC). Relative to other types of skin tumors, advanced SCC is aggressive, resistant to localized therapy with significant associated mortality and increasing frequency (Nguyen and Yoon, 2005). The emergence of epithelial skin tumors appears causally linked to ultraviolet (UV) radiation exposure. Specific UV-B “signature” gene changes likely occur early in epidermal carcinogenesis. Transition of a normal keratinocytes to an initiated pre- or early malignant phenotype, in fact, often involves loss- or gain-of-function mutations in a multitude of genes (Boukamp, 2005; Tsantoulis et al., 2007; Yuspa, 1998). These accumulated genetic changes accompanying evolution of aggressive subtypes of cutaneous SCC are found in the context of a complex environment contributed to by both tumor and surrounding cells. These changes are largely contributed by increases in different growth 4 Freytag, Jennifer L. factors (e.g., hepatocyte growth factor (HGF); epidermal growth factor (EGF); platelet-derived growth factor (PDGF); and transforming growth factor- (TGF-)) (Cui et al., 1996; Derynck et al., 2001; Han et al., 2005; Kalluri and Weinberg, 2009; Moreno-Bueno et al., 2008; Portella et al., 1998). TGF- is a particularly robust initiator of phenotypic changes that frequently accompany cancer progression and is a likely facilitator of tumor invasion and metastasis (Kalluri and Weinberg, 2009; Moreno-Bueno, et al., 2008). Indeed, acquisition of cancer celllike traits with creation of a morphologically restructured, motile phenotype (e.g., Heldin et al., 2009; Thiery and Sleeman, 2006) is thought to facilitate development of invasive carcinomas (Cui et al., 1996; Peinado et al., 2007; Portella et al., 1998; Zavadil et al., 2001; Zavadil and Bottinger, 2005). One proposed mechanism of increased capability to metastasize is through increased expression of certain matrix metalloproteinases (MMPs). The MMPs are proteins responsible for cleaving a wide range of proteins, such as the degradation of extracellular matrix proteins, release of membrane-bound growth factors, and activation of other metalloproteinases (reviewed in Curran and Murray, 1999). With increased expression of MMPs, cells have the ability to “chew through” thick protein matrices designed to help keep certain cells in particular locations throughout the body. When cancer cells begin to take on an aggressive form, they degrade these protein matrices and invade to distant sites, allowing for tumor metastasis. 5 Freytag, Jennifer L. METHODOLOGY, EXPECTED RESULTS, AND FUTURE DIRECTIONS Specific Aim 1: Using a physiologically relevant model system for studying the motile response of epithelial cells, identify the requirement of matrix metalloproteinases in epithelial cell migration. A two-dimensional wound-healing model can be used as a way to quantify cell migration. When a wound is created in a layer of epithelial cells, those cells at the edge of the wound become initiated to move and/or multiply to fill the vacant area created by the wound. Using this scenario in cell culture by creating a “wound” in a layer of epithelial cells, the amount of migration can be quantified. Various specific small molecule inhibitors of MMPs have been developed and can be purchased. These can then be used to determine which of the MMP family members are responsible for increased cell motility in the two-dimensional wound-healing model. If these inhibitors work to block cell migration in the cell culture model, further experiments can determine if these inhibitors can block cancer cell invasion in an animal model. Specific Aim 2: Using a physiologically relevant model system for studying the invasive response of epithelial cells, identify the requirement of matrix metalloproteinases in epithelial cell invasion. For determination of epithelial invasion, two different techniques can be used. Platypus Technology’s Oris Cell Invasion Assay kits are an accurate and effective way to measure the amount of cells that can invade though a thick protein matrix. It is expected that if MMPs are essential for optimal cell invasion, upon growth factor treatment, the various MMP inhibitors will block the amount of cell invasion as quantitated by the Oris Cell Invasion Assay. An alternative method will also be employed using the established Boyden chamber method for quantification of exact numbers of invasive cells. Cells are seeded on the top of the chamber 6 Freytag, Jennifer L. must invade through a think protein matrix in order to reach the other side of the chamber. The number of cells with invasive capacity can then be counted. Using the MMP inhibitors in this assay will allow for a method to measure amount of impact that these inhibitors have on the amount of cell invasion. BUDGET Total amount requested: $5000 1. MMP inhibitors and antibodies: $1000 2. Tissue culture supplies: $1200 3. Oris cell invasion assay (4): $1400 4. Boyden chamber inserts and protein matrix: $1100 5. Camera for inverted microscope: $300 1. MMP inhibitors and antibodies: There are several available small molecule inhibitors available to block the different MMP family members’ activity in cells. One or more of these inhibitors can be used to indicate that particular MMPs are playing a role in cancer cell migration and invasion. Importantly, many of the MMPs have specific inhibitors that will specifically block the activity of a specific MMP, which will allow us to implicate the role of that MMP in cell migration and/or invasion. 2. Tissue culture supplies: To do all proposed experiments, tissue culture supplies are needed. (This includes: tissue culture dishes, tissue culture plates, sterile pipets, growth media for cells, antibiotics for growth media, trypsin and cell scrapers to harvest cells, carbon dioxide gas needed 7 Freytag, Jennifer L. to grow the cells. Sage College of Albany has the incubator necessary to grow the cells and the tissue culture hood required to work with mammalian cells in culture. 3. Cell invasion assay: Platypus Technologies produces a novel assay to measure amount of cell migration and/or invasion. Quantitative tracking of cells that migrate in response to growth factors and/or MMP inhibitors can help predict how cells would behave in the body if they were trying to invade surrounding tissues, which is the first step in cancer metastasis. These assays have been used by the researcher before, so have been validated as a reliable quantitative method to monitor cell invasion. 4. Boyden chamber inserts and protein matrix: The Boyden chamber provides for a method of quantifying the number of cells that are able to invade though a protein matrix. This required the purchase of the chambers, the membrane inserts and the protein matrix. These components can then be assembled. Cells are seeded on top of the chamber and allowed time to invade through the protein matrix. The cells that have successfully invaded can be identified by their location on the bottom of the chamber. The number of cells can be counte3d using a software program. 5. Camera for inverted microscope: In order to properly view mammalian cells growing in culture, an inverted microscope is necessary (microscope objectives located below the stage are required to view the cells sitting on the bottom of a tissue culture dish). Recently this sophisticated microscope was purchased. The addition of a camera to this microscope would allow images to be taken as cells at different time periods as cells were migrating. It would also allow for quantitation by publicly available cell counting software. Furthermore, a camera for the inverted microscope would improve the current Cell and Molecular Biology lab course 8 Freytag, Jennifer L. (BIO319) offered at SCA, as several parts of the labs require culture and observation of mammalian cells. SIGNIFICANCE OF THE STUDY Identification of members of the matrix metalloproteinase family of proteins may lead to the development of novel therapeutics that target specific stages of human tumor progression. This study models squamous cell carcinomas, but these findings could potentially be relatable to other types of cancers as well. QUALIFICATIONS OF RESEARCHER Jennifer L. Freytag, Ph.D. has been working in the area of cancer research in various capacities since 2004. She has previously worked as an intern, a graduate student, and a postdoctoral fellow at Albany Medical College (AMC) in The Center for Cell Biology and Cancer Research. Dr. Freytag still retains research ties with Albany Medical College and does voluntary research as a visiting scientist. Dr. Freytag is currently collaborating with Paul J. Higgins, Ph.D. at AMC. Dr. Higgins has had an established lab in the field cell biology at AMC for over 20 years. He has a well-established lab, with multiple pieces of invaluable and technologically advanced equipment that will greatly facilitate this research project. Dr. Higgins has agreed to continue collaboration with Dr. Freytag on this proposed study. 9 Freytag, Jennifer L. REFERENCES Boukamp, P. (2005). UV-induced skin cancer: similarities-variations. J. Dtsch. Dermatol. Ges. 3, 493-503. Cui, W., Fowlis, D. J., Bryson, S., Duffie, E., Ireland, H., Balmain, A. and Akhurst, R. J. (1996). TGF1 inhibits the formation of benign skin tumors, but enhances progression to invasive spindle carcinomas in transgenic mice. Cell 86, 531-542. Curran, S. and Murray, G.I. (1999). Matrix metalloproteinases in tumor invasion and metastasis. J. Pathol. 189, 300-308. Derynck, R., Akhurst, R. J. and Balmain, A. (2001). TGF- signaling in tumor suppression and cancer progression. Nat. Genet. 29, 117-129. Dlugosz A., Merlino G. and Yuspa S. H. (2002). Progress in cutaneous cancer research. J. of Invest Derm. Symp. Proc. 7, 17-26. Eide M. J. and Weinstock M. A. (2005). Epidemiology of skin cancer. Cancer of the Skin 4760. Han, G., Lu, S. L., Li, A. G., He, W., Corless, C. L., Kulesz-Martin, M. and Wang, X. J. (2005). Distinct mechanisms of TGF-1-mediated epithelial-to-mesenchymal transition and metastasis during skin carcinogenesis. J. Clin. Invest. 115, 1714-1723. Heldin, C. H., Landström, M. and Moustakas, A. (2009). Mechanism of TGF-β signaling to growth arrest, apoptosis, and epithelial-mesenchymal transition. Curr. Opin. Cell Biol. 21, 166-176. Kalluri, R. and Weinberg, R. A. (2009). The basis of epithelial-mesenchymal transition. J. Clin. Invest. 119, 1420-1428. Lang, P. G. and Maize, J. C. (2005). Basal Cell Carcinoma. Cancer of the Skin. 101-132. Moreno-Bueno, G., Portillo, F. and Cano, A. (2008). Transcriptional regulation of cell polarity in EMT and cancer. Oncogene 27, 6958-6969. Nguyen, T. H. and Yoon, J. (2005). Squamous cell carcinoma. Cancer of the Skin. 133-150. Peinado, H., Olmeda, D. and Cano, A. (2007). Snail, ZEB, and bHLH factors in tumour progression: an alliance against the epithelial phenotype? Nat. Rev. Cancer 7, 415-428. Portella, G., Cumming, S. A., Liddell, J., Cui, W., Ireland, H., Akhurst, R. J. and Balmain, A. (1998). Transforming growth factor is essential for spindle cell conversion of mouse skin carcinoma in vivo: implications for tumor invasion. Cell Growth Differ. 9, 393-404. Staples, M. P., Elwood, M., Burton, R. C., Williams, J. L., Marks, R. and Giles G. G. (2006). Non-melanoma skin cancer in Australia: the 2002 national survey and trends since 1985. Med. J. Austrialia. 184, 6-10. Thiery, J. P. and Sleeman, J. P. (2006). Complex networks orchestrate epithelial-mesenchymal transitions. Nat. Rev. Mol. Cell Biol. 7, 131-142. Tsantoulis, P. K., Kastrinakis, N. G. Tourvas, A. D., Laskaris, G. and Gorgoulis V. G. (2007). Advances in the biology of oral cancer. Oral Oncol. 43, 523-534. Yuspa, S. H. (1998). The pathogenesis of squamous cell cancer: lessons learned from studies of skin carcinogenesis. J. Dermatol. Sci. 17, 1-7. Zavadil, J., Bitzer, M., Liang, D., Yang, Y. C., Massimi, A., Kneitz, S., Piek, E. and Böttinger, E. P. (2001). Genetic programs of epithelial cell plasticity directed by transforming growth factor-β. Proc. Natl. Acad. Sci. USA. 98, 6686-6691. 10 Freytag, Jennifer L. Zavadil, J. and Böttinger, E. P. (2005). TGF- and epithelial-to-mesenchymal transitions. Oncogene 24, 5764-5774. 11