Surgical Case
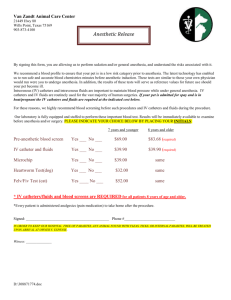
advertisement

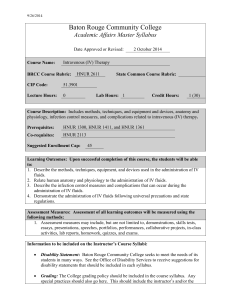
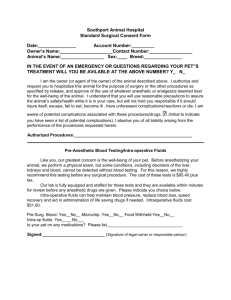
Simulation Interest Group Scenario Template I. Title: Gynecology Simulation Case 1 - 22 year old female Topic: Female with Vaginal Bleeding and Pelvic Pain Last Modified: 10/31/2010 II. Target Audience: All levels of gynecology students and providers III. Learning Objectives or Assessment Objectives A. Learning Objectives 1. Demonstrate the appropriate and early diagnosis of an ectopic pregnancy. 2. Demonstrate the ability to decide which treatment options are most appropriate for each clinical scenario. B. Critical actions checklist – a list to ensure the educational /assessment goals are met. This may include: 1. Simple checklist of critical actions – built into the case narrative below 2. Optimal sequence of critical actions – Make the diagnosis, order appropriate laboratory and radiographic studies, decide to proceed with management 3. Duration to critical actions– built into the case narrative below 4. Scoring based on performance actions – built into the case narrative below IV. A. B. Case Narrative Scenario Background Given to Participants Chief complaint, triage note, medic report - 22 year old healthy, but anxious, female with vaginal bleeding. The patient complains of lower abdominal pain for the last 3 days, worse in the last 6 hours. 1. Past medical history Illnesses: mild asthma Surgeries: none 2. Meds and allergies Meds: albuterol inhaler as needed Allergies: NKDA Habits: denies smoking and illicit drug use, drinks alcohol 4 times per week, 3-4 drinks at a time 3. OB/Gyn Hx: never been pregnant, has regular periods but isn’t sure when her last period was. Has no history of sexually transmitted diseases. Never had a Pap smear. 4. Physical Exam Thin, fit appearing female, anxious and in mild distress Wt : 53 kg T : 37.2 HR : 105 BP : 90/60 RR : 20 Lungs: clear Heart: normal Abdomen: slightly distended, tender to palpation in bilateral lower quadrants with mild rebound tenderness. No masses, HSM, or hernia. PV: not done 5. Pelvic Ultrasound Uterus: 7.3 cm x 3.5 cm x 4.4 cm Endometrium 2.9 mm with no intrauterine pregnancy Left ovary: 2.2 x 3.8 x 3.4 cm with left adnexal mass of 4.7 x 6.0 x 2.9 cm Right ovary: 3.3 x 1.5 x 3.8 cm Free fluid in cul-de-sac: moderate 6. Labs Urine Pregnancy Test: positive Hematocrit: 29 White blood cell count 12.2 Electrolytes, Glucose, Blood Urea Nitrogen, creatinine : normal 7. NPO Status Last ate 4 hours ago C. State: Arrive 1. History patient gives: The patient is uncomfortable but complies with all requests. 2. Exam: Abdomen is slightly distended, tender to palpation in bilateral lower quadrants with mild rebound tenderness without masses, hepatospenomegaly, or hernia. 3. Phys: HR 105, 90/ 60 4. What Next: Perform quick history and physical exam, including a visual speculum exam of the vagina. Do NOT perform brisk bimanual exam at this time. Establish IV access and administer fluids. Order pregnancy test and pelvic ultrasound. 5. Transitions: a. To state: Diagnosis If: ultrasound & pregnancy test Points: +200 Debrief: You appropriately performed a pregnancy test and pelvic ultrasound exam b. To state: Fluids i. If: Intravenous Fluid > 999cc and < 2001cc ii. Points: +200 iii. Debrief: You appropriately administered IV fluids. c. To state: Fluids i. If: Intravenous Fluid > 2000cc ii. Points: -100 iii. Debrief: You administered a very large initial intravenous fluid bolus d. To state: Medical Management i. If: methotrexate administered D. E. ii. Points: -600 iii. Debrief: You should not have administered methotrexate for this case. e. To state: Surgical Management i. If: salpingectomy/salpingostomy ordered ii. Points: -400 iii. Debrief: You appropriately performed surgery to remove the ectopic pregnancy, but you did not appropriately order tests first. f. To state: Delay i. If: >300 sec elapses ii. Points: -400 iii. Debrief: You failed to act in a timely fashion during this urgent clinical scenario State: Diagnosis 1. History patient gives: The patient's pain is worse and she is beginning to feel light-headed when she sits up 2. Exam: The abdomen is more distended and there is clear rebound tenderness 3. Phys: BP 88/58 HR 115 4. What Next: Establish IV access and administer fluids 5. Transitions: a. To state: Diagnosis with Fluids i. If: Intravenous Fluid > 999cc and Intravenous Fluid < 2001cc ii. Points: +200 iii. Debrief: You appropriately administered intravenous fluids b. To state: Diagnosis with Fluids i. If: Intravenous Fluids > 2000 cc were administered ii. Points: -100 iii. Debrief: You administered a very large initial IV fluid bolus c. To state: Surgical Management i. If: salpingectomy/salpingostomy ordered ii. Points: +200 iii. Debrief: You appropriately performed surgery to remove the ectopic pregnancy, but you should have replaced intravenous fluids d. To state: Medical Management i. If: methotrexate administered ii. Points: -600 iii. Debrief: You should not have administered methotrexate for this case e. To state: Delay Diagnosis i. If: > 300 sec elapses ii. Points: -400 iii. Debrief: You should have performed a pregnancy test and pelvic ultrasound exam sooner State: Fluids 1. History patient gives: The patient's pain is worse 2. Exam: The abdomen is more distended and there is clear rebound tenderness F. 3. Phys: BP 100/70 HR 95 4. What Next: Perform pregnancy test and pelvic ultrasound 5. Transitions: a. To state: Diagnosis with Fluids i. If: Intravenous Fluid > 999cc and Intravenous Fluid < 2001cc ii. Points: +200 iii. Debrief: You appropriately administered intravenous fluids b. To state: Diagnosis with Fluids i. If: Fluids > 2000 cc were administered ii. Points: -100 iii. Debrief: You administered a very large initial intravenous fluid bolus c. To state: Fluids with Surgical Management i. If: salpingectomy/salpingostomy ordered ii. Points: -400 iii. Debrief: You appropriately performed surgery to remove the ectopic pregnancy, but you did not appropriately evaluate the patient first d. To state: Fluids with Medical Management i. If: Methotrexate administered ii. Points: -600 iii. Debrief: You should not have administered methotrexate for this case e. To state: Delay Fluids i. If: >300 sec elapses ii. Points: -400 iii. Debrief: You should have performed a pregnancy test and pelvic ultrasound exam sooner. State: Delay 1. History patient gives: The patient's pain is worse and she is beginning to feel light-headed when she sits up 2. Exam: The abdomen is more distended and there is clear rebound tenderness 3. Phys: BP 84/54 HR 120 4. What Next: Establish IV access and administer fluids. Perform pregnancy test and pelvic ultrasound 5. Transitions a. To state: Delay & Diagnosis i. If: ultrasound & pregnancy test ii. Points: +200 iii. Debrief: You appropriately performed a pregnancy test and pelvic ultrasound exam b. To state: Delay & Fluids i. If: Intravenous Fluid > 999cc and Intravenous Fluid < 2001cc ii. Points: +200 iii. Debrief: You appropriately administered intravenous fluids c. To state: Delay & Fluids G. H. i. If: Intravenous Fluid > 2000cc ii. Points: -100 iii. Debrief: You administered a very large initial intravenous fluid bolus d. To state: Medical Management i. If: methotrexate administered ii. Points: -800 iii. Debrief: You should not have administered methotrexate for this case e. To state: Surgical Management i. If: salpingectomy/salpingostomy ordered ii. Points: -600 iii. Debrief: You appropriately performed surgery to remove the ectopic pregnancy, but you did not appropriately order tests first f. To state: Critical Delay i. If: >300 seconds elapse ii. Points: -400 iii. Debrief: You failed to act in a timely fashion during this urgent clinical scenario State: Diagnosis with Fluids 1. History patient gives: The patient's pain is worse 2. Exam: The abdomen is more distended and there is clear rebound tenderness 3. Phys: BP 100/70 HR 95 4. What Next: Take the patient to surgery for the ectopic pregnancy 5. Transitions; a. To state: Fluids with Surgical Management i. If: salpingectomy/salpingostomy ordered ii. Points: +600 iii. Debrief: You appropriately performed surgery to remove the ectopic pregnancy b. To state: Fluids with Medical Management i. If: Methotrexate administered ii. Points: -600 iii. Debrief: You should not have administered methotrexate for this case c. To state: Delay Diagnosis i. If: > 300 sec elapses ii. Points: -200 iii. Debrief: You should have administered fluids sooner State: Delay Diagnosis 1. History patient gives: The patient's pain is worse and she is very light-headed 2. Exam: The abdomen is more distended and there is clear rebound tenderness 3. Phys: BP 120 84/84 4. What Next: Establish IV access and administer fluids 5. Transitions: a. To state: Diagnosis with Fluids I. i. If: Intravenous Fluid > 999cc and Intravenous Fluid < 2001cc ii. Points: +200 iii. Debrief: You appropriately administered IV fluids b. To state: Diagnosis with Fluids i. If: Intravenous Fluids > 2000 cc were administered ii. Points: -100 iii. Debrief: You administered a very large initial intravenous fluid bolus. c. To state: Surgical Management i. If: salpingectomy/salpingostomy ordered ii. Points: +200 iii. Debrief: You appropriately performed surgery to remove the ectopic pregnancy, but you should have replaced intravenous fluids. d. To state: Medical Management i. If: methotrexate administered ii. Points: -600 iii. Debrief: You should not have administered methotrexate for this case e. To state: Critical Delay & Diagnosis i. If: >300 sec elapse ii. Points: -200 iii. Debrief: You should have acted on your diagnostic tests, pregnancy test and pelvic ultrasound exam, sooner. State: DELAY with FLUIDS 1. History patient gives: The patient's pain is worse. 2. Exam: 3. Phys: BP 89/60 HR 115 4. What Next: Perform pregnancy test and pelvic ultrasound. 5. Transitions: The abdomen is more distended and there is clear rebound tenderness. a. To state: Diagnosis with Fluids i. If: perform pelvic ultrasound and pregnancy test ii. Points: +400 iii. Debrief: You appropriately performed pregnancy test and pelvic ultrasound exam b. To state: Fluids with Surgical Management i. If: salpingectomy/salpingostomy ordered ii. Points: +200 iii. Debrief: You appropriately performed surgery to remove the ectopic pregnancy, but you really should order pregnancy test and perform pelvic ultrasound to make the diagnosis first c. To state: Fluids with Medical Management i. If: Methotrexate administered ii. Points: -600 iii. Debrief: You should not have administered methotrexate for this case J. K. L. M. d. To state: Dead i. If: >300 seconds elapse ii. Points: -1000 iii. Debrief: You should have performed a pregnancy test and pelvic ultrasound exam and surgery sooner EndState: Fluids with Surgical Management 1. History patient gives: Patient is recovering from anesthesia 2. Exam: Patient is recovering from anesthesia 3. Phys: BP 110/80 HR 92 4. What Next: End of case simulation. You met the learning objectives for this case EndState: Surgical Management 1. History patient gives: Patient is recovering from anesthesia 2. Exam: Patient is recovering from anesthesia 3. Phys: BP 90/60 HR 110 4. What Next: End of case simulation. You met the learning objectives for this case but should have administered intravenous fluids EndState: Fluids with Surgical Management 1. History patient gives: Patient is recovering from anesthesia 2. Exam: Patient is recovering from anesthesia 3. Phys: BP 110/80 HR 92 4. What Next: End of case simulation. You met the learning objectives for this case State: Critical Delay 1. History patient gives: The patient's pain is worse and she very light-headed 2. Exam: The abdomen is more distended and there is clear rebound tenderness 3. Phys: BP 60/20 HR 140 4. What Next: Establish IV access and administer fluids. Perform pregnancy test and pelvic ultrasound 5. Transitions: a. To state: Critical Delay then Diagnosis i. If: perform pelvic ultrasound and pregnancy test ii. Points: +200 iii. Debrief: You appropriately performed pregnancy test and pelvic ultrasound exam b. To state: Delay with Fluids i. If: Intravenous Fluids >999cc and <2001cc ii. Points: +200 iii. Debrief: You appropriately administered intravenous fluids c. To state: Delay with Fluids i. If: Fluids >2000cc ii. Points: -100 iii. Debrief: You administered a very large initial intravenous fluid bolus d. To state: Surgical Management i. If: salpingectomy/salpingostomy ordered ii. Points: +200 N. O. iii. Debrief: You appropriately performed surgery to remove the ectopic pregnancy, but you should have replaced intravenous fluids. e. To state: Medical Management i. If: methotrexate administered ii. Points: -600 iii. Debrief: You should not have administered methotrexate for this case f. To state: Dead i. If: >300 seconds elapse ii. Points: -1000 iii. Debrief: You failed to act in a timely fashion during this urgent clinical scenario State: Critical Delay & Diagnosis 1. History patient gives: The patient's pain is worse and she very light-headed 2. Exam: The abdomen is more distended and there is clear rebound tenderness 3. Phys: BP 60/20 HR 140 4. What Next: Establish IV access and administer fluids 5. Transitions: a. To state: Diagnosis with Fluids i. If: tFluid > 999 and tFluid < 2001 ii. Points: +200 iii. Debrief: You appropriately admnistered IV fluids b. To state: Diagnosis with Fluids i. If: Fluids > 2000 cc were administered ii. Points: -100 iii. Debrief: You admnistered a very large initial IV fluid bolus c. To state: Surgical Management i. If: salpingectomy/salpingostomy ordered ii. Points: +200 iii. Debrief: You appropriately performed surgery to remove the ectopic pregnancy, but you should have replaced intravenous fluids d. To state: Medical Management i. If: methotrexate administered ii. Points: -600 iii. Debrief: You should not have administered methotrexate for this case e. To state: Dead i. If: >300 seconds elapse ii. Points: -1000 iii. Debrief: You failed to act in a timely fashion during this urgent clinical scenario. END State: Dead 1. History patient gives: The patient is unresponsive 2. Exam: The abdomen is soft. The skin is cyanotic. Heart sounds are absent 3. Phys: BP 0 HR 0 V. 4. What Next: Notify the family. You should review the learning objectives and try this case again Instructor’s Notes A. This scenario was created to run on Anesoft Obstetrics Simulator 3® B. Each trainee will require 15-30 minutes to complete the case and read the didactic part of the case. Included are case instructions for the trainee. C. Time with a preceptor should occur in close proximity to the case completion to review the decision-making and objectives of the case. D. VI. VII. Limitations: As for any simulated case, it is difficult to anticipate all trainee selections. Individual management decisions during an actual ectopic pregnancy will vary according to the clinical scenario. Debriefing Plan A. Method of debriefing – debriefing comments provided above for each transition made during the case simulation as described in the case narrative. B. Comments for the debriefing – provided as above Pilot Testing and Revisions A. Numbers of participants – this scenario is modeled from the simulations used by the anesthesia residents over the last 2 decades at the University of Washington. This clinical tool uses a modification, making it applicable to OB/Gyn trainees. It has now been incorporated in the training for the first year OB/Gyn residents. Their surveys reveal that this is a worthwhile activity that allows them to be better prepared for similar clinical scenarios. B. Performance expectations, anticipated management mistakes: 1. Many junior residents take 5 or more minutes to diagnose ectopic pregnancy. 2. Many residents fail to act to definitely diagnose ectopic pregnancy and fluid resuscitate while they are making management decisions. C. Evaluation form for participants: Participants receive a detailed printed record of the case simulation and printed debriefing of their case management. VIII. Authors and their affiliations Brenda S. Houmard, MD, PhD and Howard A. Schwid, MD Departments of Obstetrics & Gynecology & Anesthesiology University of Washington Sagittal view of the Uterus – No Sagittal view of Posterior Cul-de-Sac Intrauterine Pregnancy showing free intra-abdominal fluid Sagittal View of Right Ovary (normal) Sagittal View of Left Ovary and Echogenic left ovarian mass Uterus: of IUP. Normal. No evidence Adjacent mass Endometrium: Normal. Thickness: 2.9 mm. Fibroid(s): None seen. Right Ovary: Normal. Left Adnexa: Mass adjacent to left ovary. No discrete gestational sac seen. Small cystic area within mass has some blood flow. Mass is heterogeneous and measures 4.7 x 6.0 x 2.9cm. Cul-de-Sac: Echogenic free fluid. Moderate amount L: 7.3 W: 3.5 D: 4.4 Volume: 58.8 cc Uterus (cm): Right Ovary (cm): L: 3.3 W: 1.5 D: 3.8 Volume: 9.8 cc Left Ovary (cm): L: 2.2 W: 3.8 D: 3.4 Volume: 14.9 cc Size (cm): Mass: Lt adnexal L: 4.7 W: 6.0 D: 2.9 Volume: 42.8 cc SUMMARY Impression: No intrauterine pregnancy is identified. A heterogeneous echogenic mass is seen adjacent to the left ovary that measures 6.0 cm in maximal dimension. There is no clear gestational sac identified in this mass. Echogenic free fluid is also seen in the pelvis.