Patient Care
advertisement

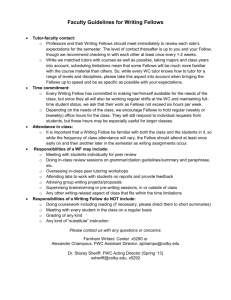
VCUHS HEMATOLOGY/ONCOLOGY FELLOWSHIP CURRICULUM Palliative Care Rotation Description of Rotation or Educational Experience The Hematology-Oncology fellowship palliative care rotation is designed to provide the fellow with the opportunity to participate in the care and management of patients admitted to the hospital in the acute setting requiring palliative acute symptom relief and/or end-of-life management and well as outpatients with cancer with chronic pain or palliative needs. The fellow operates in the context of the interdisciplinary team of physicians, mid-level providers, nurses, chaplains, social workers, and therapists trained in hospice and palliative care medicine. The fellow is exposed to the use of care sets developed for palliative care and hospice management. This rotation provides a unique opportunity for exposure to routine and advanced pain management techniques and organ-based and systemic symptom management techniques when diseasespecific therapy alone has been insufficient. The rotation also allows fellows to directly experience patient care in the inpatient and home hospice settings. Additionally, the rotation focuses on training the fellow in the establishment and communication of goals-of-care with the patient, the family, and an interdisciplinary team. All of this occurs under the supervision of the specially trained attending physicians and mid-level providers in hospice and palliative care within the Division of Hematology, Oncology, and Palliative Care. To optimize this experience for Hematology-Oncology fellows, the rotation is divided into three parts. The first part focuses on pain and symptom management. During this one-week period, fellows work with a member of the palliative care team evaluating case studies and seeing consults focused on pain and symptom management. Fellows also participate in palliative supportive care clinics during this week. The second part of the rotation focuses on inpatient care on the palliative care unit and consults pertaining to oncology patients. During this two-week period, fellows are the primary provider for at least one to two patients on the inpatient palliative care unit. Fellows are also the primary consultant for a variety of palliative care consults with a focus on those pertaining to oncology patients. Fellows also accompany the palliative care chaplain on at least two chaplain consults, which enables fellows to observe spiritual assessment and communication. The third part of the rotation focuses on hospice care. During this one-week period, fellows attend an inpatient hospice unit visit and a home hospice visit that they schedule through a local hospice agency. Throughout the 4 week rotation, fellows also participate in the weekly palliative care Problem Based Learning Initiative (PBLI) conferences, and they complete required reading assignments on palliative care and hospice. Fellows are also available to see general palliative care consults when not in clinic or on a specific assignment. Location: VCUHS MCV Hospital Palliative Care Unit VCUHS Dalton Oncology Palliative Care Clinic VCUHS MCV Hospital inpatient nursing units Hospice of Virginia inpatient unit and home hospice settings Length of Experience: 4 week block – days only including weekend day coverage with one day in 7 off of all clinical duties. There is no in-house overnight call on this rotation. Educational Goals Gain experience and knowledge in the evaluation, grading and management of acute and chronic pain from malignant and non-malignant etiologies Gain experience and knowledge in the diagnosis and management of organ-based and systemic manifestations of locally advanced or metastatic malignancy Gain experience in working with an interdisciplinary palliative care team. Gain experience and knowledge in effective establishment and communication of goals of care Gain experience in the management of the patient at the end-of-life and the resources available to the patient and their families Gain experience and knowledge of hospice care in both the inpatient and outpatient settings. Gain experience in addressing psychological and spiritual concerns in patients enduring severe illness and at the end of life. Gain experience and knowledge of the legal and societal issues as they pertain to the end-of-life management. Gain experience in and respect for the cultural differences in response to severe illness and death Gain experience in recognizing one’s own reaction to grief and stress as a provider Patient Care Goal Fellows must be able to provide patient care that is compassionate, appropriate, and effective for the treatment of health problems and the promotion of health. Please refer to overview of the fellowship curriculum for competencies/objectives for patient care. Specifically, fellows will see patients in both the acute inpatient hospital and the outpatient clinic settings under the supervision of the appropriate subspecialty faculty members. In addition, fellows will see patients in the inpatient hospice and home hospice settings under the supervision of certified hospice nurses. Fellows will participate in the evaluation, counseling, and management of acutely and chronically ill patients with both malignant and non-malignant medical conditions in need of palliative and/or end-of-life care. This will provide the opportunity to learn the different approaches to the management of these conditions. Fellows will additionally work within an interdisciplinary team of health professionals including midlevel providers, pharmacists, nurses, physical therapies, occupational therapists, social workers, care coordinators, and pastoral care. This will provide the fellow experience and feedback in effectively working within an interdisciplinary team of health professionals. Competencies Fellows are expected to: Gather appropriate clinical information Synthesize information into a care plan Partner with patients/families in the implementation of the plan and goals of care Coordinate care plans with the interdisciplinary team of health professionals and the home health agencies Objectives Fellows are expected to: Develop skills in history/physical examination of the patient Integrate clinical data in the formation of a comprehensive care plan Document the encounter in the medical record in sufficient detail to communicate to other physicians and meet billing requirements Provide compassionate, appropriate, and comprehensive patient care Medical Knowledge Goal Fellows must demonstrate knowledge of established and evolving biomedical, clinical, epidemiological, and social-behavioral sciences, as well as the application of this knowledge to patient care. Competencies Fellows are expected to demonstrate skills in: Acquisition of knowledge Analysis of information Application of knowledge Objectives All fellows are expected to: Demonstrate the ability to perform a comprehensive and accurate physical examination; demonstrate the ability to arrive at an appropriate differential diagnosis; outline a logical plan for specific and targeted investigations pertaining to the patient’s complaints; and formulate a plan for management and follow-up treatment of the patient Demonstrate their knowledge by presenting the results of a consultation orally and in writing and by defending the clinical assessment, differential diagnosis, and diagnostic and management plans Rotation-Specific Objectives Assess and quantify a patient’s pain using a variety of pain assessment tools Discuss the indications and use of a variety of medications and delivery methods used in delivery of analgesia in both the acute and chronic pain setting. Discuss the indications and use of a variety of non-pharmacologic methods used in the management of both acute and chronic pain. Calculate initial PCA dosing parameters, interrogate a PCA pump and make dose adjustments based on serial assessments of the patient’s pain. Convert among a variety of analgesics including the ability to account for a variety of routes of delivery including but not limited to oral, intravenous, subcutaneous, and epidural routes Discuss the pharmacologic properties of the various analgesics Discuss the palliative management of malignancy-related dyspnea, nausea/emesis, and anorexia/cachexia. Assess a patient’s functional performance using a variety of assessment tools Recognize the stages of normal grieving and coping. Recognize, diagnose, and manage psychological and spiritual conditions and the role that they might play in the management of the patient’s other medical conditions. Recognize the need for referral and demonstrate a knowledge of the resources available in the management of psychological and spiritual conditions Demonstrate a knowledge of and application of palliative care algorithms for the management of end-of-life conditions including but not limited to anxiety, agitation, psychological and spiritual angst, dyspnea, and pain. Practice- Based Learning and Improvement Goal Fellows must demonstrate the ability to investigate and evaluate their care of patients, to appraise and assimilate scientific evidence, and to continuously improve patient care based on constant self-evaluation and lifelong learning. The fellow is expected to present primary scientific and medical evidence to support their conclusions and care plans in the diagnosis, prognosis, management, and monitoring of the patients on the service. The fellow is expected to recognize their areas of deficiency. Depending upon the acuity of the care situation, the fellow is expected to be able to effectively utilize their resources to arrive at necessary information and to apply the information to their patient care. Moreover, the fellow is expected to recognize conditions and circumstances requiring escalation. Please refer to overview of the fellowship curriculum for competencies/objectives for practice based learning and improvement. Systems Based Practice Goal Fellows must demonstrate an awareness of and responsiveness to the larger context and system of health care, as well as the ability to call effectively on other resources in the system to provide optimal health care. Fellows will work within an interdisciplinary team of health professionals including midlevel providers, pharmacists, nurses, physical therapists, occupational therapists, social workers, care coordinator, and pastoral care. This will provide the fellow experience and feedback in effectively working within an interdisciplinary team of health professionals. Additionally, working within the context of a broader health system includes the importance and necessity to recognize conditions and circumstances requiring consultation and/or escalation for the effective and safe delivery of patient-centered medical care. Please refer to overview of the fellowship curriculum for competencies/objectives for systems based practice. Professionalism Goal Fellows must demonstrate a commitment to carrying out professional responsibilities and an adherence to ethical principles. The fellow is expected to model professional and courteous behavior in the treatment of the patient and in working with the entire health care team. The fellow is expected to complete documentation of their patient care, of their communications with the patient and health care providers, and of their procedures in a timely fashion within the medical record. The fellow is also expected to recognize the critical importance of their own education and the importance of life-long learning as part of their professional responsibility. As such, it is the obligation of the fellow to themselves, their profession, and their patients to attend and complete in a timely fashion all of fellowship training program’s expected educational activities. Please refer to overview of the fellowship curriculum for competencies/objectives for professionalism. Interpersonal and Communication Skills Goal Fellows must demonstrate interpersonal and communication skills that result in the effective exchange of information and teaming with patients, their families, and professional associates. Please refer to overview of the fellowship curriculum for competencies/objectives for interpersonal and communication skills. Teaching Methods Patient care/clinical experience Modeling of observed behaviors of attending physicians and other members of the interdisciplinary team Case-based interactive discussions Didactic sessions Performance feedback Self-directed learning Assessment of Fellow Performance End-of-rotation evaluation of the fellow by the supervising attending physicians Mini-CEX by the supervising attending physicians and/or the nurse practitioner faculty of a counseling and communication encounter Semi-annual self-assessment by the fellow Assessment of Rotation End-of-rotation evaluation of the supervising attending physicians by the fellow Annual program review Discussions with fellows during biannual review Review in-service and ABIM exam results Level of Supervision Indirect supervision with faculty immediately available Direct supervision by the faculty of select patient, family and professional health staff encounters to assess medical knowledge as conveyed in the provided counseling and care coordination, system-based practice, professionalism, and interpersonal communication skills Educational Resources VCUHS Hospital Palliative Care Unit patient care set algorithms and procedures manual UNIPAC Self-Study Program (4th Edition) EPERC Bonica Management of Pain (4th Edition) Bruera Oxford American Handbook of Hospice and Palliative Care Bruera Textbook of Palliative Medicine and Supportive Care Devita, Hellman, and Rosenberg’s Cancer: Principles and Practice of Oncology (9th Edition) UpToDate ASCO University ASCO Practice and Guidelines ASCO-SEP ASH-SEP