Cardiothoracic
advertisement

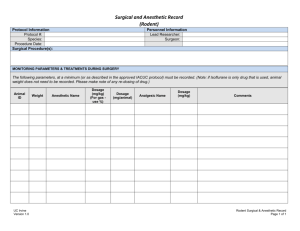
Cardiothoracic Anesthesiology Rotation Curricular Milestones Prepare Anesthesia Work Station 1. Performs appropriate and timely room set up, including standard ASA setup and relevant invasive monitors 2. Prepare emergency drugs, vasoactive infusions, and appropriate drugs for cardiothoracic cases Basic Preoperative Assessment 1. Perform preoperative assessment for patients presenting for cardiac and thoracic surgery. 2.Perform focused history and physical exam 3.Summarize and present key diagnostic data relevant to surgical procedure. 4.Correctly assign ASA classification for patients presenting for cardiac or thoracic surgery. Advanced Preoperative Assessment 1. Identifies any ethical issues which may interfere with standard perioperative care (DNR, Jehovah’s Witness, etc) 2. Demonstrate compassion to the patient and family members presenting for major surgery, while facilitating task completion of entire health care team (surgeon, nursing etc) in a timely manner 3. Incorporates evidenced-based medicine into practice; cites peer reviewed articles 4. Communicates unusual circumstances or anesthetic concerns with surgical team Preoperative Planning for Common Thoracic Surgeries 1. Identify and discuss key anesthetic and perioperative management considerations for common thoracic surgeries including: a) VATS b) Esophagectomy c) Pleurodesis d) Thoracotomy e) Mediastinoscopy f) Bronchoscopy Preoperative Planning for Less Common Thoracic Surgeries 1. Identify and discuss key anesthetic and perioperative management considerations for less common thoracic surgeries including: a) Tracheoplasty b) Tracheal Resection c) Pneumonectomy d) Lung Transplant Preoperative planning for major cardiac surgery (Standard Cardiac Operations): 1. Identify and present the key hemodynamic and perioperative management concerns that must be considered for mitral valve pathology including: a)Mitral Stenosis b)Mitral Regurgitation 2. Identify and present the key hemodynamic and perioperative management concerns that must be considered for aortic valvepathology, including: a)Aortic Stenosis b)Aortic Insufficiency 3. Identify and present the key hemodynamic and perioperative managementconcerns that must be considered for tricuspid and pulmonic valve pathology including: a) Tricuspid Regurgitation b) Tricuspid Stenosis c) Pulmonary Regurgitation d) Pulmonary Stenosis 4. Identify and present the key anesthetic and perioperative management concerns that must be considered for surgery in the setting of ischemic cardiac disease including: a) CABG b) LV dysfunction c) RV dysfunction Preoperative planning for major cardiac surgery (Advanced Cardiac Operations): 1. Identify and discuss key anesthetic and perioperative management considerations for mechanical circulatory support including: a) VAD b) ECMO c) Tandem Heart d) Impella e) IABP 2. Identify and discuss key anesthetic and perioperative management considerations for atypical cardiac surgical scenarios including: a) Pulmonary Hypertension b) LVOT obstruction c) Ablation Procedures d) ASD e) VSD f) TOF g) Heart Transplant 3. Identify and discuss key anesthetic and perioperative management considerations for patients undergoing thoracic aortic surgery including: a) Aortic Dissection- open replacement b) Aortic Dissection- endovascular repair c) Aortic Aneurysm- open replacement d) Aortic Aneurysm- endovascular repair Choice of Anesthesia 1. Identifies possible difficult mask ventilation and/or intubation 2. Has a plan and rationale for induction based upon the patient’s medical history and planned procedure 3. Adjusts induction medications/ technique depending on patient’s co-morbidities 4. Appropriately manages hemodynamics during line placement. Basic Procedures for Cardiac Operations 1. Understands the indications for the invasive monitors placed 2. Understands the contraindications for the invasive monitors placed 3. Places arterial lines, central lines and PAC in a timely fashion 4. Recognizes problems with and troubleshoots invasive monitoring Advanced Procedures for Cardiac Operations 1. Manages epicardial pacing 2. Performs basic TEE assessments (wall motion, ventricular function ventricular filling). 3. Understands conditions that can complicate TEE; places TEE atraumatically Procedures for Thoracic Operations 1. Can correctly place a double lumen endotracheal tube 2. Can discuss, or discuss placement of, a bronchial blocker 3. Can perform basic fiber-optic bronchoscopy, including identification of major anatomic landmarks 4. Recognizes indications and contraindications, advantages and disadvantages of thoracic epidurals 5. Places thoracic epidurals Management of the Pre-Cardiopulmonary Bypass Phase 1. Anticipates the operative phase from skin incision to the initiation of cardiopulmonary bypass 2. Executes the specific tasks required from the anesthesia team immediately preincision through the initiation of cardiopulmonary bypass 3. Describes the cannulation strategy for the case Management of Cardiopulmonary Bypass 1. Describes anticoagulation during cardiopulmonary bypass and can alter plan when traditional dosing fails (e.g. AT3 deficiency management) 2. Can formulate a plan for a patient with HIT/HITT who requires cardiopulmonary bypass 3. Appropriately manages hypotension during cardiopulmonary bypass 4. Manages circulatory arrest 5. Understands the physiologic complications of circulatory arrest at various temperatures 6. Prepares the patient for separation for from CPB Management of Separation from Cardiopulmonary Bypass 1. Gives protamine appropriately and recognizes complications of protamine administration 2. Can give a differential diagnosis of hypotension upon separation from CPB 3. Can discuss how to manipulate the variables contributing to blood pressure and oxygen delivery 4. Understands the different pharmacologic agents used to manage hemodynamics in the setting of cardiac surgery and utilizes invasive monitors to guide decision making for use Management of the Post Bypass Phase 1. Appropriately plans post-operative analgesia 2. Accurately charts in the anesthetic record 3. Identifies patients that are appropriate for extubation 4.Maintains appropriate contact with supervising staff Maintenance of Cardiac Cases Without Cardiopulmonary Bypass 1. Appropriately estimates fluid requirements and administers appropriate fluid type 2. Accurately estimates allowable blood loss and the need for transfusion 3. Manages massive hemorrhage 4. Treats hemodynamic changes in timely and appropriate fashion 5. Appropriately plans post-operative analgesia 6. Maintains accurate anesthestic patient record 7. Maintains appropriate contact with supervising staff General Management of Thoracic Cases 1. Appropriately estimates fluid requirements and administers appropriate fluid type 2. Understands absolute and relative indications for one lung ventilation 3.Uses appropriate tidal volumes during one lung ventilation 4.Can mathematically show minimum necessary saturation for a patient to maintain adequate oxygen delivery 5.Can discuss differential lung perfusion 6. Accurately charts in the anesthetic record 7. Maintains appropriate contact with supervising staff Management of Common Issues During Thoracic Cases 1. Manages hypoxemia during one lung ventilation 2.Recognizes dysfunction/ malposition of bronchial blocker/ DLT and intervenes to resolve the problem. 3. Appropriately identifies when blood transfusion would be beneficial 4. Appropriately treats bronchospasm 5. Manages ventilation in obstructive lung disease 6. Appropriately manages patients with pulmonary hypertension 7. Appropriately plans post-operative analgesia Coordination within operating room environment 1.Perform timely room turnover between cases 2.Utilize anesthesia technicians and pharmacy staff as appropriate 3.Maintain accurate record of controlled substances 4.Arrange transfer of patient to and from the intensive care unit 5.Communicates effectively with the surgical team and operating room Management of Unanticipated Intraoperative Events &Peri-anesthetic complications 1.Identifies, formulates a differential diagnosis and manages unexpected or emergent intraoperative scenarios 2.Understands how to apply ACLS guidelines to the operating room environment 3. Accurately charts in the anesthetic record 4.Maintains appropriate contact with supervising staff 5. With supervision, discusses adverse events with patients and family. Emergence and PACU/ICU Care 1. Prepares the patient for emergence from anesthesia 2. Understands and applies the criteria for extubation 3. Transfer the patient to the PACU/ICU and manages hemodynamics throughout the transition period 4. Provides appropriate hand-off to the PACU/ICU staff 5. Manages common post-operative problems (ie. pain, hypotension, hypertension, PONV) 6. Performs post-operative visits as appropriate Non- Extubation Situations 1. Recognizes that a patient is not appropriate for extubation 2. Plans anesthetic to maintain hemodynamics and sedation during transport 3. Provides appropriate hand-off to ICU staff 4. Performs post-operative visit