DDCMHT.Final-Report-Template

Dual Diagnosis Capability in Mental Health Treatment (DDCMHT)
Report
_____________________________ Team/Program
___________(organization)____________
Date:
Evaluator(s):
The Dual Diagnosis Capability in Mental Health Treatment (DDCMHT) visit was conducted using multiple sources for review. Sources used include chart review, interview with a clinician and client, and physical site tour/observation.
________________________________________________________________
Overall DDCMHT: x.xx on 5.00 scale
Overall Capability: (Dual Diagnosis Capable or Dual Diagnosis Enhanced) ‐ as calculated by average
Highest Level of Dual Diagnosis Capability: (Dual Diagnosis Capable or Dual Diagnosis
Enhanced) ‐ as calculated by 80% rule (Programs are DDC if at least 80 percent of scores are 3’s or greater; Programs are DDE if at least 80 percent of scores are 5))
________________________________________________________________________
Recommendations
The following recommendations serve as DDCMHT Toolkit dimension‐related suggestions to increase the capability to address co‐occurring disorders.
I. Program Structure: x.xx
To enhance the organizational factors that would foster the development of COD treatment, the program may:
Ex. 1. Consider developing a program mission statement that includes a description of the program’s focus on co‐occurring disorders and focus on recovery from co‐occurring mental illness and substance use disorders.
II. Program Milieu: x.xx
To enhance the culture of the program and create an environment that is receptive and welcoming to individuals diagnosed with COD, the program may:
Ex. 1. Provide clients access to literature and educational material on co‐occurring disorders that addresses interactions of co‐occurring disorders on health, ability to find and maintain employment, etc. Printed literature at National Institute of Mental
Health ( www.nimh.gov
) and Substance Abuse and Mental Health Service
Administration ( www.samhsa.gov
).
1
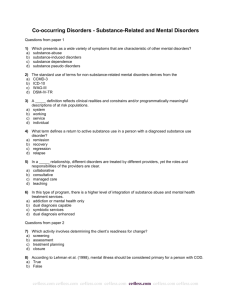
III. Clinical Process: Assessment: x.xx
To enhance specific clinical assessment activities related to COD, the program may:
Exs. 1. Consider routine utilization of a standardized screen with established psychometric properties that explores mental health and substance use disorders.
2. Routinely provide a narrative description of the history and chronology of both disorders, as well as other concerns.
3. Explore opportunities to document motivational stage for multiple presenting concerns, using a standard form that may be re‐administered over time. For example, a. University of Rhode Island Change Assessment (URICA): http://www.uri.edu/research/cprc/measures/urica.htm b. Stages of Change Readiness and Treatment Eagerness Scale (SOCRATES): http://pubs.niaaa.nih.gov/publications/assessingalcohol/instrumentpdfs/SOCRA
TE.pdf
4. Ensure assessment findings inform the treatment planning (i.e. stage‐based treatment), discharge planning, and referral processes.
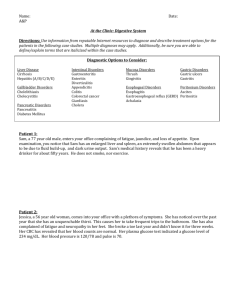
IV. Clinical Process: Treatment: x.xx
To enhance specific clinical treatment activities with relation to COD, the program may:
Exs. 1. On treatment plans, consistently document both mental health and substance use disorders equivalently and in specific detail. When appropriate, include both psychosocial and pharmacological interventions.
2. Throughout treatment, provide documentation of continued assessment and monitoring of both disorders.
3. Develop guidelines and procedures for substance related emergencies (i.e., procedures for intoxicated/high consumers, relapse, withdrawal or active users) and crisis management that include documents formal risk assessment tools or advance directives.
4. Assess differential motivation to address substance use, psychiatric concerns, and pursue recovery goals (e.g., employment, change in relationships) and modify treatment objectives accordingly.
5. Incorporate materials to deliver didactic and informational presentations on cooccurring disorders for program participants in the precontemplation or contemplation stages of change.
2
6. Explore benefit of systematically providing evidence‐based interventions to address addiction or co‐occurring disorders.
7. Consider utilization of stage‐based interventions (e.g., stage‐based groups).
8. Evaluate use of Wellness Recovery Action Plan (WRAP) facilitators and groups, wellness areas and other wellness and recovery supports to promote a recovery lifestyle.
9. Individualize referrals to facilitate involvement with self‐help groups.
10. Routinely incorporate co‐occurring disorder educational sessions (e.g., general information, treatment options, recovery) during interactions with clients, family members or other supporters.
11. Consider ways to incorporate program alumni and other peer supports with cooccurring disorders into the program.
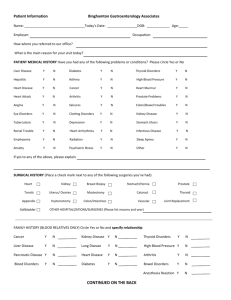
V. Continuity of Care: x.xx
To enhance the long‐term treatment issues and external supportive care issues commonly associated with COD services, the program may:
Exs. 1. Ensure necessary referrals are routinely made, confirmed, and documented in the discharge plan.
2. Create a discharge planning procedure that addresses substance use and mental health concerns in an equal, integrated manner (e.g., the potential impact of recovery of substance use and mental health problems on maintaining wellness and housing.)
3. When appropriate, create and document in the discharge summary a plan to connect the client with family, alumni, or community support groups.
4. Focus on ongoing recovery from both disorders. Encourage staff to embrace the philosophy of recovery equivalently for both mental health and substance disorders.
5. Assertively link clients to peer support groups welcoming to COD.
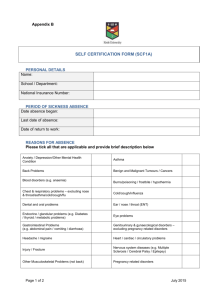
VI. Staffing: x.xx
To enhance staffing patterns and operations that support COD services, the program may:
Exs. 1. Monitor the implementation of COD‐specific services during supervision and the quality assurance process. Implement routine case reviews that support
3
co‐occurring disorder treatment and are policy‐driven.
2. Agency‐wide, utilize supervision as an opportunity to discuss participant quality of care and staff understanding and implementation of best practices (e.g., integrated treatment, stage of change, motivational strategies, process of substance use and mental health recovery).
3. Examine opportunities for psychiatrists or other mental health professionals with whom the program collaborates to act in a teaching role (e.g., offer teaching rounds or a presentation during regularly scheduled agency or program meetings).
4. Explore opportunities to include peers with co‐occurring disorders on‐site as paid or volunteer staff.
5. Consider the benefit of providing supervision that is documented and focused on in‐depth learning of assessment and treatment skill development.
VII. Training: x.xx
To enhance the training and supports that facilitate the capacity of staff to treat individuals diagnosed with co‐occurring disorders, the program may:
Ex. 1. Consider incorporating agency or program training related to COD services into a strategic plan or agency policies.
2. Provide training on substance use disorders for clinical team.
3. Support advanced trainings for clinical staff to increase understanding of pharmacotherapies and competency utilizing specialized interventions.
4