CMHDA California Counties` Continuum of Mental Health Care and
advertisement

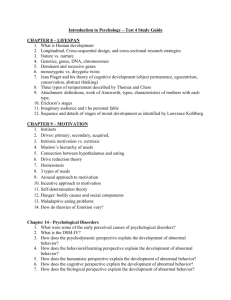
California Counties’ Continuum of Mental Health Care and Medi-Cal Specialty Mental Health “Carve Out” Services for Adults with Serious Mental Illness February 2013 INTRODUCTION The purpose of this document is to provide a concise overview of the continuum of mental health care offered to California’s adults with serious mental illness. In our state, California’s counties administer, directly operate, and contract with local providers to help adults experiencing a serious mental illness to recover and live full, independent lives in the community. This document provides information about the adult clients we serve, the services we provide, and the funds that support California’s public mental health system. For more information, contact the California Mental Health Directors Association at (916) 556-3477 or visit www.cmhda.org. OUR GOALS FOR ADULT CLIENTS As expressed in California’s Bronzan-McCorquodale Acti, the mission of California's mental health system is to “enable persons experiencing severe and disabling mental illnesses and children with serious emotional disturbances to access services and programs that assist them, in a manner tailored to each individual, to better control their illness, to achieve their personal goals, and to develop skills and supports leading to their living the most constructive and satisfying lives possible in the least restrictive available settings.” The President’s New Freedom Commission on Mental Health, which presented its final recommendations to President George W. Bush in 2003ii, identified that successfully transforming the mental health service delivery system rests on these two principles: 1. Services and treatments must be consumer and family centered, geared to give consumers real and meaningful choices about treatment options and providers - not oriented to the requirements of bureaucracies. 2. Care must focus on increasing consumers' ability to successfully cope with life's challenges, on facilitating recovery, and on building resilience, not just on managing symptoms. 1 ADULT CLIENTS SERVED BY COUNTIES The adult target population for California’s public mental health system and Medicaid state plan and waivers are people who are experiencing a serious and disabling mental disorder. o Clients served by county mental health departments are primarily Medi-Cal beneficiaries, although this can vary depending on socioeconomic levels in each county. o Counties also provide mental health services to indigent individuals, to the extent resources are available. o Using prevention and early intervention resources from Proposition 63, counties are also implementing programs to reach individuals with the early signs of mental illness to prevent it from becoming severe or disabling. o The most common diagnoses among our adult clients are: Schizophrenia; Schizoaffective Disorder; Bipolar Disorder; Anxiety Disorders, including Post-Traumatic Stress Disorder; and Major Depression. (See Appendix 1 for a basic overview of these mental health conditions). What is a “serious and disabling” mental disorder? The clinical terms in state lawiii Severe and persistent; and May cause behavioral functioning that interferes substantially with the primary activities of daily living, and may result in an inability to maintain stable adjustment and independent functioning without treatment, support, and rehabilitation for a long or indefinite period of time What do these terms mean? A severe illness with complex symptoms, requiring ongoing treatment and management. The illness is “chronic”, similar to diabetes, asthma, or high blood pressure, which are not temporary, must be managed over the lifespan, and tend to worsen if left untreated. Due to a mental disorder, the person may have difficulty with basic and important activities of daily living (eating, bathing, dressing, shopping, budgeting, household chores), with important social relationships, or with working and sustaining an income and housing. There is currently no cure for mental illness, and left untreated, mental illness can be disabling and lead to other health complications or even suicide. However, people with mental illness can and do recover every day after receiving evidence-based medications, treatments, and services. Medi-Cal beneficiaries with serious mental health needs that cannot be met within a primary care physician’s scope of practice receive specialty mental health services and supports that are administered by counties. These services are often described as “carved out” because they are not provided by the Medi-Cal managed care plans, but are provided by counties instead because of their specialized nature. County mental health plans (MHPs), which are the county mental health departments throughout the state, perform this function under the state’s Specialty Mental Health Services (SMHS) Consolidated Medicaid Waiver. 2 California’s Medi-Cal beneficiaries whose needs are less serious can access basic mental health services, such as prescription medications and appointments with psychiatrists, through the state’s Medi-Cal feefor-service system or through their Medi-Cal managed care plan.iv Medi-Cal beneficiaries are eligible to receive “carved out” Medi-Cal specialty mental health services from the counties if they meet the medical necessity criteria in state regulations, described in the table below. Who receives “carve out” Medi-Cal Specialty Mental Health? Medical necessity criteriav 1) Diagnosed, qualified mental disorder; What do these criteria mean? One of 18 diagnoses in the Diagnostic and Statistical Manual of Mental Disorders (DSM).vi 2) Experiencing a significant impairment in an important area of life functioning, or a reasonable probability of significant deterioration in an important area of life functioning; and Due to a mental disorder, the person may have difficulty with basic and important activities of daily living (eating, bathing, dressing, shopping, budgeting, household chores), with important social relationships, or with working and sustaining an income and housing. 3) The focus of the intervention is to address the resulting impairment condition, the service is expected to significantly improve the condition, and the condition would not be responsive to physical health case based treatment. Effective interventions are used with clients, and the services will help – not harm – the individual. COUNTIES ADMINISTER A BROAD CONTINUUM OF EMERGENCY AND REHABILITATIVE SERVICES Counties provide a broad continuum of voluntary, outpatient mental health services and supports. Involuntary psychiatric hospitalization only occurs when a person, due to a mental disorder, poses harm to their self or others, or is gravely disabled (cannot provide basic needs). The services are individualized and are based on each person’s needs and goals, are evidence-based, and are linguistically and culturally appropriate. Services are community-based and mobile, not just clinic-based. Services and provider qualifications funded by the Mental Health Services Act (Proposition 63) are described in state law and regulations. Medi-Cal Specialty Mental Health services and provider qualifications are described in state regulations and California’s Medicaid State Plan, Medi-Cal Specialty Mental Health Consolidated Medicaid Waiver, and two Medicaid state plan amendments (SPAs) – Rehabilitative Services and Targeted Case Management. In particular, California’s Rehabilitative Services SPA and Prop. 63 provide county mental health departments with funding and tools to do more than just treat the medical symptoms of an illness. 3 Taken together, these services help address the whole person – from the symptoms of their mental illness, to their ability to successfully live and work in the community. See Appendix 2 for a comprehensive list of the services counties administer. COMMUNITY-BASED, RATHER THAN CLINIC-BASED, SERVICES To be as accessible and responsive to individuals’ diverse needs as possible, service settings are diverse and strive to be as community-based and culturally appropriate as possible. Services are offered in what one may think of as “traditional” settings, such as mental health clinics, hospitals, and long-term care facilities. However, significant portions of our services are offered outside of clinical settings, including wellness centers, individuals’ homes, schools and colleges, jails and courts, and on the streets or in homeless shelters. Adults access public mental health services through a variety of sources, including by referring themselves for help. Referrals to counties and community providers come from family members, guardians, conservators, physicians, hospitals, county welfare departments, and law enforcement agencies. Additionally, all counties operate a 24/7 toll-free access hotline and emergency services, which are available to all community members. WIDE ARRAY OF PROVIDERS Services are provided by an array of professionals, paraprofessionals, consumers, and family members, the variety of which far exceed what is traditionally available in primary care settings. These include: o Psychiatrists o Psychologists o Licensed Clinical Social Workers o Licensed Marriage and Family Therapists o Licensed Professional Clinical Counselors o Licensed Psychiatric Technicians o Mental Health Rehabilitation Specialists o Physicians and Physician Assistants o Registered Nurses, Certified Nurse Specialists, Licensed Vocational Nurses, Nurse Practitioners o Pharmacists o Occupational Therapists o Peers and family members Counties also partner with others in the community, including schools, law enforcement, health clinics, hospitals, churches, and county social services, child welfare, and substance use disorder services. 4 FUNDING SOURCES SUPPORTING THE CONTINUUM OF CARE As depicted in the pie chart below, the largest funding source (about one-third) for California’s community mental health services is federal Medicaid reimbursement. One-quarter of funds are from the Mental Health Services Act (Prop. 63), and the remaining funds come from state sales tax revenues, provided by 1991 and 2011 Realignment. Some counties also provide local funds, and a small amount of federal grant funds are available. Counties coordinate other third-party reimbursement, such as Medicare and private insurance. Estimated California Community Mental Health Funding in FY 2012-13 (Total: $4.865 billion) Other $185 million Federal Medicaid $1.7 billion 2011 Realignment $780 million 15% 35% 23% 23% Prop. 63 $1.1 billion 1991 Realignment $1.1 billion Note: These are estimated amounts for fiscal year 2012-13. Actual amounts depend largely on economic performance of state sales tax, Vehicle License Fees, and personal income tax revenues. These funding sources do not operate in silos – they are used in a complementary fashion to meet each client’s unique needs, while maximizing federal Medicaid reimbursement. For example, a Medi-Cal beneficiary may need psychotherapy and assistance managing their symptoms. The county could use 1991 or 2011 Realignment funds as match to provide these Medi-Cal specialty mental health services, and to receive federal Medicaid reimbursement. However, the beneficiary may also need assistance with housing, which the county could provide using Prop. 63 funds. 5 Major Funding Sources for Community Mental Health in California Federal Medicaid – Federal funds that reimburse counties (generally 50%) for medically necessary services provided to Medi-Cal Specialty Mental Health beneficiaries. Funds takes an average of 2 years after a service is delivered/claimed to be distributed to counties. Funds from all of the sources listed below are used as match to the greatest extent possible to draw down these federal funds. 1991 Realignment – Dedicated sales tax revenues distributed to counties to provide: emergency evaluation and treatment for persons who are a danger to self/others or gravely disabled; long-term nursing care; state hospital care; hospitalization in skilled nursing facilities licensed as Institutions for Mental Disease. Most services funded by this source are not permitted to be funded by other sources. Proposition 63 – The Mental Health Services Act, passed by voters in 2004, provides personal income tax revenues (surcharge on incomes above $1 million) to counties to expand services to people of all ages with serious mental health issues and build upon evidence-based, effective service models. It also requires that a specific percentage of funding to be used for prevention and early intervention services. 2011 Realignment – Dedicated sales tax revenues distributed to counties to provide medically necessary services to Medi-Cal Specialty Mental Health beneficiaries, including Early and Periodic Screening, Diagnosis and Treatment mental health services to children and adolescents. Other – Some counties provide county general funds or receive federal block grant funds. 6 APPENDIX 1 Adult Serious Mental Illnesses: A Basic Overview Schizophrenia Schizophrenia most often appears in men in their late teens or early twenties, while it appears in women in their late twenties or early thirties. Interfering with a person's ability to think clearly, manage emotions, make decisions and relate to others, schizophrenia impairs a person's ability to function to their potential when it is not treated. Psychosis, a common symptom of schizophrenia, is the experience of loss of contact with reality and usually involves hallucinations and delusions. Along with medication, psychosocial rehabilitation and other community-based support can help those with schizophrenia go on to lead meaningful and satisfying lives. Schizoaffective Disorder Schizoaffective disorder has features that resemble both schizophrenia and also serious mood symptoms. It affects 1% of adults in the US. Schizoaffective disorder is thought to be between the bipolar and schizophrenia diagnoses as it has features of both. Most experts believe it is a type of chronic mental illness that has psychotic symptoms at the core, and with depressive and manic symptoms as a secondary—but equally debilitating—component. For most people with schizoaffective disorder, treatment will be very similar to treatment of schizophrenia and will include antipsychotic medications to help address symptoms of psychosis. Bipolar Disorder Bipolar disorder is a serious brain disorder that causes extreme shifts in mood, energy, and functioning. It is characterized by intense emotional states known as mania and depression, which can last from days to months. It affects 1.2% of adults in the US. A manic state can be identified by feelings of extreme irritability and/or euphoria, along with several other symptoms during the same week such as agitation, surges of energy, reduced need for sleep, talkativeness, pleasure-seeking and increased risk-taking behavior. Depression is identified by feelings of extreme sadness, hopelessness, and loss of energy. Bipolar disorder is a chronic and generally life-long condition with recurring episodes that often begin in adolescence or early adulthood, and occasionally even in children. While there is no cure for bipolar disorder, it is a treatable and manageable illness once it is correctly diagnosed. Anxiety Disorders Anxiety disorders include panic disorder, obsessive-compulsive disorder, post-traumatic stress disorder, generalized anxiety disorder, and phobias (such as social phobia, agoraphobia, etc.). They affect 13.3% of adults in the US. Panic disorder is characterized by “panic attacks,” and results in sudden feelings of terror that can strike repeatedly and sometimes without warning. Obsessive-compulsive disorder is characterized by repetitive, intrusive, irrational and unwanted thoughts (obsessions) and/or rituals that seem impossible to control (compulsions). Post-traumatic stress disorder (PTSD) is an anxiety disorder that can occur after someone experiences a traumatic event that caused intense fear, helplessness, or horror. PTSD can result from personally experienced traumas (e.g., rape, war) or from the witnessing of or learning of a violent or tragic event. Major Depression Depression is a biological disorder that results in a syndrome of sleeping, eating and energy disturbance that impairs functioning and may lead to suicide. Depression is not just a bad day, the blues or being moody. It affects approximately 5% of adults in the US. Among all major medical illnesses, major depression is the leading cause of disability in America. Unlike normal emotional experiences of sadness, major depression is persistent and can significantly interfere with an individual’s thoughts, behavior, mood, activity, job productivity and physical health. Although major depression can be a devastating illness, it is highly treatable. Between 80 and 90% of people living with serious depression can be effectively treated and return to their normal daily activities and feelings. Sources: National Alliance on Mental Illness (NAMI), Primer on Depressive, Bipolar and Anxiety Illnesses: Facts for Policymakers and NAMI: What is Mental Illness? 7 APPENDIX 2 What kinds of services are provided by counties? Service types What is the purpose? COMMUNITY-BASED, OUTPATIENT SERVICES Outreach, engagement, and screening Programs and activities to identify un-served individuals who are eligible for public mental health services in order to engage them, and when appropriate their families, so that they receive the appropriate services Assessment and diagnosis Client assessments include things such as the chief complaint and history of the presenting problem, current level of functioning, family history, relevant cultural issues, client strengths, medical and mental health history, substance use, mental status exam, and complete diagnosis from the most current DSM Client plan Plans are developed at least annually with the client. Plans include specific goals and treatment objectives; proposed types, frequency, and duration of interventions; address recovery and resiliency supports; and address identified functional impairments as a result of the mental disorder Full Service Partnership Targeted to people who need a range of services and supports in order to recover, providing 24/7 assistance with housing, employment, education, mental health supports, physical health care, clothing, food, or other services Counseling and psychotherapy Focuses on reducing symptoms, restoring functioning, and improving coping and adaptation, including modifying feelings, thoughts, attitudes or behaviors that are ineffective in the person’s life Prevention and early intervention Efforts to reduce the stigma associated with mental illness, offering services to individuals with the earliest signs of illness, serving high-risk students in schools, and suicide prevention programs Non-mental health services and supports This can include food, clothing, housing (rent subsidies, housing vouchers, house payments, residence in a drug/alcohol rehabilitation program, transitional and temporary housing), respite care, or the cost of other health care Peer and family member supports Services and supports provided by mental health clients and their family members to support wellness, recovery, and resiliency (Continued from previous page) To identify individuals who may need mental health services and supports To determine what mental illness issues may be affecting the individual To identify the goals and services desired by the client and provider To reduce the negative outcomes that result from untreated mental illness, including suicide, incarceration, school failure or dropout, unemployment, prolonged suffering, homelessness, and removal of children from their family homes To alleviate psychological distress and provide support, education, and guidance, and to assist in developing adaptive thinking and skills To prevent mental illnesses from becoming severe and disabling To support an individual in living successfully in the community To help people connect and get guidance from others who have experienced mental illness (Table continued on next page) 8 What kinds of services are provided by counties? Service types Medication support Prescribing, administering, dispensing, and monitoring prescription drugs; education on risks, benefits, and side effects Targeted case management Services to assist individuals in gaining access to needed medical, alcohol and drug treatment, educational, and other services Crisis intervention A field-based, unplanned, expedited, emergency service enabling an individual to cope with a crisis and assist the individual in regaining their status as a functioning community member Crisis stabilization An unplanned, expedited service lasting <24 hours in a licensed setting to address an urgent condition requiring immediate attention that cannot be addressed safely or adequately in a community setting What is the purpose? To effectively alleviate symptoms To help individuals obtain needed services To avoid hospitalization and stabilize an immediate crisis within a community or clinical treatment setting To avoid the need for inpatient services which, if the condition/symptoms are untreated, present an imminent threat to the individual/ others, or could result in them becoming gravely disabled INPATIENT, LONG-TERM CARE SERVICES Crisis residential treatment Short-term (<3 mos.), 24/7 therapeutic/rehabilitative services in a non-institutional residential setting as an alternative to hospitalization for individuals in an acute psychiatric episode or crisis who do not require nursing care for medical complications. Includes counseling, developing a community support system, skillbuilding, and socialization Residential treatment Recovery focused, 24/7 rehabilitative services provided in a noninstitutional residential site for individuals otherwise at risk of hospitalization or institutional placement that includes counseling, developing a community support system, skill-building, and socialization Day rehabilitation Structured program offered 3+ hrs/day to a group of individuals, including rehabilitation, skill building and process groups, to improve or restore independence and functioning in order to live in the community Day treatment intensive Structured, multidisciplinary program offered 3+ hrs/day to a group of individuals, intended as an alternative to hospitalization or to avoid more restrictive placements and assist individuals in living in community settings To provide an alternative to hospitalization and restore, improve, or preserve an individual’s interpersonal and independent living skills and access to community support systems that support recovery and enhance resiliency To minimize the risk of hospitalization and restore, improve, or preserve an individual’s interpersonal and independent living skills and access to community support systems that support recovery and enhance resiliency To improve independence and assist in living in the community To avoid hospitalization and assist in living in the community (Table continued on next page) 9 What kinds of services are provided by counties? Service types (Continued from previous page) What is the purpose? Psychiatric health facility services Therapeutic/rehabilitative, multidisciplinary services provided in a locked, licensed, psychiatric health facility for individuals who do not have a physical illness/injury that requires inpatient treatment. Services include psychiatric, psychosocial, counseling, rehabilitative, and social services To provide a less costly alternative to psychiatric inpatient hospitalization for individuals who, due to a mental disorder, have been determined to be a danger to themselves or others Psychiatric inpatient hospitalization Services provided by a free-standing psychiatric hospital (or psychiatric unit of a general hospital) for diagnosis or treatment of a mental disorder that cannot be effectively or safety treated in an outpatient setting Mental health rehabilitation centers Licensed, locked centers that provide 24/7, long-term, intensive support and rehabilitation services to assist adults with mental disorders to develop the skills to become self-sufficient and capable of increasing levels of independent functioning Locked skilled nursing facilities Licensed, locked nursing facilities that provide 24/7 long-term, intensive support. Individuals often have co-morbid medical or substance use disorders State hospitals State hospitals, operated by the California Department of State Hospitals, provide 24-hour long-term care, treatment and education in a locked, institutional setting to individuals who, due to a mental disorder, have been civilly committed, determined to be gravely disabled, and have a court-appointed guardian To treat an acute episode of mental illness for individuals who, due to a mental disorder, have been determined to be a danger to themselves or others To provide an alternative to state hospital or other mental health facility placements for individuals who, due to a mental disorder, have been determined to be gravely disabled and have a court-appointed guardian To treat individuals who, due to a mental disorder, have been determined to be gravely disabled and have a court-appointed guardian To provide care, treatment, and education to individuals who, due to a mental disorder, have been determined to be gravely disabled and have a court-appointed guardian Note: This is a comprehensive, but not fully exhaustive list of the defined mental health services that counties administer. Additional details can be found in state regulations and California’s Medicaid Waivers and State Plan Amendments. 10 DRAFT END NOTES i Welfare and Institutions Code 5600.1 ii New Freedom Commission on Mental Health, Achieving the Promise: Transforming Mental Health Care in America. Final Report. DHHS Pub. No. SMA-03-3832. Rockville, MD: 2003. iii Welfare and Institutions Code 5600.3 iv As part of their responsibility for coordination of care, Medi-Cal managed care plans must have written policies and procedures to ensure that they assist members who need mental health services that the plan does not cover. If the member has a tentative psychiatric diagnosis that meets eligibility criteria for specialty mental health services, the managed care plan must make appropriate referrals to the county MHP. If the member has a psychiatric diagnosis that the county MHP does not cover, the managed care plan must refer them to an appropriate fee-for-service Medi-Cal mental health provider and must consult with the county MHP as necessary to identify other appropriate community resources and help the member to locate available mental health services. Their contracts with the state require them to negotiate in good faith and execute a Memorandum of Understanding with the MHP. The MOU must specify the respective responsibilities and protocols of the Medi-Cal managed care plan and the MHP in delivering medically necessary covered services and specialty mental health services to members. v 9 CCR § 1830.205 and 1805.210 vi The 18 DSM diagnoses that are part of medical necessity criteria for Medi-Cal beneficiaries to obtain specialty mental health services that are the responsibility of the MHP are: (A) Pervasive Developmental Disorders, except Autistic Disorders; (B) Disruptive Behavior and Attention Deficit Disorders; (C) Feeding and Eating Disorders of Infancy and Early Childhood; (D) Elimination Disorders; (E) Other Disorders of Infancy, Childhood, or Adolescence; (F) Schizophrenia and other Psychotic Disorders, except Psychotic Disorders due to a General Medical Condition; (G) Mood Disorders, except Mood Disorders due to a General Medical Condition; (H) Anxiety Disorders, except Anxiety Disorders due to a General Medical Condition; (I) Somatoform Disorders; (J) Factitious Disorders; (K) Dissociative Disorders; (L) Paraphilias; (M) Gender Identity Disorder; (N) Eating Disorders; (O) Impulse Control Disorders Not Elsewhere Classified; (P) Adjustment Disorders; (Q) Personality Disorders, excluding Antisocial Personality Disorder; and (R) Medication-Induced Movement Disorders related to other included diagnoses. (See: 9 CCR Section 1830.205) 11