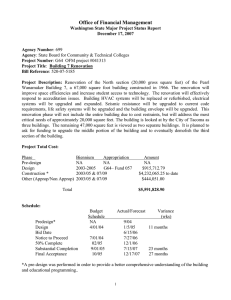
Date - Design Organization
advertisement
DESIGN ORGANIZATION, INC. Planning Architecture Interior Design 300 W. Hubbard Street, Suite 201 Chicago, Illinois 60654 Tel (312) 324-5500 Fax (312) 324-5501 April 19, 2011 Healthcare Equipment and Technology Integration. In the world of healthcare architecture, design must accommodate technology – not just today, but also in the future. That may be easier said than done, but necessary to serve clients’ best interests. On some projects, we are fortunate enough to know what equipment a hospital has selected. But frequently, to meet schedule expectations, planning must proceed before final equipment. So, why do we find ourselves designing spaces without knowing equipment and systems requirements? Hospital clients may be comparing competing equipment performance and pricing. Other times, all-important hospital/physician partnerships aren’t yet clearly defined. And sometimes, hospitals/physicians are still investigating emerging technology – waiting for the most advanced equipment to be unveiled. Whatever the reason, it happens. And it’s our job to create spaces that anticipate decisions that are yet to come. How do we anticipate and accommodate those decisions? Most importantly, process driven decision-making is an absolute requirement to meet expectations, and the needs of project stakeholders. Developing a detailed decision matrix/schedule should be a collaborative effort of the A/E team, specialty consultants (physicist, shielding), equipment supplier, and contractor. And, if equipment isn’t selected, we also incorporate estimated shop/installation drawings and delivery/installation timeframes into the plan by gathering information from potential suppliers. If we must begin the design process without selections - as we recently did on a Franciscan Alliance Cancer Treatment Center – we’ll create a universal floor plate to accommodate a wide range of equipment types and/or configurations. This can be done with any number of diagnostic and treatment modality rooms. Remember, it’s not if - but when - technology will change, so rooms should be flexible. Access for future equipment replacement must also be addressed. Increasing corridor width or integrating a roof hatch in the early stages of design is inexpensive, especially compared to destructive demolition for something such as an MRI equipment change later. Of course, not all projects are new construction. At the University of Chicago Medical Center, Design Organization recently completed the renovation of the MRI diagnostics Suite with new 3.0 T. and 1.5 T rampable to a 3.0 T MRI’s. Located within an internal courtyard completely surrounded by buildings, the Q-Building was not easily accessible. The existing multi-ton MRI units and chiller needed to be lifted into the courtyard over an existing three story building and maneuvered into openings created in the building’s curtain wall. It was also imperative that areas of the third floor remain accessible to students who utilized two computer rooms daily throughout the construction process. In addition to the difficult site and phasing constraints, we were asked to provide a solution to ensure that the noisy MRI equipment would not disrupt the activities in the spaces below the units on the second floor which included a lecture room and the radiology staff offices. Considerations driving renovation and alternate re-use of existing space are efficient use of resources, limited land for expansion and/or accelerated schedules. We worked with IU Health LaPorte Hospital on a master facility plan that called for increased cardiology services. With limited land to expand, the only space available with proximity to existing cardiology was Radiation Oncology which was being relocated out of the hospital. We were able to renovate the LINAC Vault as a Heart Catheterization Lab with minimal demolition. The adjacent space with larger column spacing was able to accommodate the new Electrophysiology Lab, the only one of it’s kind in the Midwest that features, the only integrated GE Biplane fluoroscopy, Cardiolab XT EP monitoring and Vivid q Cardiovascular ultrasound systems, a Biosense Webster CARTO 3 Mapping System, and Hansen Sensei Robotics. The quantity of ceiling supported equipment, raceways, structure, etc, was more like making a swiss watch. This is an example of the importance of thorough due diligence/field investigation before design on any renovation project. This effort is not just in the project area, but also in the evaluation of core systems for adequacy and access to serve the new function. The early definition and understanding of total scope allows the project team to effectively estimate costs and to develop accurate documents limiting field changes. As with many renovation projects, a phasing plan is needed to minimize disruption and address infection control. Working with multiple hospital departments and the contractor we develop an implementation plan that is communicated to all owner stakeholders. When construction begins, the same collaborative effort of the owner stakeholders, design team, contractor, equipment vendor and installers continues through punch-list. Always close the loop. When equipment installation drawings are completed there needs to be a thorough review of earlier assumptions and documentation. In the electronic age, if possible, we still prefer to have a check-set with arch/structural/MEPFP/equipment vendor/contractor all in the room together. We then update our Revit BIM Documents to additionally guard against conflicts and change orders. In the end, it’s about working together and keeping all stakeholders involved. Whether it’s new construction, renovation, or any other unique challenge that may arise, the key is seeking input, being responsive and remaining available throughout the entire process. By adhering to these principles, we’re better able to serve our clients, and ultimately, their patients. Design Organization Inc. Spero Valavanis AIA, LEED AP President