Sensitivity in children with steroid
advertisement

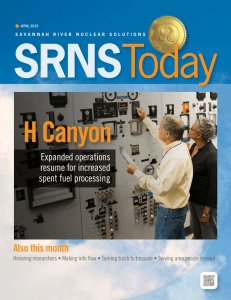
O52 INITIAL STEROID-SENSITIVITY IN CHILDREN WITH STEROID-RESISTANT NEPHROTIC SYNDROME PREDICTS POST-TRANSPLANT RECURRENCE Wen Y Ding1,2*, Ania Koziell4,5*, Hugh J McCarthy1,2, Agnieszka Bierzynska2, Murali K Bhagavatula3, Jan A Dudley1, Carol D Inward1, Richard J Coward1,2, Jane Tizard1, Christopher Reid4, Corinne Antignac6, Olivia Boyer6, Moin A Saleem1,2 1. Department of Paediatric Nephrology, Bristol Royal Hospital for Children 2. Academic Renal Unit, University of Bristol 3. Children’s Hospital for Wales 4. Department of Paediatric Nephrology, Evelina Children’s Hospital 5. Department of Experimental Immunobiology, King’s College London 6. Néphrologie Pédiatrique & INSERM U983, Hôpital Necker-Enfants Malades *Joint first authors INTRODUCTION: Steroid-resistant nephrotic syndrome (SRNS) is a disease with significant morbidity where many affected children progress to end-stage renal failure (ESRF). 30-50% of transplanted patients suffer from a recurrence of disease and as yet, we have no robust clinical or biochemical indicators that predict recurrence. A proportion of SRNS is genetic, and studies have shown that those with mutations are resistant to immunosuppression but have a low posttransplant recurrence rate of 0-3%. It is believed that an immunologically-derived circulating factor underlies post-transplant recurrence of SRNS. We hypothesised that SRNS can be broadly classified into 2 groups: those with a genetic mutation who are immunosuppression resistant with low post-transplant recurrence rates; and those with a circulating factor who initially respond to steroids with high post-transplant recurrence rates. METHODS: We retrospectively reviewed 150 paediatric SRNS patients who received transplants at the 3 large European paediatric nephrology centres. We collected data on clinical characteristics including sex, race, age at diagnosis, time to ESRF, time on dialysis, age at transplant, initial steroid-sensitivity at presentation, genetic mutations, family history, extrarenal abnormalities, recurrence, rejection, and graft loss. RESULTS: 25/150 children had genetic or familial SRNS and none of these showed recurrence post-transplant. Of the remaining 125 patients, 57/125 (45.6%) patients developed posttransplant recurrence. 26/29 (89.7%) patients with initial steroid-sensitivity recurred posttransplant while only 26/86 (30.2%) of those resistant from the outset recurred (p<0.0001; OR=30, 95%CI=6.62 to 135.86). (Figure 1) We were unable to determine recurrence in 2 patients and 8 patients did not receive steroids. CONCLUSION: Our data shows for the first time that initial steroid-sensitivity is highly predictive for post-transplant disease recurrence. Steroid-resistance from the outset and/or genetic mutation significantly diminished risk. We propose that initial steroid response is a surrogate marker for circulating factor disease, and show that this progresses to posttransplantation recurrence in approaching 100% of patients. These findings will enable patients to be counselled appropriately and targeted for intensive therapy in the earlier stages of their disease as well as during the peri-transplant period. Figure 1 Forest plot for odds ratios for recurrence Age at Diagnosis<6 years Time to ESRF<3 years st Age of 1 Transplant<12 years Time on dialysis<2 years African-European Donor Type Initial Steroid Sensitivity 0.1 1 10 Odds ratio for recurrence 100 1000