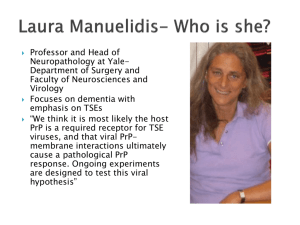
Manuelidis web site statements
advertisement

BBS Program Yale University New Haven, CT 06520Fax: 203.785.3734bbs@yale.edu Laura Manuelidis MD Professor of Surgery (Neuropathology); Section Chief Neuropathology (Surgery) Research Interests Clinical and experimental models of dementia with an emphasis on Transmissible Encephalopathies (TSEs); Chronic viral infections of the nervous system Research Summary The Section of Neuropathology focuses on clinical and experimental models of dementia, with an emphasis on Transmissible Encephalopathies (TSEs) such as human Creutzfeldt-Jakob disease (CJD), and endemic sheep scrapie. Our goal is to elucidate the nature of the infectious agent, and to delineate how the host responds to infection. Many pre-senile dementias of unknown etiology, such as Alzheimer's Disease, may share common host-activated neurodegenerative pathways. We established the first rodent models of human CJD in the 1970s. An infectious agent that has many viral characteristics causes this progressive neurodegenerative disease. As many "neurotropic" viruses, the TSE agent can spread though the blood (1,2) to infect lymphoreticular tissues such as the spleen and lymph nodes before invading the brain. At this stage, the infection is clinically inapparent or latent. Extensive Research Description The Section of Neuropathology focuses on clinical and experimental models of dementia, with an emphasis on Transmissible Encephalopathies (TSEs) such as human Creutzfeldt-Jakob disease (CJD), and endemic sheep scrapie. Our goal is to elucidate the nature of the infectious agent, and to delineate how the host responds to infection. Many pre-senile dementias of unknown etiology, such as Alzheimer's Disease, may share common host-activated neurodegenerative pathways. We established the first rodent models of human CJD in the 1970s. An infectious agent that has many viral characteristics causes this progressive neurodegenerative disease. As many "neurotropic" viruses, the TSE agent can spread though the blood (1,2) to infect lymphoreticular tissues such as the spleen and lymph nodes before invading the brain. At this stage, the infection is clinically inapparent or latent. Nevertheless, the host recognizes the agent as foreign (unlike its own prion protein), and activates many innate immune responses before clinical signs of disease develop (3,4). None of these host responses are sufficient to stop the progressive infection, and effective treatment will probably require a rigorous molecular definition of the infectious particle. Infectious particles isolated from the brain are spherical show with a discrete viral size of 25nm in diameter corresponding to a molecular weight of ~5x10e3 kDa by high pressure liquid chromatography. They also have a homogeneous viral density (1.28gm/cc) in sucrose, a good indication that they contain a protected viral genome (reviewed in 5). Although agent-specific nucleic acid sequences have not been defined, nucleic acids more than 500nt long have been extracted from infectious 25nm particle-rich fractions. Recently, we identified arrays of similarly dense 25nm viruslike particles in situ within infected but not control cells in culture (6). Arrays of these particles are shown in the Electron micrograph at the right, where the bar is 100nm and several dense particles cut in cross-section are marked by arrows. Neither the isolated 25nm particles from brain fractions, nor those visualized in intact cells contain abnormal prion protein (PrP) as determined by antibody binding studies. In contrast, PrP antibodies did label abnormal PrP amyloid fibers as expected. This PrP amyloid was physically separated from the viruslike arrays in the cell. It is commonly assumed that PrP amyloid is the infectious agent. However, there is no reproducible evidence that this protein can infect animals and humans. Indeed, many studies show infectious particles are separate from PrP multimers and aggregates in accord with our initial gradient purifications. We think it most likely that host PrP is a required receptor for TSE viruses, and that viral-PrP membrane interactions ultimately cause a pathological PrP response. Ongoing experiments are designed to test this viral hypothesis. On a public health level, a more virulent TSE agent has recently evolved in cows ("mad cow disease"), and has spread to humans and a variety of other species. There is also a spreading epidemic from yet another strain of TSE in the deer (cervid) population of the USA. It is not known if this TSE agent in cervids will infect humans. One of the most intriguing questions in the TSE field is what limits the natural spread and pathological sequelae of individual TSE agent strains. TSE strains maintain their identity despite various changes in prion protein (7). This fact strongly implicates a relatively stable but mutable viral genome. The figure below shows how dramatically TSE agents can differ in their capacity to evoke pathological sequelae. Section A below shows the brain lesions after infection with a typical attenuated sporadic CJD strain (sCJD) from humans. This agent provokes pathology and abnormal prion protein (red at arrow) only in a very small region of the thalamus and terminal disease only after >350 days when passaged in mice. In contrast, section B shows the widespread deposits as in the hippocampus (H) caused by a more virulent geographic CJD agent isolated from a patient in Japan. This strain has not been found in the USA or Europe, and causes death in as little as 120 days in a mouse. Remarkably, the less virulent sCJD strain can interfere with superinfection by the more virulent Japanese CJD agent. This viruslike protection against a related challenge strain can last for the lifetime of a mouse. Furthermore since no pathological PrP can be detected, abnormal PrP is not involved in this viruslike protection (8). Similar protection, without PrP involvement, has also been documented here in a simplified cell culture system (9). Cultures offer new opportunities to resolve fundamental questions as well as to rapidly assess preventive and treatment strategies. These may also lead to the development of effective preventive vaccines. Selected Publications Nishida N, Katamine S, Manuelidis L. Reciprocal interference between specific CJD and scrapie agents in neural cell cultures. Science. 2005 310(5747):493-6. PMID: 16239476 Manuelidis L. A 25 nm virion is the likely cause of transmissible spongiform encephalopathies.J Cell Biochem. 2007 100(4):897-915. PMID: 17044041 Manuelidis, L, Liu, Y, Mullins, B.: Strain-specific viral properties of variant Creutzfeldt–Jakob Disease (vCJD) are encoded by the agent and not by host prion protein. J Cell Biochem 106:220–231, 2009. Manuelidis, L, Chakrabarty, T, Miyazawa, K, Nduom, N-A, and Emmerling, K. The kuru infectious agent is a unique geographic isolate distinct from Creutzfeldt–Jakob disease and scrapie agents. Proc. Natl. Acad. Sci. USA 106: 13529-13534, 2009.