Report HPV - Final4
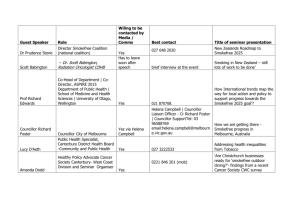
advertisement
Incorporating Systematic Smokefree Practice in the Hawke’s Bay District Health Board HPV Vaccination Programme report prepared by David Smith 29 June 2010 Smith Consulting Ltd phone: (03) 315 7763 mobile: (0274) 311 212 fax: (03) 315 7764 e-mail: smith.consulting@xtra.co.nz 1. Contents 1. Contents .............................................................................................................. 2 2. Executive Summary ............................................................................................. 3 3. Recommendations ............................................................................................... 4 4. Background ......................................................................................................... 5 5. Literature Review ................................................................................................. 7 5.1. HPV ........................................................................................................... 7 5.2. Smoking Cessation ................................................................................... 8 6. Description of the HPV vaccination programme .................................................. 9 7. Key Smokefree Messages ................................................................................. 10 8. Education plan and resource development ........................................................ 11 9. 8.1. Education ................................................................................................ 11 8.2. Resources ............................................................................................... 12 Staff perceptions ................................................................................................ 13 9.1. Importance of ABC Smokefree Practice .................................................. 13 9.2. Legitimacy of ABC Smokefree Practice ................................................... 13 9.3. Clarity of Process Expectations ............................................................... 14 9.3.1. Design ........................................................................................... 14 9.3.2. System/Process ............................................................................ 15 9.4. Education ................................................................................................ 15 9.5. Resources ............................................................................................... 16 9.6. Roles ....................................................................................................... 16 10. Client Perceptions.............................................................................................. 17 11. Preliminary Audit – April 2010 ........................................................................... 18 11.1. Results .................................................................................................... 18 11.2. Comments ............................................................................................... 18 12. Appendices ........................................................................................................ 20 12.1. APPENDIX 1 - Bookmark Resource........................................................ 20 12.2. APPENDIX 2 - Recording Sticker ............................................................ 21 12.3. APPENDIX 3 - Session Outline – 20 minute presentation ....................... 22 Page 2 of 23 2. Executive Summary Smokefree ABC practice was formally incorporated into the HPV screening programme following initial discussions between the team’s manger and the HBDHB Maternal, Child and Youth Services smokefree coordinator. The rationale was that smoking was directly linked to increased risk of HPV infection and subsequent cervical cancer and that brief smokefree intervention by health professionals is an effective strategy in supporting those who currently smoke to become smokefree. Consultation among the HPV team yielded support for this proposal and arrangements were subsequently made to proceed. This report provides information that suggests that the experience of the HPV team in delivering smokefree ABC practice within the vaccination process has been acceptable and professionally satisfying. It also provides strong indications that students accept the smokefree ABCs as a legitimate part of the routine. Further, the description by staff of the response of some students in accepting advice and cessation support indicates that some students are not just hearing the information but are choosing to act upon it. The HPV team described the first period of activity to which this report primarily relates was intended as an opportunity to achieve ‘proof of concept’. The report provides detail suggesting that the concept has indeed been proven. In particular, this can be interpreted from the HPV team’s decision to implement a systematic recording process for documenting smokefree ABC practice. The comments provided by members of the HPV team interviewed during the course of this review also strongly support this. This report recommends the continuation and strengthening of the delivery of smokefree ABC practice within the HPV programme and recommends further evaluation of the impact of the programme on the thinking and behaviour of students. Page 3 of 23 3. Recommendations Based on the information gathered during the course of developing this report, the following recommendations are made: That smokefree ABC practice continue to be formally included as part of the HPV vaccination process That further investigation takes place to gain a closer understanding of the response of those students receiving vaccinations to smokefree screening, advice and cessation support. Specifically, to determine if and what impact these have on the thinking of the students and on their subsequent smoking behaviour That the Ministry of Health be encouraged to consider the formal inclusion in its HPV programme resources of information on the risks of smoking and the benefits of being smokefree particularly as they relate to cervical cancer That further investigation takes place to understand the factors that lie behind the recently obtained audit results indicating high levels of screening of smokefree status and substantially lower levels of the provision of brief advice and cessation support That the smokefree education provided for members of the HPV team be reviewed to ensure it effectively addresses learning needs encompassing knowledge relating to smoking and smoking cessation; to the procedures that will be followed in the HPV programme; and to ensure team members achieve confidence in the practical delivery of those requirements Page 4 of 23 4. Background 99% of all cervical cancer is caused by genital infection with human papillomavirus (HPV). HPVs are common viruses that are spread through skin to skin contact. Some types of high-risk HPV can cause cell changes in the cervix which, if not detected through cervical screening and treated, over many years can lead to cervical cancer. Other factors increase the risk of cervical cancer including genetics, smoking and number of sexual partners. The HPV Immunisation Programme is a Ministry of Health initiative which aims to protect young women from HPV infection and the risk of developing cervical cancer later in life. Currently, around 150 women are diagnosed with cervical cancer and 60 women die from it each year in New Zealand. The HPV immunisation is free for girls and young women born on or after 1 January 1990. It is available through participating schools or from family doctors, local health centres and some Family Planning clinics. Girls and young women represent an ‘at risk’ group in terms of initiation of smoking. Across New Zealand, young women from 17 years of age have the highest prevalence of smoking. 2006 Census data1 shows that over 40% of 19 year old women in the Hawke’s Bay smoke. The data further reveal high and disproportionate representation of Māori women smoking with Māori and Pacifica women also recording the greatest burden of harm from tobacco related disease and with higher rates of cervical cancer2 Each District Health Board (DHB) has been responsible for developing plans to implement the HPV Immunisation Programme and in Hawke’s Bay the DHB has established a designated team within the Public Health Nursing unit. The team has designed and is implementing a school-based vaccination programme which in 2009 was targeted at college-age girls. In 2010 the programme will target intermediate-age (Year 8) girls. During the development of the HPV team’s plans, the team was approached by the member of the HBDHB Smokefree Team responsible for Maternal, Child and Youth Services who highlighted smoking as a key factor that increases the risk of cervical cancer 1 2 Jones L. Census 2006 – Knowing our people – smoking trends. Unpublished Report. Hawke’s Bay District Health Board. The HPV (Human Papillomavirus) Vaccination Programme. National Implementation Strategic Overview. http://www.moh.govt.nz/moh.nsf/pagesmh/7893/$File/hpv-national-implementation-strategic-overview.pdf Page 5 of 23 and described the initiative underway throughout HBDHB for services to routinely address smoking with all patients. The DHB’s smokefree strategy is an evidence-based approach in which the smokefree status of every patient is identified and every patient that is not smokefree is provided brief advice as to the benefits of being smokefree and the risks of smoking and is provided support to access cessation support including provision of nicotine replacement therapy and behavioural counseling. This is often referred to as ABC practice representing: Ask - Brief advice – Cessation. The Hawke’s Bay HPV team considered this suggestion and decided that it made sense to formally incorporate ABC practice into the vaccination process. Accordingly, a protocol for implementing ABC was agreed and the practice was incorporated into the vaccination process. Most vaccinators working in the HPV team are trained Quit Card providers and were accordingly able to issue Quit Cards to any participants where that was appropriate and according to the requirements of the Quit Card programme3. This report has been prepared to document the process by which ABC practice came to be formally incorporated into the HPV vaccination programme and to gather feedback from those involved in the programme as to the perceived appropriateness of its inclusion and as to impressions of its success. 3 http://www.quit.org.nz/page/providers/QuitCards.php Page 6 of 23 5. Literature Review 5.1. HPV Human papillomavirus (HPV) is among the most common sexually transmitted infection 4 and half of all cervical cancers worldwide are attributed to HPV5. In 2006 Wiley et al6 reported on a randomized clinical trial in which they had sought to determine the association between tobacco smoking and HPV antibodies among women with HPV. Similar findings have been reported more recently by Moralejo 7. Wiley et al found that HPV-16 infected women who reported increasingly greater levels of daily cigarette smoking were less likely to test positive for anti-HPV16 antibodies that nonsmoking women. In fact, they found that women that were not smokefree were twice as likely as women that were smokefree to test negative for HPV16 antibodies even after controlling for the effects of other covariates. In their discussion, they suggested that among young women with HPV16 infection smoking cigarettes may impair the development of an HPV16-specific humoral immune response and they went on to state that the data indicated a causal relationship between smoking and cancer that may be open to behavioural interventions. Wiley et al stated that their findings supported the need for enhanced public health messages that convey yet another smoking-related health risk to women. They argued that as it may take some time to achieve population protection from HPV through vaccination and immunity, it would also be important to test smoking cessation interventions as to their impact on immune responses and subsequent long-term risk of persistent oncogenic HPV infection. Szarewski et al investigated the effect of cessation or reduction of cigarette smoking on the course of minor-grade cervical lesions and found support for a link between smoking and cervical disease suggesting that smoking cessation could have a beneficial effect on 4 5 6 7 Stone KM, Karem KL, Sternberg MR, et al. Seroprevalence of human papillomavirus type 16 infection in the United States. J Infect Dis 2002; 186: 1396-402 Munoz N. Human papillomavirus and cancer: the epidemiological evidence. J Clin Virol 2000; 19: 1-5 Wiley DJ, Wiesmeier E, Masongsong E, Gylys KH, Koutsky LA, Ferris DG, Barr E, Rao JY, and The Proof of Principle Study Investigative Group. Smokers at higher risk for undetected antibody for oncogenic human papillomavirus type 16 infection. Cancer Epidemiol Biomarkers 15 (5) May 2006. D Moralejo Smoking increased risk of cervical cancer, independent of infection with high-risk HPV types. Evid Based Nurs 2009;12:122 Page 7 of 23 early cervical abnormalities8. Bishop et al similarly found that where there is a low grade cervical abnormality, becoming smokefree can result in regression of the lesion9 5.2. Smoking Cessation The literature is replete with evidence relating to the effectiveness of interventions designed to assist a person to become smokefree. A seminal report was issued by the US Surgeon General in 200010. This highlighted, among other things, the importance of screening the smokefree status of all patients at every opportunity and providing brief advice and cessation support to those patients that are not smokefree. This approach also provides the basis of the New Zealand Smoking Cessation Guidelines 200711. These guidelines describe an ABC approach in which every patient is Asked about their smokefree status, those that are not smokefree are provided with Brief advice, and Cessation support is provided (or referred) for those wishing to access it. Since 2004, New Zealand hospitals and other health providers have been increasingly incorporating smokefree ABC into routine practice. ABC practice has become part of routine best practice across many health disciplines including doctors, nurses and midwives, and is being incorporated in other services as well. Hawke’s Bay DHB has prepared a number of reports on the effectiveness of this strategy, including preliminary investigation into the effectiveness of routine smokefree ABC in a school dental service 12 and an Audiology service13. 8 9 10 11 12 13 Szarewski A, Jarvis MJ, Sasieni P, Anderson M, Edwards R, Steele SJ, Guillebaud J, Cuzick J. Effect of smoking cessation on cervical lesion size. The Lancet 1996, Volume 347, Issue 9006, Pages 941-943 Bishop A, Marteau T, Hall S, Kitchener H, Hajek P. Increasing womens intentions to stop smoking following an abnormal cervical smear test result. Preventive Medicine 41 (2005) 179-185 Fiore MC, Bailey WC, Cohen SJ, et al Treating tobacco use and dependence. Clinical Practice Guideline. Rockville MD: US department of Health and Human Services. Public Health Services. June 2000. Ministry of Health. 2007 New Zealand Smoking Cessation Guidelines. Wellington: Ministry of Health Smith DJ. ABC in a Dental Service provided at Wairoa College, 2009. Unpublished report prepared for Hawke’s Bay DHB Totally Smokefree Project. Smith DJ. ABC by the staff at the HBDHB Audiology Department, 2009. Unpublished report prepared for Hawke’s Bay DHB Totally Smokefree Project. Page 8 of 23 6. Description of the HPV vaccination programme The Hawke’s Bay HPV vaccination programme, like other programmes throughout New Zealand, is offered in school settings. The team book to visit schools in advance with an initial group presentation, usually delivered in an assembly session, during which the Ministry of Health DVD is shown and spoken to. There is also an opportunity for questions. Students take home the consent forms for completion prior to the vaccination day. The vaccination is scheduled and usually takes place three to four weeks after the initial assembly presentation. HPV vaccinations are delivered in a 1:1 setting in which the nurse follows the vaccination protocol which includes preliminary administrative questions and administration of the vaccine itself. Vaccination usually takes place in the school hall which is set up with a waiting area and a vaccination area. The vaccination area features individual cubicle spaces with privacy screens separating those receiving vaccinations so as to ensure privacy of discussions as well as ensuring visual privacy from others. Participants assemble and wait in the waiting area then enter the cubicle spaces individually where the vaccination process takes place. Following their vaccination, participants are required to wait for twenty minutes in a ‘recovery’ area where they are monitored for any adverse reactions. After this time, and providing no adverse reactions have been observed, the participants return to class. The Hawke’s Bay programme has been modified to incorporate ABC smokefree screening and discussion as follows: during the initial assembly session, information on being smokefree and the inclusion of the smokefree (ABC) discussion within the vaccination process is discussed including the opportunity for questions and discussion smokefree ABC screening and discussion are completed during the 1:1 vaccination which takes place behind the privacy screens. Screening (A) is completed by asking the student if she is smokefree with the subsequent discussion (B&C) following on as per training provided including provision of Quit Card if appropriate Delivery of the ABC smokefree intervention during the 1:1 vaccination stage was decided after consideration by the HPV team as described in section 9.3.1 Design below Page 9 of 23 7. Key Smokefree Messages The inclusion of ABC practice within the HPV programme was fundamentally designed to bring a strong smokefree message to programme participants. The tone of the message was carefully designed to focus on the positive aspects and benefits of being smokefree, to highlight that becoming (or remaining) smokefree is important, possible and that support is readily available. The intended outcome of the messages was to inform the thinking of participants and, wherever possible, to support them in making positive changes relating to being smokefree The following key smokefree messages were identified with one key message related directly to HPV and several others related to the importance of being smokefree and support available to assist cessation efforts: HPV-specific The body is 50% more likely to resist the human papillomavirus if you are smokefree Smokefree-related Being smokefree is the single most important thing you can do for your health Effective support to be smokefree (including nicotine replacement therapy and behavioural support) is readily available Page 10 of 23 8. Education plan and resource development 8.1. Education Arising from consultation between the HBDHB Smokefree Team responsible for Maternal, Child and Youth Services, and the HPV Programme Coordinator, an Education Plan was developed to ensure members of the HPV team were sufficiently informed as to the rationale for, and the clinical protocol for delivering, ABC smokefree intervention within the HPV vaccination process. The plan was based on an understanding of the educational needs of the team members and of the need to include components relating to both knowledge and practice. That is, education which addressed both the evidence-basis for ABC intervention (including information relating to the benefits of being smokefree and the risks of smoking, the role of smoking as a risk factor in the development of cervical cancer, and the evidence supporting ABC practice as an effective intervention14) as well as education to develop the practical confidence of team members to deliver ABC practice. Education provided for the HPV team prior to the introduction of ABC smokefree practice included dedicated input: a presentation by the DHB’s Smokefree Coordinator for Maternal, Child and Youth Services designed to provide relevant background relating to smoking, and to smokefree evidence and practice together with generic education available to all DHB staff: a 20 minute, focused-discussion with a member of the smokefree team to further support understanding about smokefree practice, the Ministry of Health Performance Targets, HBDHB commitment and goals and referral systems (refer Appendix 3) team members were also required to complete the Ministry of Health’s online smokefree e-Learning module15 14 15 NZ Smoking Cessation Guidelines 2007 https://smokingcessationabc.org.nz/ Page 11 of 23 8.2. Resources Simple resources were available to support the ABC practice including posters on the privacy screens separating the vaccination cubicles, and bookmarks to be given to each girl. The concept of providing bookmarks emerged in the initial discussions with the Smokefree Project Leader who facilitated a careful design process. The bookmark is intended as a ‘take-home’ reminder of the smokefree conversation including simple relevant information and was designed to “affirm the message that being smokefree is a positive action to contribute to protection from cervical cancer”. A careful process of consultation was undertaken in designing the bookmark which included seeking feedback from 50 secondary school students who were given draft bookmarks. 27 of the 50 samples were returned with comments which were generally positive and constructive with many of the practical recommendations addressed in the final product. A copy of the bookmark is provided in Appendix 1. A further resource to the initiative was already available to the team by virtue of the fact that many members of the team were already trained Quit Card providers. Accordingly, Quit Cards were a resource available to support this initiative. Page 12 of 23 9. Staff perceptions Three members of the HPV team were interviewed to ascertain their views relating to the smokefree initiative. This included the Programme Coordinator, the wider Public Health Nursing Team’s Practice and Quality Educator and one of the Registered Nurse Vaccinators. 9.1. Importance of ABC Smokefree Practice Interviewees were unanimous in their view that ABC smokefree practice is an important consideration in the provision of health services. Comments included: important to get it (smokefree message) out there normalise ABC into practice develop comfort with practice people expect you to ask there is evidence of the effect I believe in the model of brief intervention posters (eg It’s Cool to be Smokefree) provide support smokers ostracised nowadays a good change 9.2. Legitimacy of ABC Smokefree Practice Interviewees were even more united in their opinion that ABC practice is a legitimate and important part of the HPV programme. Comments included: its even more important the body is 50% less likely to resist the virus if the person is smoking the direct link with our issue (HPV) makes it important The general health benefit in being smokefree was well recognised within the group with ABC smokefree practice acknowledged as a legitimate activity for health professionals. The linkage between being smokefree and better outcomes in relation to HPV was a strong feature of the discussion and appeared to be a key consideration in the team’s decision to implement ABC smokefree practice as a formal and systematic component of the vaccination process. Page 13 of 23 9.3. Clarity of Process Expectations 9.3.1. Design Interviewees were clear as to the requirements of the ABC process. This was particularly so following the extent of involvement of the team in determining how the ABC would be incorporated into the vaccination process. Indeed the team was instrumental in revising the originally proposed process in which the ABC conversation was to occur during the 20 minute ‘recovery’ period following the administration of the vaccination. The team determined that it would be more effective to complete the ABC process during the 1:1 process of vaccine administration. The rationale for this was based on the team’s experience in providing vaccinations in school hall settings involving large groups of teenage students. The experience of the team was that as the students assemble in the common area, and during the 20 minute post-vaccination observation period where the students are once again assembled in the common waiting area, there is a high level of social interaction among the students. The team characterised these conversations as often being animated as a function of the unusual process, the involvement of needles, etc. Indeed, the team reported that often the students would exhibit considerable bravado in the face of the process. This was seen as being un-conducive to the ABC conversation and accordingly, the team agreed that the ABC conversation take place during the period of time in which the students are taken individually into privacyprotected spaces for the vaccination. The team’s experience was that during this time, the students were generally calm, focused and open to the ‘serious-business’ at hand. The team felt this would be a much more effective opportunity to engage in the brief smokefree intervention. Comments relating to the decision to incorporate smokefree intervention with the 1:1 phase of the vaccination process included: it’s a comfortable setting it feels intimate it takes the ‘sniggering’ away it eliminates ‘group behaviour’ the girls have trust in the vaccination process Page 14 of 23 it is a time to be professional and serious it is a safe environment there is a relationship between the girl and the vaccinator 9.3.2. System/Process Interviewees reported they, and other members of the HPV team, were clear as to the requirements of ABC smokefree practice. They felt the process was intuitively simple, and that it aligned closely with the intent and purpose of the HPV programme in promoting optimal health. A simple recording process was agreed and has since been reviewed with the team determining that a recording sticker will be affixed to each student’s notes. This has been decided so as to simplify the process requirements of recording and of any subsequent audit. 9.4. Education As described above Education provided to the HPV team prior to the introduction of ABC smokefree practice included a presentation by the DHB’s Smokefree Project Leader for women’s health services designed to provide relevant background relating to smoking, and to smokefree evidence and practice. Following this team members were required to complete the Ministry of Health’s online e-Learning module16. Interviewees reported that the education provided was entirely adequate and appropriate. Comments included: Smokefree coordinator’s support was great the initial team session was a great opportunity for team input and ideas education was definitely adequate there was strong evidence It was noted by those interviewed that some ‘reminder’ education would be useful especially in the lead up to the next season of vaccinations. This was considered useful both in terms of reminding of the ABC approach and also so as to ensure 16 https://smokingcessationabc.org.nz/ Page 15 of 23 continued clarity of process for all team members particularly in light of the proposed revised recording requirements. 9.5. Resources As described above, simple resources were available to support the ABC practice including posters on the privacy screens separating the vaccination cubicles and bookmarks to be given to each girl. Interviewees were generally pleased that simple resources were available to support practice. Comments included: they are tangible they are provided free it’s a good design they include good information 80% of the girls take them home they are positive The vaccination programme includes a Ministry of Health DVD17 which is shown to groups of students during education sessions held between two and four weeks prior to the vaccinations being given. Interviewees expressed concern that the information provided in the DVD does not adequately address issues relating to the risks of smoking and the benefits of being smokefree and felt that inclusion of this in any revision of the DVD would support their efforts. 9.6. Roles The team felt they were clear as to the various roles. In particular there is a high level of clarity as to the requirements of nurse vaccinators. In addition the team leader was clear as to her responsibility for supporting the initiative in terms of facilitating educational opportunities for the team, enabling the team to participate in the planning process, and in ensuring documentation and other systems were in place. 17 Cervical cancer vaccine – DVD presentation for girls and young women about the HPV Immunisation Programme. Ministry of Health, Wellington, 2008 Page 16 of 23 10. Client Perceptions This current review process did not provide for direct feedback from participants in the HPV programme. Perceptions of participants, as observed by members of the HPV team, were reported during the team interview. There was close agreement between the three team members interviewed as to their observations of participant response and experience. Comments about the response and experience of the participants included: the girls listen the girls are receptive to the information they are not faking it! they often ask questions there has been no negative or abusive reaction the girls don’t feel alienated by the discussion the girls seem to expect the discussion having it incorporated in the recording form helps make ABC practice more acceptable, the girls know is universal and not a judgment of them in particular A further demonstration of the receptiveness of the participants to the ABC discussion is that a substantial number of Quit Cards are being provided to participants. Details relating to the number of Quit Cards issued are not available, however, analysis of this would be a useful component of any subsequent review. Page 17 of 23 11. Preliminary Audit – April 2010 11.1. Results A preliminary audit of ABC smokefree practice has been undertaken by the HPV team during April 2010. This follows the introduction of the recording sticker (refer Appendix 2) which is affixed to every student’s record and provides for a simple, tick-box recording of smokefree status and the provision of brief advice and cessation support. Data from the preliminary audit are as follows: 1175 student records were reviewed Smokefree status recorded as screened for 1007 of the 1175 (86%) Of the 1007 students whose smokefree status had been screened, 741 were recorded as being smokefree (74%) and 266 were recorded as not being smokefree (26%) Of the 266 students that were not smokefree, 50 were recorded as having received brief advice (19%) and 21 received further support (8%) 11.2. Comments The percentage of students whose smokefree status was recorded is relatively high at 86% suggesting this aspect of the process has been readily adopted by vaccinators. The percentage of students recorded as not smokefree is approximately the same as that reveled in the 2006 census data which showed the prevalence of smoking among 17 year old girls at just over 25%. It is unclear what the age composition of the audit sample was and this would be important information to confirm as if significantly more younger students were involved this would indicate a higher prevalence that that shown in the Hawke’s Bay 2006 census statistics1 (which showed smoking prevalence among 15 year old girls at 12% and among 16 year old girls at 17%). Page 18 of 23 The percentage of those students that were recorded as receiving brief advice was relatively low at 19%. It is unclear from the preliminary audit what factors lie behind this result. It could be that brief advice was not provided in many instances and, alternatively, it could be that brief advice has indeed been offered during the vaccination process but that this has not been consistently recorded. Further investigation is warranted into this aspect in order to identify how best to address the issue which could involve further training in recording or further training in delivering brief advice. It could also be that certain features of the vaccination process are impacting on performance and it would be important to consider these as well. The percentage of students that were recorded as receiving cessation support was also relatively low at 8%. As with screening, further investigation is warranted to determine the reasons for this. Notwithstanding the relatively low percentage, it is noteworthy that in the sample of students that were included in this audit, 26 received further support to become smokefree beyond the provision of simple brief advice. It is not clear what the nature of this support was however it is likely to have ranged from more intensive (motivational) conversations through to the provision of NRT via a Quit Card and referral for cessation support. That 26 young students have received this kind of advice is excellent and demonstrates that the opportunity afforded by the HPV vaccination process can effectively be used to reinforce and support students to become smokefree. As above, further investigation would be useful to better understand the nature of the cessation support provided. It would also be valuable to undertake a follow up investigation to determine the subsequent impact of that cessation support. Indeed an outcome-focused follow up would be highly valuable to determine if the screening and brief advice has had any impact on the thinking of students and if the cessation support provided has led to any changes in smoking behaviour. Page 19 of 23 12. Appendices 12.1. APPENDIX 1 - Bookmark Resource Page 20 of 23 12.2. APPENDIX 2 - Recording Sticker Page 21 of 23 12.3. APPENDIX 3 - Session Outline – 20 minute presentation 20 Minute Introduction For Registered Health Professionals 1. Introduction a. Introduce the training package, discuss outcomes, intro + E-Learning Tool b. MOH National Health Targets c. Duty of care / best practice d. On completion of the entire training you will be able to provide NRT via the standing order in hospital or a quit card upon discharge 2. Smokefree language a. Non-judgemental language reduces resistance 3. NRT Products (Refer to “Quick Reference Card”) Long-acting - Patch Short-acting – Gum / lozenge / inhaler Inhaler is the only of these products not subsidised and ideally used as a short acting product when patient NBM – important to explain to the patient that this will not be subsidised on discharge. Contraindications - NBM (gum or lozenge) - Allergy to sticking plaster (patch) Cautions - Pregnancy/breastfeeding - Within 2 weeks post severe cardiovascular event/stroke - Patients admitted into ICU (NRT use in ICU patients is an Anaesthetist’s decision) - Theatre – patch needs to be removed for during theatre 4. How to assess nicotine dependency (Refer to “NRT Flowchart”) 5. NRT Standing Order (Resource: HBDHB NRT Standing Order) Pre-requisite is E-Learning Tool Nicotine patch/gum/lozenge/inhaler Documented on medication chart - Medication Name / Date / Dose / Frequency of administration / Reference to NRT Standing Order / Name & signature of RN Must be countersigned within 24 hours All patients receiving NRT require Nicotine withdrawal symptoms assessed twice daily (BD) 6. Assessing Nicotine Withdrawal (Resource: “Assessing Nicotine Withdrawal Laminated ID Card”) Assessed twice daily for all patients receiving NRT Use scale of 0 – 5 Increase dose or frequency of NRT when patient scores 2 or more Document score in Patient Flowchart under Treatment and Observations Page 22 of 23 7. Refer for Smokefree Support (Resource: “Hospital Based Smokefree Service Pamphlet”) Refer to Hospital Based Smokefree Service ext 2472 for ongoing support to become smokefree. Leave Name, NHI number and a brief message. 8. Where to from here - How to access E-Learning Tool - When completed, fax certificate through to L&D ext 2216 (required so that L&D can update history) 9. Additional information for speciality areas Doctors; - offer brief advice (robust research backing this) - sign off on standing orders - importance of discharge summary relating to smokefree status / NRT commenced (eg drug interactions) Maternity and Paediatrics…. Brief advice on becoming smokefree at any stage of wellness is a powerful motivator and a necessary part of clinical practice. Page 23 of 23