References - European Heart Journal
advertisement

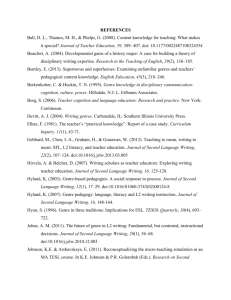
CP 3618 References are available as supplementary material at European Heart Journal online Title: Antenatal assessment of cardiac defects in the foetus References: 1 Mensah GA. An overview of cardiovascular disease burden in the United States. Heath Affairs 2007;26:38-48. 2 Trends in infant mortality attributable to birth defects – United States, 1980 – 1995. MMWR 1998;47:773-778 3 Haak MC. Echocardiography in early pregnancy: Review of the literature. Journal of ultrasound in medicine 2003;223:271-280 . 4 Khalil A, Nicolaides KH. Foetal heart defects: potential and pitfalls of first trimester detection. Seminars in Foetal and Neonatal Medicine 2013;18:251-260. 5 Respondek M, 2D echocardiographic assessment of the foetal heart size in the 2nd and 3rd trimester of uncomplicated pregnancy. Eur J Obstet Gynecol Reprod Biol 1992;13:185-188 6 Kirk S Foetal cardiac asymmetry. A marker for congenital heart disease obstetrics and gynecology 1999; 93;189-192 7 Salvo DN Clinical significance of isolated foetal pericardial effusion. Journal of ultrasound in medicine 1994;13;291-293 8 Ayres N. 1997. Advances in foetal echocardiography. Texas Heart Institute Journal. 1997;4:250-259. 9 Devore G, Trisomy 21:91% detection rate using second-trimester ultrasound markers ultrasound journal of obstetrics and gynecology 2000;16;133-141 10 Hornberger LK Echocardiographic study of the morephology and growth of the aortic arch in the human foetus. Circulation 1992 86:741 Title: Assessing foetal cardiac anomalies using Echocardiography REFERENCES 1 Synqelaki A, Challenges in the diagnosis of foetal non-chromosomal abnormalities at 11-13 weeks, Prenatal diagnosis 2011;31;90-120 2 Faiola S Likelihood ratio for trisomy 21 in foetuses with tricuspid regurgitation at the 1113+6 week scan. Ultrasound Obstetric Gynaecology 2005 Jul 26 (1) 22-27 3 Nicholaides K Screening for foetal aneuploidies at 11-13 weeks Prenatal Diagnosis 2011;31;7-15 4 Nicholaides K Turning the pyramid of care Foetal Diagnosis and therapy 2011;29;183-196 5 Devore G, Trisomy 21:91% detection rate using second-trimester ultrasound markers ultrasound journal of obstetrics and gynecology 2000;16;133-141 6 Ayres N Advances in foetal echocardiography Pediatric cardiology 1997;24;250-259 7 Frid C Mortality in Down’s syndrome in relation to congenital malformations J intellect Disabil Res 1999;43; 234-241 8 Renna MD Sonographic markers for early diagnosis of foetal malformations. World Journal of radiology 2013 5(10) 356-371. 9 Khalil A Foetal heart defects: Potential and pitfalls of first trimester detection Seminars in Foetal and Neoantal Medicine 2013;18;251-260 Title: Pregnancy hormones in cardiovascular disease References: 1. Regitz-Zagrosek V, Blomstrom Lundqvist C, Borghi C, Cifkova R, Ferreira R, Foidart JM, Gibbs JS, Gohlke-Baerwolf C, Gorenek B, Iung B, Kirby M, Maas AH, Morais J, Nihoyannopoulos P, Pieper PG, Presbitero P, Roos-Hesselink JW, Schaufelberger M, Seeland U, Torracca L. ESC Guidelines on the management of cardiovascular diseases during pregnancy: the Task Force on the Management of Cardiovascular Diseases during Pregnancy of the European Society of Cardiology (ESC). Eur Heart J 2011; 32(24):3147-3197. 2. Mannisto T, Mendola P, Vaarasmaki M, Jarvelin MR, Hartikainen AL, Pouta A, Suvanto E. Elevated blood pressure in pregnancy and subsequent chronic disease risk. Circulation 2013; 127(6):681-690. 3. Powe CE, Levine RJ, Karumanchi SA. Preeclampsia, a disease of the maternal endothelium: the role of antiangiogenic factors and implications for later cardiovascular disease. Circulation 2011; 123(24):2856-2869. 4. Hilfiker-Kleiner D, Kaminski K, Podewski E, Bonda T, Schaefer A, Sliwa K, Forster O, Quint A, Landmesser U, Doerries C, Luchtefeld M, Poli V, Schneider MD, Balligand JL, Desjardins F, Ansari A, Struman I, Nguyen NQ, Zschemisch NH, Klein G, Heusch G, Schulz R, Hilfiker A, Drexler H. A cathepsin D-cleaved 16 kDa form of prolactin mediates postpartum cardiomyopathy. Cell 2007; 128(3):589-600. 5. Albrecht ED, Pepe GJ. Placental steroid hormone biosynthesis in primate pregnancy. Endocr Rev 1990; 11(1):124-150. 6. Jobe SO, Tyler CT, Magness RR. Aberrant synthesis, metabolism, and plasma accumulation of circulating estrogens and estrogen metabolites in preeclampsia implications for vascular dysfunction. Hypertension 2013; 61(2):480-487. 7. Barbagallo M, Dominguez LJ, Licata G, Shan J, Bing L, Karpinski E, Pang PK, Resnick LM. Vascular Effects of Progesterone : Role of Cellular Calcium Regulation. Hypertension 2001; 37(1):142-147. 8. Zeisler H, Sator MO, Joura EA. Serum levels of progesterone in patients with preeclampsia. Wien Klin Wochenschr 2000; 112(8):362-364. 9. Szlachter BN, Quagliarello J, Jewelewicz R, Osathanondh R, Spellacy WN, Weiss G. Relaxin in normal and pathogenic pregnancies. Obstet Gynecol 1982; 59(2):167-170. 10. Halls ML, Bond CP, Sudo S, Kumagai J, Ferraro T, Layfield S, Bathgate RA, Summers RJ. Multiple binding sites revealed by interaction of relaxin family peptides with native and chimeric relaxin family peptide receptors 1 and 2 (LGR7 and LGR8). J Pharmacol Exp Ther 2005; 313(2):677-687. 11. Conrad KP. Emerging role of relaxin in the maternal adaptations to normal pregnancy: implications for preeclampsia. Semin Nephrol 2011; 31(1):15-32. 12. Patten IS, Rana S, Shahul S, Rowe GC, Jang C, Liu L, Hacker MR, Rhee JS, Mitchell J, Mahmood F, Hess P, Farrell C, Koulisis N, Khankin EV, Burke SD, Tudorache I, Bauersachs J, del Monte F, Hilfiker-Kleiner D, Karumanchi SA, Arany Z. Cardiac angiogenic imbalance leads to peripartum cardiomyopathy. Nature; 485(7398):333-338. 13. Sliwa K, Blauwet L, Tibazarwa K, Libhaber E, Smedema JP, Becker A, McMurray J, Yamac H, Labidi S, Struman I, Hilfiker-Kleiner D. Evaluation of bromocriptine in the treatment of acute severe peripartum cardiomyopathy: a proof-of-concept pilot study. Circulation 2010; 121(13):1465-1473. 14. Halkein J, Tabruyn SP, Ricke-Hoch M, Haghikia A, Nguyen NQ, Scherr M, Castermans K, Malvaux L, Lambert V, Thiry M, Sliwa K, Noel A, Martial JA, HilfikerKleiner D, Struman I. MicroRNA-146a is a therapeutic target and biomarker for peripartum cardiomyopathy. J Clin Invest 2013; 123(5):2143-2154. Title: Marfan-syndrome and pregnancy: Monitoring and management References 1. European Society of Gynaecology (ESG); Association for European Paediatric Cardiology (AEPC); German Society for Gender Medicine (DGesGM), Regitz-Zagrosek V, Blomstrom Lundqvist C, Borghi C, Cifkova R, Ferreira R, Foidart JM, Gibbs JS, Gohlke-Baerwolf C, Gorenek B, Iung B, Kirby M, Maas AH, Morais J, Nihoyannopoulos, P, Pieper PG, Presbitero P, Roos-Hesselink JW, Schaufelberger M, Seeland U,Torracca L; ESC Committee for Practice Guidelines. ESC Guidelines on the management of cardiovascular diseases during pregnancy: the Task Force on the Management of Cardiovascular Diseases during Pregnancy of the European Society of Cardiology (ESC). Eur Heart J. 2011 Dec;32(24):3147-97. doi: 10.1093/eurheartj/ehr218. Epub 2011 Aug 26. PubMed PMID: 21873418. 2.Giannubilo SR, Cecchi S, Tidu E, Ciavattini A. Maternal NT-proBNP in chronic hypertensive pregnancies and superimposed preeclampsia. Int J Cardiol. 2014 Oct 20;176(3):1227-9. doi: 10.1016/j.ijcard.2014.07.214. Epub 2014 Aug 5. PubMed PMID: 25115250. 3.Hassan N, Patenaude V, Oddy L, Abenhaim HA. Pregnancy Outcomes in Marfan Syndrome: A Retrospective Cohort Study. Am J Perinatol. 2014 Jun 4. [Epub aheadof print] PubMed PMID: 24896139. 4. Ruys TP, Roos-Hesselink JW, Hall R, Subirana-Domènech MT, Grando-Ting J,Estensen M, Crepaz R, Fesslova V, Gurvitz M, De Backer J, Johnson MR, Pieper PG. Heart failure in pregnant women with cardiac disease: data from the ROPAC. Heart.2014 Feb;100(3):231-8. doi: 10.1136/heartjnl-2013-304888. Epub 2013 Nov 29. 5.Tutarel O, Lotz J, Roentgen P, Drexler H, Meyer GP, Westhoff-Bleck M.Pregnancy in a Marfan patient with pre-existing aortic dissection. Int J Cardiol.2007 Jan 8;114(2):E36-7. Epub 2006 Oct 24. PubMed PMID: 17067692. 6.Westhoff-Bleck M, Podewski E, Hilfiker A, Hilfiker-Kleiner D. Cardiovascular disorders in pregnancy: diagnosis and management. Best Pract Res Clin ObstetGynaecol. 2013 Dec;27(6):821-34. doi: 10.1016/j.bpobgyn.2013.07.001. Epub 2013Aug 8. Review. PubMed PMID: 23932772. Title: Underestimated risk for life-threatening ventricular arrhythmias in newly diagnosed peripartum cardiomyopathy? References 1. Sliwa K, Hilfiker-Kleiner D, Petrie MC, et al. Current state of knowledge on aetiology, diagnosis, management, and therapy of peripartum cardiomyopathy: a position statement from the Heart Failure Association of the European Society of Cardiology Working Group on peripartum cardiomyopathy. Eur J Heart Fail. 2010;12(8):767– 778. doi:10.1093/eurjhf/hfq120. 2. Chee K-H. Favourable outcome after peripartum cardiomyopathy: a ten-year study on peripartum cardiomyopathy in a university hospital. Singapore Med J. 2013;54(1):28– 31. 3. Blauwet LA, Libhaber E, Forster O, et al. Predictors of outcome in 176 South African patients with peripartum cardiomyopathy. Heart. 2013;99(5):308–313. doi:10.1136/heartjnl-2012-302760. 4. Goldberger JJ, Cain ME, Hohnloser SH, et al. American Heart Association/American College of Cardiology Foundation/Heart Rhythm Society Scientific Statement on Noninvasive Risk Stratification Techniques for Identifying Patients at Risk for Sudden Cardiac Death. Heart Rhythm. 2008;5(10):e1–e21. doi:10.1016/j.hrthm.2008.05.031. 5. Zipes DP, Camm AJ, Borggrefe M, et al. ACC/AHA/ESC 2006 Guidelines for Management of Patients With Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death: A Report of the American College of Cardiology/American Heart Association Task Force and the European Society of Cardiology Committee for Practice Guidelines (Writing Committee to Develop Guidelines for Management of Patients With Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death): Developed in Collaboration With the European Heart Rhythm Association and the Heart Rhythm Society. Circulation. 2006;114(10):e385–e484. doi:10.1161/CIRCULATIONAHA.106.178233. 6. Klein HU, Meltendorf U, Reek S, et al. Bridging a Temporary High Risk of Sudden Arrhythmic Death. Experience with the Wearable Cardioverter Defibrillator (WCD). Pacing and Clinical Electrophysiology. 2010;33(3):353–367. doi:10.1111/j.15408159.2009.02590.x. 7. Saltzberg MT, Szymkiewicz S, Bianco NR. Characteristics and outcomes of peripartum versus nonperipartum cardiomyopathy in women using a wearable cardiac defibrillator. Journal of Cardiac Failure. 2012;18(1):21–27. doi:10.1016/j.cardfail.2011.09.004. 8. Goland S, Modi K, Bitar F, et al. Clinical profile and predictors of complications in peripartum cardiomyopathy. Journal of Cardiac Failure. 2009;15(8):645–650. doi:10.1016/j.cardfail.2009.03.008. 9. Sliwa K, Forster O, Tibazarwa K, et al. Long-term outcome of peripartum cardiomyopathy in a population with high seropositivity for human immunodeficiency virus. International Journal of Cardiology. 2011;147(2):202–208. doi:10.1016/j.ijcard.2009.08.022. 10. Whitehead SJ, Berg CJ, Chang J. Pregnancy-related mortality due to cardiomyopathy: United States, 1991-1997. Obstet Gynecol. 2003;102(6):1326–1331. doi:10.1016/j.obstetgynecol.2003.08.009. 11. Forster O, Hilfiker-Kleiner D, Ansari AA, et al. Reversal of IFN-gamma, oxLDL and prolactin serum levels correlate with clinical improvement in patients with peripartum cardiomyopathy. Eur J Heart Fail. 2008;10(9):861–868. doi:10.1016/j.ejheart.2008.07.005. 12. Duncker D, Haghikia A, König T, et al. Risk for ventricular fibrillation in peripartum cardiomyopathy with severely reduced left ventricular function—value of the wearable cardioverter/defibrillator. Eur J Heart Fail. 2014: in press.