Zager_-_Febrile
advertisement

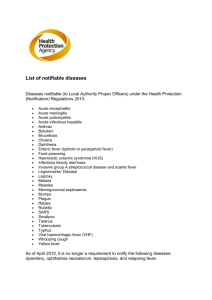
Zager – Febrile Stuff Case 1 • You are volunteering in the tent for Grandma’s Marathon and the first wave of runners are finishing. The first patient of the day is a 27 year old male (5th place finisher) who is ashen, mumbling, and stumbles in supported by two friends. His vital signs are taken. Pulse= 168, RR= 42, pulse ox= 85%, BP= 85/ 54, Temp=107.2 degrees. • Hyperthermia Case 2 • You are working in the emergency room and go on to see the next patient- a 20 month old female with three days of elevated temps at home. Parents measured a temperature of 104.6 degrees and have brought her in at 11 PM. She has no URI symptoms, no rash, but has had some vomiting today. Her vital signs are taken. Pulse= 168, RR= 42, pulse ox= 98%, BP= 85/54, Temp= 105.4 degrees. • Physiologic Physiologic Responses to Increase Body Temperature (Heat Production/ Reduce Loss): • Peripheral vasoconstriction • Shivering • Behavioral (seeking clothing, blankets, Warmth) • (Accompanied by tachycardia and tachypnea) Physiologic Responses to Reduce Body Temperature (Heat Loss) • Sweating • Peripheral vasodilation To treat (fever)….or not to treat….that is the question • Many parents believe that fever is injurious. Physiological fever doesn’t really do harm. Physicians May Suffer From the Same Contextual Problems As Parents: • May and Bauchner ((1992) performed a survey of Pediatricians and found: - 65% believed that fever alone could cause bodily injury - 60% cited a temperature above 40 degrees (C) as a critical point - 21% listed brain damage as the most serious complication of fever - 26% listed death as the most serious complication Reasons Not to Treat Fever: • Fever enhances immune function • Fever is physiologic • Limited research suggests that it may shorten duration of illness Reasons to Treat Fever: • Comfort • ??? Metabolic preservation in certain chronic disease (i.e., cardiac) Effective Treatments for Fever Reduction: • Acetaminophen (15 mg/kg/dose q 4 hours up to standard adult dosage) • Ibuprofen (10 mg/kg/dose q 6 hours up to standard adult dosage) • Aspirin (not recommended under age 16) – Reye’s Syndrome Risk. Ineffective Treatments for Fever Reduction: • Sponging • Bathing • Electric fans • Alternating acetaminophen/ ibuprofen (no more effective than one agent) Causes of Fever: • Infectious: viral, bacterial, fungal, and parasitic • Inflammatory: Kawasaki Syndrome, Juvenile Rheumatoid Arthritis • Cancer: Acute Lymphocytic Leukemia • Pharmacologic: Aspirin overdose • (fictitious) Considerations in Evaluating Febrile Children • Pattern of fever reported by parents (reliable?) • Age of Child (newborn to age 3 months more at risk) • Risk factors by age, chronic disease, immunization status, travel, etc. • • Known patterns of disease entities- i.e., Kawasaki Syndrome Exam findings: vital signs, “sick appearance”, focal abnormalities Occult Bacteremia: Bacteria Recovered From Blood of Nonseptic Individual • More common in children under 3 than older ages • Generally: pneumococcus, Hemophilus, meningococcus • Vaccines licensed for all three typical bacterial pathogens (above) • Less than 3% of febrile children under age 3 with temp > 103 Urinary Tract Infection Is More Common Than Bacteremia • Equal male : female ratio under age 6 months • Caucasian female under age 3 years with T> 39 degrees= 16% UTI • UTI in uncircumcised : circumcised male (under age 1)= 10:1 • Diagnosis by culture of urine Interpretation of CBC: • WBC> 15K predicts bacteremia with 80% sensitivity, 69% specificity, and positive predictive value of 6% • WBC< 5K with ANC < 1500 is worrisome • ANC > 10K gives sensitivity of 76%, specificity of 78% and positive predictive value of 8% • Thrombocytopenia is exceptionally worrisome development • Thrombocytosis is a frequent consequence of inflammation after 10- 21 days • Total Band Count: ANC > 0.16 highly predictive of neonatal sepsis ESR and CRP: • CRP> 4.0 suggest increased chance of bacterial disease • CRP> 10 have been associated with 85% chance of bacterial infection • ESR is an indirect measure of plasma acute phase reactants • ESR can be affected by fibrinogen, RBC morphology, sex • ESR fluctuates at a slower pace than CRP Fever Under the Age of 30 Days: • one study of 254 neonates presenting to an urban ER with temp >38 (C) identified 32 infants with serious bacterial illness (SBI) • No screening protocols for identifying young infants at “low risk” have been validated. • Evaluation must be individualized and strong consideration must be given to “full sepsis work up”- CXR, blood culture, urine culture, CSF studies and empiric antibiotics Fever From 30- 90 Days of Age (Am. Coll. Of ER Physicians): • Full exam (are they “well appearing”?) • Screening CBC • CXR in children with respiratory symptoms • Screen all infants for UTI (UA and urine culture) • Infants who have positive screening receive blood culture, CSF studies, and empiric antibiotics. Fever From 3 – 36 Months of Age - Nigrovic, Et Al, (Clinical Pediatric Emergency Medicine- March 2004) • Pre- 1987 causes of bacteremia- Hemophilus and Pneumococcus • Hib vaccination eliminated Hemophilus (1987) • • • • Pneumococcal vaccination (Prevnar) is about 85-93% effective at prevention of invasive pneumococcal disease Febrile children- 2.5% rate of pneumococcal bacteremia (80% spontaneous resolution?) 1998 to 2001 surveillance- 69% drop in invasive pneumococcal disease “Well-appearing”, febrile child > 6 mos + hx 3 doses Prevnar= no screening CBC, blood culture at Boston Children’s Hospital Febrile Seizures • Occur in about 4% of children • 6 mos of age to 6 years • Associated with temp > 38 degrees • Absence of CNS infection/ inflammation • Absence of systemic metabolic disturbance • Absent hx of prior afebrile seizure Febrile Seizure Classification: • Simple: duration less than 15 minutes, nonfocal (>90%) • Complex: longer than 15 minutes, may have focal component, post ictal paresis Etiology of Febrile Seizures: • Genetic susceptibility: several chromosomal loci have been identified in various extended families • Siblings and parents of children with febrile seizures show 4-10% rate of epilepsy • 10-20% of parents/ siblings will have a hx of febrile seizures • MRI studies suggest hippocampal abnormality may have role Differential Dx • Involuntary myoclonic release movements • Shivering • Metabolic disorder • Bacterial meningitis • Viral encephalitis Diagnostic Evaluation: • Conflicted opinion regarding necessity of examining CSF in children < 12 mos • Consider LP in questions of meningitis or if seizure occurs after first day of fever • Routine metabolic studies rarely yield etiology • Neuroimaging and EEG should be considered in “complex” variety Treatment of Febrile Seizures: • Supportive care • If duration exceeds five minutes consider emergent anticonvulsant Tx (IV lorazepam @ 0.05 to 0.1 mg/ kg) • IV fosphenytoin (15-20 mg/ kg) can be used if refractory • Diazepam rectal gel (0.5 mg/kg) if IV access unavailable • Fever reduction is unlikely to be accomplished by “external” means (sponging, bathing)- best to use acetaminophen or ibuprofen Recurrent Febrile Seizure Treatment • Home use of rectal Diazepam gel can be used by parents if seizure is longer than 5 minutes • Focal seizures are more likely to be prolonged Prevention of Febrile Seizures • AAP does not recommend intermittent or continuous anticonvulsant use • Evidence supporting aggressive antipyretic use likewise has no evidence Prognosis for Febrile Seizures • Recurrence rate is 50-65% if first seizure occurs below age 12 months • Recurrence rate is 20% in older children • Majority of recurrences are within one year of the first seizure • No evidence for developmental, neurologic, cognitive sequelae • “Normal child” with simple febrile seizure= “slightly” increased risk epilepsy • Risk factors for later epilepsy= focal sz, prolonged sz, multiple sz< 24 hrs Next to Last Word • 30% of office visits to Pediatricians have fever as the primary concern. More than 50% of afterhours phone calls involve fever concerns. Fever is a significant factor in primary care of children. • Fever is not a diagnosis (though, there is an ICD9 code for it) but rather a sign of an underlying disorder. Fever by itself is not harmful and there is increasing recognition of its role in enhanced body response to infection. Last Word • Fever as the sole manifestation of serious illness is unusual. Urinary tract infection is the most common of these obscure etiologies- generally in the preverbal child (under age 3). Hence, of all potential lab studies in the hunt for isolated fever, a UA is more productive than a CBC. • Febrile seizures are not rare. All parents will go into “panic mode” in the face of this dramatic event. The health professional’s role is first to assess and treat the needs of the child- and, second, to interpret this event for the parents. Pediatric Pharmacology Disclaimer: Pediatric Pharmacology is a diverse and involved subspecialty This presenter is not a pharmacist Pediatric Rx Principles Children are not merely “small” adults Weight-based dosage calculations are commonly used Developmental physiology may affect dosages for various drugs Breast fed infants indirectly receive their mother’s medications Most meds were tested in adult studies There’s a lot we don’t know! The Neonate Example Renal blood flow increases 10-fold in the first year of life Premie GFR= 0.8 ml/min Term infant GFR= 6-20 ml/min “Adult” GFR is achieved around 6 mos (“Adult” GFR is > 100 ml/min) Drug dosing variables Other drug competing for enzymes? Other drug displacing from protein binding (i.e., albumin)- bioavailability Renal clearance varies by hydration and maturation And on… and on… and on…. Breast feeding Categories Compatible Use with caution Unknown with concern Contraindicated Safety not established Pregnancy Categories Adequate studies have not shown risk Animal studies have not shown risk Animal studies have shown risk but human studies do not Animal studies show risk- no human studies available Human risk has been shown but potential benefits may warrant use Risk is shown and outweighs any benefit Summary: Dosage by weight is commonly employed Developmental physiology counts Pregnancy, lactation meds affect infants Databases should be consulted routinely Pediatric Respiratory Distress Pediatric Respiratory System A. Developmental Aspects B. Respiratory parameters by age C. Recognition of Respiratory Distress D. Causes of Respiratory Distress in Pediatrics E. Investigation of Pediatric Respiratory Distress F. Treatment of Respiratory Distress Case Management Examples • Case 1: 20 month old male with fever, stridor • Case 2: 20 month old female with fever, stridor • Case 3: 5 year old male with URI and sudden shortness of breath/ fever • Case 4: 5 year old female with URI and shortness of breath/no fever • Case 5: 5 week old with ER presentation of shortness of breath Pediatric Respiratory System • The younger the child the smaller the trachea is relative to body size • “Stenting” cartilage rings in trachea stiffen over the first 12 months • The lung will grow 15 fold from birth to adulthood • The “bony bellows” of the ribs are pliable (cartilage) at young ages • The abdominal muscles are the “accessory” muscles of respiration in toddlers • Infants are obligate nose breathers • Pediatric cardiac arrests are almost always precipitated by respiratory arrest Respiratory Parameters • Newborn respiratory rate is 40 breaths per minute (+/-) • Adolescent respiratory rate is 12-15 breaths per minute • Tidal volume x respiratory rate= minute ventilation • Minute ventilation requirements vary by energy needs • Various disorders will affect tidal volume Recognition of Respiratory Distress • Inspection (i.E. Color, work of breathing) • CNS status • Vital signs • Anticipation of deterioration Causes of Pediatric Respiratory Distress • Airway obstruction (large vs. Small airway) • Alveolar disease • CNS disorder • Cardiovascular collapse • Metabolic changes (acidosis, fever) • Muscle drive disorder (abdominal distension) Investigation of Pediatric Respiratory Distress • History • Examination (including vital signs) • Oximetry • Pulmonary function testing • Imaging • Blood gases Treatment of Respiratory Distress • First reach for Oxygen • treat the underlying cause • support work of breathing with technology required/available Case 1 • A 20 month old male is brought to the emergency room with fever to 104 degrees onset today. He has not had URI symptoms, but is having difficult breathing (retractions, nasal flaring) with a “muffled, thickened” quality to his respirations. He appears very anxious and is drooling. It is influenza season and you query the parents about whether he had influenza vaccination- their response is that they do not believe in vaccination. What approach is called for? Epiglottitis • Etiology: Hemophilus influenza type B • DX by inspection of epiglottis in controlled situation (Operating Room) • (Lateral neck soft tissue Xrays often challenging to interpret) • Cultures of blood and epiglottis • Treatment by intubation, airway management, antimicrobials • Prevention: Hemophilus vaccination has virtually eliminated epiglottitis • Outcome: generally fatal if no intervention, otherwise almost certain recovery Case 2 • A 20 month old female comes to the Emergency Room with URI symptoms and fever to 104 degrees. She has had a hoarse voice and a”seal bark” quality to her cough. The parents noted that she seemed much better while they were driving in to the ER- but it worsened again here. She has intercostal retractions, though, does not appear anxious. Her older brother (age 8) had had a URI and sore throat a few days ago. Croup • Etiology: usually parainfluenza virus • Mechanism: edema of glottic/ subglottic trachea • (Parainfluenza may also cause interstitial pneumonitis) • DX: clinical picture • CXR may show “steeple sign” of subglottic region • Treatment: expectant management, Dexamethasone may help more significant subglottic edema • Course usually 5-7 days Case 3 • This 5 year old male is brought to the office with onset of fever and shortness of breath today. He had been experiencing a “typical” URI for the last 4 days. His temp is 102.5 degrees and he has pale color with mild intercostal retractions. Oximeter is reading 88% on room air and respiratory rate is 38 breaths per minute. Bacterial Pneumonia • Many infectious agents may cause “pneumonia”- viral, bacteria, fungal • Pediatric bacteria: pneumococcus, mycoplasma • Pneumococcus: sequela post URI, lobar infiltrate • DX= exam confirmed by CXR • Treatment: appropriate antimicrobial choice (PCN resistance?) • Prevention: vaccination Case 4 • Late in the afternoon you are seeing a 5 year old female with the chief complaint of shortness of breath. She has had URI symptoms for 3 days. Last night slept poorly and parents noted lack of energy and her complaints of “hard to breathe”. Parents note that she has had this pattern a few times in the past, but it was mild and never lasted more than 2 days. She has no fever but does show some accessory muscle use and intercostals retractions. Pale in color, her respiratory rate is 50 breaths per minute and oximeter is 88% on room air. Asthma: • Mechanism: spasm and/or edema of bronchioles • Etiology is inflammatory trigger: infection, allergy, exertion • Treatment: Beta 2 agonists, leukotriene inhibitors, corticosteroids • Prevention: education, pharmacologic agents, environmental control • Prognosis: resolution common under age 7 years, lifetime if older Case 5 • Later that night during your ER clerkship you are tagging with one of the ER doctors when one of the nurses grabs her by the arm and urgently guides her to an exam room. It holds a 5 week old male with poor color and extreme work of breathing- abdominal heaving, retractions and a respiratory rate of 80 breaths per minute. Heart rate is 187 beats per minute. Oximeter is 68%. Parents note that he was fine until this morning but seemed to have more difficulty eating until 30 minutes ago when he became limp and poorly responsive. Respiratory Syncytial Virus (RSV) • RNA virus • Marked coryza symptoms in older children • Children under age 2 often have asthma-like picture • Mechanism: bronchiolar edema/ severe mucosal damage • Treatment: supportive care • Prevention by passive immunization (monoclonal antibody) Case: • You are the first year FP resident doing your ER rotation and trying to get a quick supper in when your pager goes off. The ER charge nurse insists that you come immediately to assess a 2 y-o male in respiratory distress. • When you get to the exam room he is laying in his father’s arms, pasty in color with profound retractions, and poorly aware. HR=180, RR= 30, Oximeter = 82%. • Parents note that he was fine until this evening. They had been at a high school basketball game and he had been playing under the bleachers when he suddenly started to cough- progressing to respiratory distress. Foreign Body Aspiration • Generally under the age of two (up to four?) • Mechanism: f.b. migrating to airway causing ball valve obstructive effect • History= often sudden change in respiratory status • Exam= respiratory distress, asymmetric breath sounds • CXR= unilateral lung hyperexpansion (often right side) with possible mediastinal shift away from involved side • Treatment= removal of f.b. by bronchoscopy • Complications= pneumothorax, pneumonia Pediatric Respiratory Distress Last Thoughts • The respiratory system is the most vulnerable in Pediatrics • Deterioration may progress rapidly • Simple airway management techniques may buy time • Equipment required may have to be sized for age • Accurate, rapid assessment and graded supportive care take precedence over lavishing time on diagnosis