Ambulatory First Year 2015-2016
advertisement

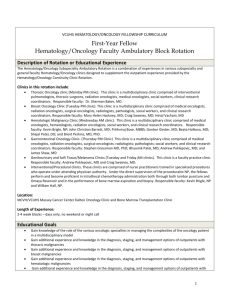
VCUHS HEMATOLOGY/ONCOLOGY FELLOWSHIP CURRICULUM First-Year Fellow Hematology/Oncology Faculty Ambulatory Block Rotation Description of Rotation or Educational Experience The Hematology/Oncology Subspecialty Ambulatory Rotation is a combination of experiences in various subspecialty and general faculty Hematology/Oncology clinics designed to supplement the outpatient experience provided by the Hematology/Oncology Continuity Clinic Rotation. Clinics in this rotation include: Thoracic / Head&Neck Oncology. This clinic is a multidisciplinary clinic comprised of interventional pulmonologists, thoracic surgeons, radiation oncologists, medical oncologists, social workers, clinical research coordinators. Responsible faculty: Drs. Erin Alesi, MD and Sherman Baker. Breast Oncology Clinic. This clinic is a multidisciplinary clinic comprised of medical oncologists, radiation oncologists, surgical oncologists, radiologists, pathologists, social workers, and clinical research coordinators. Responsible faculty: Charles Geyer, MD; Mary Helen Hackney, MD; Hetal Vachani, MBBS Hematologic Malignancy Clinic. This clinic is a multidisciplinary clinic comprised of medical oncologists, hematologists, radiation oncologists, social workers, and clinical research coordinators. Responsible faculty: Kevin Brigle, NP; John Christian Barrett, MD; Gordon Ginder, MD; Beata Holkova, MD; Shejal Patel, DO; Brent Perkins, MD, PhD; Danielle Shafer, DO; Christine Weidel, MD; and Victor Yazbeck, MD. Gastrointestinal Oncology Clinic. This clinic is a multidisciplinary clinic comprised of medical oncologists, radiation oncologists, surgical oncologists; radiologists; pathologists; social workers; and clinical research coordinators. Responsible faculty: Stephen Grossman MD, PhD; Khalid Matin, MBBS; and Bhaumik Patel, MBBS; and Asit Paul, MBBS. Genitourinary and Soft Tissue/Melanoma Clinics. This clinic is a faculty practice clinic. Responsible faculty: Sopipatros Boikos, MD; Asit Paul, MBBS; Andrew Poklepovic, MD and Craig Swainey, MD. Interventional/Procedural clinics. These clinics are comprised of nurse practitioners trained in specialized procedures who operate under attending physician authority. Under the direct supervision of the proceduralist NP, the fellows perform and become proficient in intrathecal chemotherapy administration both through both lumbar puncture and Omaya Reservoir and in the performance of bone marrow aspiration and biopsy. Responsible faculty: Kevin Brigle, NP and William Hall, NP. Location: MCVH/VCUHS Massey Cancer Center Dalton Oncology Clinic and Bone Marrow Transplantation Clinic Length of Experience: 2-4 week blocks – days only, no weekend or night call Educational Goals Gain knowledge of the role of the various oncologic specialties in managing the complexities of the oncology patient in a multidisciplinary model Gain additional experience and knowledge in the diagnosis, staging, and management options of outpatients with thoracic malignancies Gain additional experience and knowledge in the diagnosis, staging, and management options of outpatients with breast malignancies Gain additional experience and knowledge in the diagnosis, staging, and management options of outpatients with hematologic malignancies Gain additional experience and knowledge in the diagnosis, staging, and management options of outpatients with 1 gastrointestinal malignancies Gain experience and become proficient in intrathecal chemotherapy administration via lumbar puncture. Gain experience and become proficient in performing bone marrow aspiration and biopsy. Patient Care Goal Fellows must be able to provide patient care that is compassionate, appropriate, and effective for the treatment of health problems and the promotion of health. Please refer to overview of the fellowship curriculum for competencies/objectives for patient care. Specifically, fellows will see patients in all of these clinic settings under the supervision of the appropriate subspecialty faculty member. Fellows will participate in the evaluation and management of acutely and chronically ill oncology outpatients in order to learn the different approaches to subspecialty cancer treatment. Competencies Fellows are expected to: • Gather appropriate clinical information • Synthesize information into a care plan • Partner with patients/families in the implementation of the plan • Coordinate care plans with referring physicians, social workers, and home health agencies Objectives Fellows are expected to: • Develop skills in history/physical examination of the patient with cancer • Develop skills as an outpatient subspecialty consultant • Integrate clinical data in the formation of a comprehensive care plan • Document the encounter in the medical record in sufficient detail to communicate to other physicians and meet billing requirements • Provide compassionate, appropriate, and comprehensive patient care through: o Responding to requests for outpatient consultation, evaluation and/or management in a timely and appropriate fashion, o Providing appropriate follow-up management Medical Knowledge Goal Fellows must demonstrate knowledge of established and evolving biomedical, clinical, epidemiological, and social-behavioral sciences, as well as the application of this knowledge to patient care. Competencies Fellows are expected to demonstrate skills in: Acquisition of knowledge Analysis of information Application of knowledge Objectives All fellows are expected to: Demonstrate the ability to perform a comprehensive and accurate physical examination; demonstrate the ability to arrive at an appropriate differential diagnosis; outline a logical plan for specific and targeted investigations pertaining to the patient’s complaints; and formulate a plan for management and follow-up treatment of the patient Demonstrate their knowledge by presenting the results of a consultation orally and in writing and by defending the 2 clinical assessment, differential diagnosis, and diagnostic and management plans Content-Specific Objectives Thoracic Oncology Demonstrate knowledge of epidemiology and work up of thoracic oncology. Recognize the treatment options for thoracic malignancy as related to the disease stage Identify and manage complications of the treatment of thoracic cancers such as radiation pneumonitis, infection, dyspnea Recognize the importance of palliation of symptoms including pain and dyspnea in patients with thoracic malignancies. Recall the interventional options for patients with thoracic malignancies and pleural effusions for palliative purposes Understand the importance of clinical trials in thoracic malignancies Breast Oncology Demonstrate knowledge of the diagnosis, staging and management of breast cancer Demonstrate knowledge of the treatment of breast malignancy and its relationship to disease stage Demonstrate the ability to access and use the available prognostic models and online lines used in the management of breast cancer including but not limited to the Gail model, the Claus model, Adjuvant online and OncotypeDX. Identify and manage complications of the treatment of breast cancers Recognize the importance of palliation of symptoms in patients with breast malignancies. Understand the importance of clinical trials in breast malignancies Hematologic Malignancies Demonstrate the knowledge of the WHO classifications, prognostic scores, and staging used for the hematologic malignancies Demonstrate an understanding of the diagnostic modalities used in differentiating hematologic malignancies such as lymph node biopsy, bone marrow biopsy, flow cytometry, molecular assays, and cytogenetics along with means of demonstrating clonality in hematologic malignancies Understand the importance of clinical trials in hematologic malignancies Gastrointestinal Oncology Demonstrate knowledge of epidemiology, work up, and staging of GI oncology. Demonstrate a knowledge of the treatments of GI malignancy as they relate to disease stage Identify and manage complications of the treatment of GI cancers such as pain, mucositis, infection, and diarrhea Recognize the importance of palliation of symptoms in patients with GI malignancies. Understand the importance of clinical trials in GI malignancies Practice- Based Learning and Improvement Goal Fellows must demonstrate the ability to investigate and evaluate their care of patients, to appraise and assimilate scientific evidence, and to continuously improve patient care based on constant self-evaluation and life long learning. Please refer to overview of the fellowship curriculum for competencies/objectives for practice based learning and improvement. Systems Based Practice Goal Fellows must demonstrate an awareness of and responsiveness to the larger context and system of health care, as well as the ability to call effectively on other resources in the system to provide optimal health care. Please refer to overview of the fellowship curriculum for competencies/objectives for systems based practice. 3 Professionalism Goal Fellows must demonstrate a commitment to carrying out professional responsibilities and an adherence to ethical principles. Please refer to overview of the fellowship curriculum for competencies/objectives for professionalism. Interpersonal and Communication Skills Goal Fellows must demonstrate interpersonal and communication skills that result in the effective exchange of information and teaming with patients, their families, and professional associates. Please refer to overview of the fellowship curriculum for competencies/objectives for interpersonal and communication skills. Teaching Methods Clinical teaching Role modeling Patient care/clinical experience Didactic sessions (division, department, institution) Performance feedback Self-directed learning Assessment of Fellow Performance Evaluation by the attending of the fellow Procedural assessment of each performed procedure by the supervising faculty member Assessment of Rotation Annual program review Discussions with fellows during biannual review Review in-service and ABIM exam results Level of Supervision For non-procedural patient encounters supervision is indirect with direct supervision immediately available by adulttrained hematology and/or oncology physicians All procedures during the rotation are performed under the direct supervision of a faculty member Educational Resources Devita, Hellman, and Rosenberg’s Cancer: Principles and Practice of Oncology (9th Edition) Hoffman Hematology: Basic Principles and Practice (4th Edition) UpToDate ASCO University ASCO Practice and Guidelines ASCO-SEP ASH-SEP NCCN Guidelines (www.nccn.org) NCI Common Cancer Types and Clinical Trails by Cancer Type/Disease (www.cancer.gov) The AJCC 7th edition TMN staging of Cancer 4 Common Toxicity Criteria v4.0 (aka Common Terminology Criteria for Adverse Events) GAIL model Claus model Adjuvant! Online 5