2, Intern rapport
advertisement
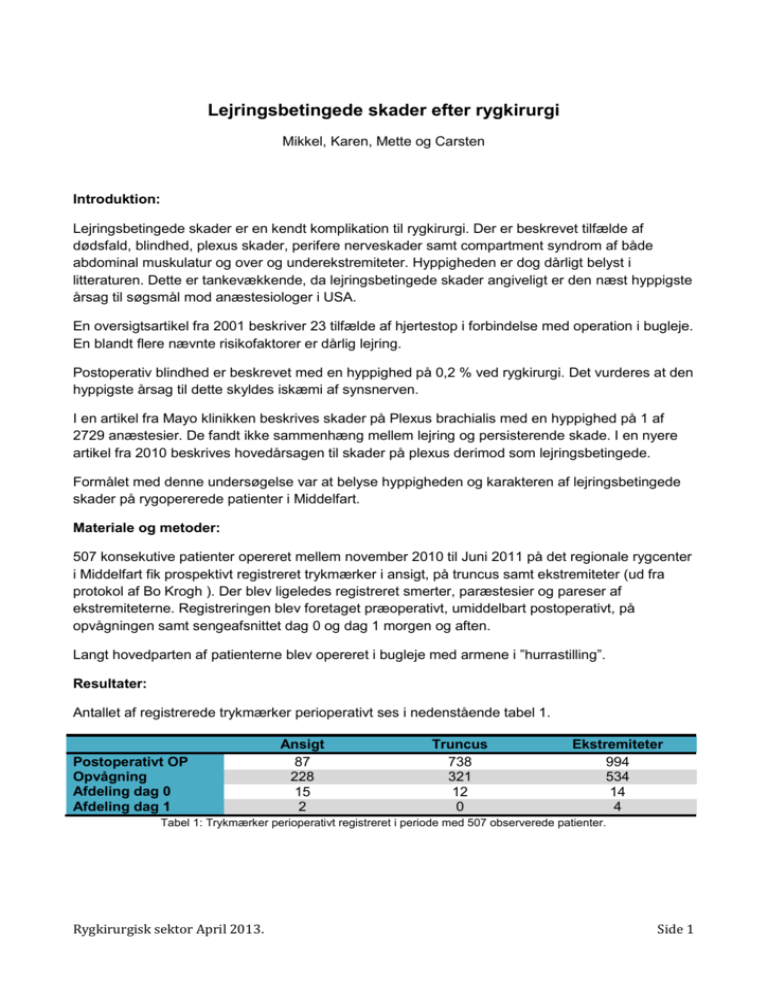
Lejringsbetingede skader efter rygkirurgi Mikkel, Karen, Mette og Carsten Introduktion: Lejringsbetingede skader er en kendt komplikation til rygkirurgi. Der er beskrevet tilfælde af dødsfald, blindhed, plexus skader, perifere nerveskader samt compartment syndrom af både abdominal muskulatur og over og underekstremiteter. Hyppigheden er dog dårligt belyst i litteraturen. Dette er tankevækkende, da lejringsbetingede skader angiveligt er den næst hyppigste årsag til søgsmål mod anæstesiologer i USA. En oversigtsartikel fra 2001 beskriver 23 tilfælde af hjertestop i forbindelse med operation i bugleje. En blandt flere nævnte risikofaktorer er dårlig lejring. Postoperativ blindhed er beskrevet med en hyppighed på 0,2 % ved rygkirurgi. Det vurderes at den hyppigste årsag til dette skyldes iskæmi af synsnerven. I en artikel fra Mayo klinikken beskrives skader på Plexus brachialis med en hyppighed på 1 af 2729 anæstesier. De fandt ikke sammenhæng mellem lejring og persisterende skade. I en nyere artikel fra 2010 beskrives hovedårsagen til skader på plexus derimod som lejringsbetingede. Formålet med denne undersøgelse var at belyse hyppigheden og karakteren af lejringsbetingede skader på rygopererede patienter i Middelfart. Materiale og metoder: 507 konsekutive patienter opereret mellem november 2010 til Juni 2011 på det regionale rygcenter i Middelfart fik prospektivt registreret trykmærker i ansigt, på truncus samt ekstremiteter (ud fra protokol af Bo Krogh ). Der blev ligeledes registreret smerter, paræstesier og pareser af ekstremiteterne. Registreringen blev foretaget præoperativt, umiddelbart postoperativt, på opvågningen samt sengeafsnittet dag 0 og dag 1 morgen og aften. Langt hovedparten af patienterne blev opereret i bugleje med armene i ”hurrastilling”. Resultater: Antallet af registrerede trykmærker perioperativt ses i nedenstående tabel 1. Postoperativt OP Opvågning Afdeling dag 0 Afdeling dag 1 Ansigt 87 228 15 2 Truncus 738 321 12 0 Ekstremiteter 994 534 14 4 Tabel 1: Trykmærker perioperativt registreret i periode med 507 observerede patienter. Rygkirurgisk sektor April 2013. Side 1 Præoperativt Postoperativt Opvågning Afdeling dag 0 Afdeling dag 1 Smerter skulder Hø/Ve 40/36 Smerter Arm Hø/Ve Paræstesier arm Hø/Ve 32/41 Pareser arm Hø/Ve 0/1 Pareser UE Hø/Ve 4/7 44/28 6/3 4/6 2/2 10/7 8/11 7/9 14/13 11/14 4/4 0/1 0/2 0/0 4/2 1/2 0/2 Tabel 2: Registrering af smerter, paræstesier og pareser i ekstremiteter, i periode med 507 observerede patienter . Som det fremgår af Tabel 2 er den hyppigste præoperative klage skulder smerter. Ca. 30 timer postoperativt er den hyppigste klage smerter i armene. De to patienter som registreres med pareser i UE 1. dag postoperativt, er efterfølgende gennemgået i eletronisk patientjournal, hvor det konkluderes at patienternes pareser opfattes som komplikationer i forbindelse med grundlidelse og kirurgi. Diskussion: Lejringsbetingede skader kan og skal forhindres, da de kan overskygge et ellers godt kirurgisk resultat. Vi har i registreringsperioden været forskånet for alvorlige lejringsbetingede skader. Der er således ikke registreret pareser i overekstremiteterne og under 1 % af patienterne klager over paræstesier 30 timer postoperativt. Konklusion: Da de registrerede trykmærker stort set forsvinder 1 dag postoperativt, og de præoperative registreringer for smerter /paræstesier ikke kan skyldes lejringsskader, vurderer vi, at vores nuværende lejrings procedurer er sufficiente. Fremover oprettes kun et registrerings skema, hvis patienten postoperativt klager over gener eller personalet bemærker lejringsgener. Rygkirurgisk sektor April 2013. Side 2 Referencer: Resuscitation. 2001 Aug;50(2):233-8. Cardiac arrest during surgery and ventilation in the prone position: a case report and systematic review. Brown J, Rogers J, Soar J. Source Aneasthetics Department, Southmead Hospital, North Bristol NHS Trust, Bristol BS10 5NB, UK. Abstract We present a case report of successful resuscitation following cardiac arrest in a patient undergoing surgery in the prone position. A systematic review of the literature identified 22 further cases. Risk factors for intra-operative cardiac arrest in patients in the prone position include: cardiac abnormalities in patients undergoing major spinal surgery, hypovolaemia, air embolism, wound irrigation with hydrogen peroxide, poor positioning and occluded venous return. Cardiac arrest is also a risk in the increasing number of patients with acute respiratory distress syndrome ventilated in the prone position. Management of prone cardiac arrest may be improved by identification of high-risk patients, careful patient positioning, use of invasive monitoring and placement of self-adhesive defibrillator paddles. Suitable techniques for cardiopulmonary resuscitation including methods for chest compression, defibrillation and the management of air embolism are discussed. PMID: 11719152 [PubMed - indexed for MEDLINE] J Clin Anesth. 2003 Sep;15(6):471-3. Unusual presentation and complication of the prone position for spinal surgery. Ali AA, Breslin DS, Hardman HD, Martin G. Source Department of Anesthesiology, Duke University Medical Center, Durham, NC 27710, USA. Abstract Patient positioning for operative procedures has long been associated with perioperative complications. We present a case report of shoulder dislocation, which occurred following positioning in the prone position, and was detected by axillary artery occlusion resulting in the loss of the radial artery blood pressure line waveform. We discuss the diagnosis and consequences of this complication. Anesth Analg. 2006 May;102(5):1538-42. Rygkirurgisk sektor April 2013. Side 3 The use of somatosensory evoked potentials to determine the relationship between patient positioning and impending upper extremity nerve injury during spine surgery: a retrospective analysis. Kamel IR, Drum ET, Koch SA, Whitten JA, Gaughan JP, Barnette RE, Wendling WW. Source Department of Anesthesiology, Temple University Hospital and School of Medicine, Philadelphia, Pennsylvania 19140, USA. ihab.kamel@temple.edu Abstract Somatosensory evoked potential (SSEP) monitoring is used to prevent nerve damage in spine surgery and to detect changes in upper extremity nerve function. Upper extremity SSEP conduction changes may indicate impending nerve injury. We investigated the effect ofoperative positioning on upper extremity nerve function retrospectively in 1000 consecutive spine surgeries that used SSEP monitoring. The vast majority (92%) of upper extremity SSEP changes were reversed by modifying the arm position and were therefore classified as position-related. The incidence of positionrelated upper extremity SSEP changes was calculated and compared for five different surgical positions: supine arms out, supine arms tucked, lateral decubitus position, prone arms tucked, and the prone "superman" position. The overall incidence of position-related upper extremity SSEP changes was 6.1%. The lateral decubitus position (7.5%) and prone superman position (7.0%) had a significantly more frequent incidence of position-related upper extremity SSEP changes (P < 0.0001, Z-test for Poisson counts) compared with other positions (1.8%-3.2%). No patient with a reversible SSEP change developed a new postoperative deficit in the affected extremity. SSEP monitoring is of value in identifying and reversing impending upper extremity peripheral nerve injury. Comment in The following popper user interface control may not be accessible. Tab to the next button to revert the control to an accessible version. Destroy user interface controlA soft cervical collar may help prevent neck sprain or nerve injury from occurring after surgery in the lateral decubitus position. [Anesth Analg. 2006] J Neurosurg Spine. 2010 Oct;13(4):552-8. doi: 10.3171/2010.4.SPINE09682. Brachial plexus injury following spinal surgery. Uribe JS, Kolla J, Omar H, Dakwar E, Abel N, Mangar D, Camporesi E. Source Department of Neurological Surgery, University of South Florida, USA. juansuribe@gmail.com Abstract OBJECT: In the present study, the authors identified the etiology, precipitating factors, and outcomes of perioperative brachial plexus injuriesfollowing spine surgery. Rygkirurgisk sektor April 2013. Side 4 METHODS: We reviewed all the available literature regarding postoperative/perioperative brachial plexus injuries, with special concern for thepatient's position during surgery, duration of surgery, the procedure performed, neurological outcome, and prognosis. We also reviewed the utility of intraoperative electrophysiological monitoring for prevention of these complications. RESULTS: Patient malpositioning during surgery is the main determining factor for the development of postoperative brachial plexus injury. Recovery occurs in the majority of cases but may require weeks to months of therapy after initial presentation. CONCLUSION: Brachial plexus injuries are an increasingly recognized complication following spinal surgery. Proper attention to patient positioning with the use of intraoperative electrophysiological monitoring techniques could minimize injury. Spine (Phila Pa 1976). 2008 Dec 15;33(26):2938-41. doi: 10.1097/BRS.0b013e31818b9029. Face tissue pressure in prone positioning: a comparison of three face pillows while in the prone position for spinal surgery. Grisell M, Place HM. Source Department of Orthopaedic Surgery, Saint Louis University, Saint Louis, MO 63110, USA. Abstract STUDY DESIGN: This is a prospective, randomized study. OBJECTIVE: The purpose was to compare the tissue-pillow interface pressures at the forehead and chin in patients positioned in the pronefashion for spinal surgery on each of 3 facial positioners. SUMMARY OF BACKGROUND DATA: Facial pressure ulcers have been infrequently observed after spinal surgery requiring prone positioning. This requires the use of a specially designed head positioner to maintain spinal alignment and to allow space for the endotracheal tube. METHODS: We enrolled 66 consecutive elective thoracic and/or lumbar surgery patients from 18 to 65 years of age. Patients were randomized on entry into the study to 1 of 3 positioners. Facial tissue pressures were measured at the patient's forehead and chin at times 0, 5, 15, and 60 minutes of positioning. The integrity of the patient's skin was recorded and classified at the end of surgery. RESULTS: The pressures measured for the Dupaco positioner were lower at all time points at both the forehead and the chin in comparison with the other 2 positioners (P < 0.05). The ROHO and the OSI positioners created similar chin pressures at all time points (P > 0.05). The pressures at the forehead for the ROHO positioner were significantly less than those for the OSI positioner at all time points (P < 0.05). Tenpatients on the OSI positioner had pressure ulcers at the end of the procedure. CONCLUSION: The Dupaco ProneView Protective Helmet System is superior to both the OSI and the ROHO positioners in decreasing forehead and chin tissue interface pressures during prone position surgery. Rygkirurgisk sektor April 2013. Side 5 PMID: 19092629 [PubMed - indexed for MEDLINE] Am J Ophthalmol. 2008 Apr;145(4):604-610. doi: 10.1016/j.ajo.2007.09.016. Perioperative visual loss after nonocular surgeries. Newman NJ. Source Department of Ophthalmology, Emory University School of Medicine, Atlanta, Georgia, USA. ophtnjn@emory.edu Abstract PURPOSE: To review the current knowledge of persistent visual loss after nonocular surgeries under general anesthesia. DESIGN: Perspective. METHODS: Literature review. RESULTS: The incidence of perioperative visual loss after nonocular surgeries ranges from 0.002% of all surgeries to as high as 0.2% of cardiac and spine surgeries. Any portion of the visual pathways may be involved, from the corneas to the occipital lobes, but the most common site of permanent injury is the optic nerves, and the most often presumed mechanism is ischemia. Anterior ischemic optic neuropathy (AION) is more prevalent among cardiac surgery patients and posterior ischemic optic neuropathy (PION) predominates among those who have had spine and neck procedures. Patients range from age five to 81 years and typically awake with severe bilateral visual loss. Multiple factors have been proposed as risk factors for perioperative ION, including long duration in the prone position, excessive blood loss, hypotension, anemia, hypoxia, excessive fluid replacement, use of vasoconstricting agents, elevated venous pressure, head positioning, and a patient-specific vascular susceptibility that may be anatomic or physiologic. However, the risk factors for any given patient or procedure may vary and are likely multifactorial. CONCLUSIONS: If, when an ophthalmologist is consulted for a patient with perioperative visual loss, an obvious ocular cause is not apparent, urgent neuroimaging should be obtained to rule out intracranial pathology. Anterior and posterior ION should be considered and careful documentation is essential. Currently, the pathogenesis of perioperative ION remains unclear, and preventive and therapeutic measures remain elusive. Anesthesiology. 1994 Dec;81(6):1332-40. Ulnar neuropathy. Incidence, outcome, and risk factors in sedated or anesthetized patients. Rygkirurgisk sektor April 2013. Side 6 Warner MA, Warner ME, Martin JT. Source Mayo Medical School, Rochester, Minnesota. Abstract BACKGROUND: Ulnar neuropathy is well-recognized as a potential complication of procedures performed on anesthetized patients. However, reported outcomes and risk factors for this problem are based on small series and anecdotes. METHODS: We retrospectively reviewed the perioperative courses of 1,129,692 consecutive patients who underwent diagnostic and noncardiac surgical procedures with concurrent anesthetic management at the Mayo Clinic from 1957 through 1991 (inclusive). The medical diagnoses of patients who had these procedures were scanned for 26 diagnoses associated with neuropathy. Persistent neuropathy of anulnar nerve was defined as a sensory or motor deficit of greater than 3 months' duration. Risk factors anecdotally associated with persistentneuropathy were analyzed by comparing patients with an ulnar neuropathy with control subjects in a 1:3 case-control study. RESULTS: Persistent ulnar neuropathies were identified in 414 patients, a rate of 1 per 2,729 patients. Of these, 38 (9%) patients had bilateralneuropathies. Approximately equal numbers of the neuropathies included sensory loss only or mixed sensory and motor loss. Initial symptoms form most neuropathies were noted more than 24 h after the procedure. Factors associated with persistent ulnar neuropathyincluded male gender and a duration of hospitalization of more than 14 days (P < 0.01). Neuropathy was more likely to develop in very thin and obese patients than in patients with average body habitus. Neither the type of anesthetic technique nor the patient position was found to be associated with this neuropathy. Of the 382 patients who survived the 1st postoperative yr, 53% regained complete motor function and sensation and were asymptomatic. Of those with neuropathies persisting for more than 1 yr, most had moderate or greater disability from pain or weakness. CONCLUSIONS: These data suggest that perioperative ulnar neuropathies are associated with factors other than general anesthesia and intraoperative positioning. Men at the extremes of body habitus who have prolonged hospitalizations are particularly susceptible to development of ulnar neuropathies. Comment in The following popper user interface control may not be accessible. Tab to the next button to revert the control to an accessible version. Destroy user interface controlPerioperative ulnar neuropathy: are we ready for shortcuts? [Anesthesiology. 1994] The following popper user interface control may not be accessible. Tab to the next button to revert the control to an accessible version. Destroy user interface controlPeri- or postoperative ulnar neuropathy? [Anesthesiology. 1995] Rygkirurgisk sektor April 2013. Side 7


![[Session A] Kontakten til sundhedsvæsenet](http://s3.studylib.net/store/data/009732071_1-90e7c7dc246805d636794996a581b450-300x300.png)