Hjertesvigtsdiagnostik & Hospitaliseringsrisiko
advertisement
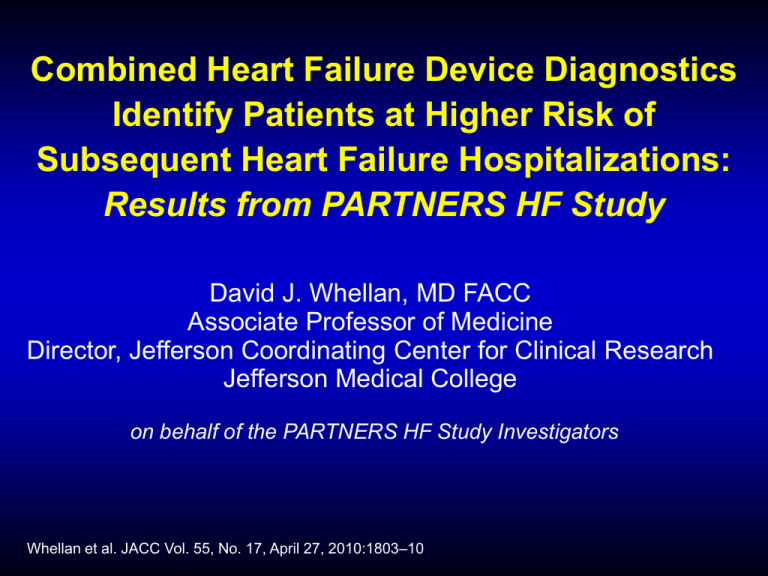
Combined Heart Failure Device Diagnostics Identify Patients at Higher Risk of Subsequent Heart Failure Hospitalizations: Results from PARTNERS HF Study David J. Whellan, MD FACC Associate Professor of Medicine Director, Jefferson Coordinating Center for Clinical Research Jefferson Medical College on behalf of the PARTNERS HF Study Investigators Whellan et al. JACC Vol. 55, No. 17, April 27, 2010:1803–10 Disclosure I will not discuss off label use or investigational use in my presentation. I have financial relationships to disclose: Employee of: Thomas Jefferson University Consultant for: Medtronic Stockholder in: NA Research support from: Medtronic Honoraria from: Medtronic Background • Despite medical interventions, there remains a high rate of HF hospitalizations in the CRT-D patient population. • Identifying at risk patients is a challenge • Recent publications have shown a single parameter HF diagnostic identifies high risk patients 1,2 1. Small et al. J Card Fail. November 2009; 15(9):813. 2. Perego et al. Interv Card Electrophysiol 2008, 23:235-242. Hypothesis Routine evaluation of combined diagnostics recorded by implantable devices can identify HF patients at risk for subsequent heart failure hospitalizations. Combined Diagnostic Algorithm • Based on 8 Diagnostic trends which are recorded daily • Individual algorithms for each trend have been used to flag significant observations from the trends in Medtronic ICDs/CRTs OptiVol VT/VF therapy AF burden Rate during AF %CRT HR Activity HRV Study Design • Prospective observational study • Subjects with CRT ICDs • 12-month follow-up, scheduled visits every 3 months • Clinical and device data collected at all visits • Limitations: Clinicians had access to the diagnostics Review and/or interventions based on trends were not required and alerts were not utilized Methods – Categorization of Events • All CV and HF-related events were collected • Events and deaths were classified and adjudicated by an independent committee • Primary endpoint was the number of HF hospitalizations with pulmonary congestion Combined Algorithm Positive Combined Algorithm = any 2 criteria + Parameter Criterion Fluid Index AT/AF Duration V. rate during AT/AF Patient Activity Night Heart Rate HRV CRT % Pacing Shock(s) ≥60 ohm/days ≥6 hours & not persistent AT/AF AT/AF ≥24 hrs & V. ≥ 90 bpm Avg. <1 hr over 1 week ≥85 bpm for 7 consecutive days <60 ms for 7 consecutive days < 90% for 5 of 7 days 1 or more shocks OR Fluid Index ≥100 Combined Algorithm • Algorithm criteria were tested on an independent data set from a registry (819 patients) to determine optimal # of criteria met to trigger combined algorithm # Criteria Evaluations 1 43% too high 2 14% optimal 3 3% too few • Combined algorithm also used prior finding that a high (≥100) fluid index alone has higher specificity Monthly Evaluation Model Start* 30 Diagnostic Risk Assessment 1 60 90 ...Repeat until End of Follow-up HF Event Assessment 1 Evaluation 1 Diagnostic Risk Assessment 2 HF Event Assessment 2 Evaluation 2 Diagnostic Risk Assessment 3 HF Event Assessment 3 Evaluation 3 * Day 0 = later of consent date or 60 days post-implant • Repeated using Quarterly (90 days) and Semi-monthly (15 days) evaluations Statistical Methods • Cox proportional hazards model to adjust for pre-defined clinical variables including: Age Gender Heart Failure Etiology NYHA Class* Diabetes HF Medication Regimen (Diuretics, ACE/ARB, B-Blocker)* * Most recent prior to evaluation • Sub-group analysis for subjects with and without a HF event. Results: Cohort and Event Rates • 694 patients in this analysis cohort who had impedance monitoring and >2 months of FU • 60 patients (8.5%) had 78 monthly evaluation periods with at least one HF hosp. (pulmonary) • Low event rate: 1.4% (78/5693) of monthly evaluations had HF hosp. (pulmonary) Baseline Characteristics (N = 694) Age 68 yrs Female 33% African American 11% NYHA (Class III) 95% History of AF 26% Ischemic HF 62% Diabetic 40% Diuretics 83% ACE Inhibitor or ARB 81% Beta Blockers 89% Combined Diagnostics Triggered 1324 monthly evaluations with combined algorithm triggered ≥ 2 Diagnostic Criteria Met 43% % of evaluations when ≥2 Diagnostic Criteria Met (N = 960) 75% OptiVol Fluid Index ≥100 ohm days Met 29% 67% 28% % of triggered evaluations 62% 60% 43% 45% 30% 21% 18% 14% 15% 7% 5% 0% AF AF+RVR OptiVol Low Night Index ≥60 Activity HR Low HRV Low ICD Shock(s) Pacing% Evaluations with Heart Failure Hospitalization (Pulmonary) Kaplan-Meier HF Hospitalization Curves 6% P < 0.0001 Hazard Ratio = 5.5 (95% CI: 3.4 – 8.8) 5% + Diagnostic 4% 3% 2% 1% - Diagnostic 0 0 10 20 30 Days After Diagnostic Evaluation Risk of a HF hosp. for pts with + Diagnostic was 5.5 x risk of pts w/ - Diagnostic Multivariable Analysis P-Value 1 Age 0.90 0.7 Gender 0.15 1 Heart Failure Etiology 0.91 1.4 NYHA Class* 0.18 1.6 Diabetes (@baseline) 0.06 1.6 Diuretics* 0.35 0.7 ACE/ARB* 0.7 0.9 Beta-Blockers* 0.90 4.8 + Combined Diagnostic * Before evaluation date 0 1 2 3 4 5 <0.0001 6 7 8 Hazard Ratio Patients w/ + combined diagnostic were 4.8 times more likely to have a HF hospitalization with pulmonary congestion independent of other clinical variables. Subgroup by HF Event 0.9 5.4 0.9 Subjects with P = 0.85 5.4 Pulm HF Hosp. -1 1 3 5 7 9 -1 1 3 5 7 9 7 9 0.9 P < 0.0001 5.4 Subjects without Pulm. HF Hosp. -1 1 3 5 Effect of Evaluation Frequency Evaluation Frequency 6.9 15 Days (Semi-Monthly) 5.5 30 Days (Monthly) 3.1 90 Days (Quarterly) -1 1 3 5 7 9 11 Hazard Ratio • More frequent evaluations enhance risk stratification. • Monthly evaluations provide reasonable balance of risk stratification benefit and clinician effort. Conclusion • Patients with a + combined diagnostic were 5.5x more likely to have a HF hospitalization with pulmonary congestion before the next evaluation • The combined algorithm is an independent predictor of HF hospitalization in patients without a HF hospitalization, while it provides limited information in patients who have experienced a HF hospitalization. Clinical Implications • Monthly evaluation of combined diagnostics can identify patients at a higher risk of a HF hospitalization within the next month. • Intervening by either modification of medications (i.e. diuretic dosing) or increase surveillance (i.e. clinic visit) may reduce clinical events HF Hosp. w/Pulm. Cong. 30 Day Evaluation window Case Study 1 AF+ Fluid + Case Study 2 HF Hospitalization with Pulmonary Congestion Evaluation Window OptiVol Index+ Activity+ HRV+

![[Session A] Kontakten til sundhedsvæsenet](http://s3.studylib.net/store/data/009732071_1-90e7c7dc246805d636794996a581b450-300x300.png)