Clinical Journal I - Georgetown Digital Commons
advertisement

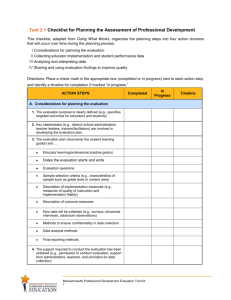
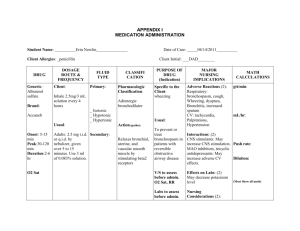
1 Running head: CLINICAL GUIDED JOURNAL 1 Clinical Guided Journal I Lauren Walker Georgetown University 2 CLINICAL GUIDED JOURNAL 1 For the Acute and Critical Care Clinical Nurse Specialist I clinical, I am working at Georgetown University Hospital (GUH) in the Neuroscience Critical Care Unit (NSICU). My preceptor, Stephen (Steve) Risch, RN, MSN, CCRN, CCNS, is the clinical educator for the Neuroscience ICU. While my preceptor does have his CCNS certification, he is hired at Georgetown University Hospital as a Clinical Educator. Below, you will see a diagram of the chain of command for the Clinical Educators. As a Clinical Educator, Steve is hired under the Clinical Education program, along with 11 other Clinical Educators. The educators, all on the same level, report directly to and are evaluated by the Clinical Education Director. Each Clinical Educator also works directly with a unit of their expertise at the hospital. On the NSICU, there is also a chain of command and role responsibility. At the top of the chain of command, is the Critical Care and Neurosciences Director, below her is the Neurosciences Specialty Director, then the Clinical Manager and Clinical Educator are on the same level, and lastly there is the nursing staff. According to Steve, though the Clinical Manager and Clinical Educator are on the same level, he feels as if the Clinical Manager has more authority for unit based decisions. This is due partially due to the financial position of the unit, reporting from the critical care and neurosciences director and role responsibility. While his role as the Clinical Educator is essential on the unit and drives many decisions on the unit, Steve believes that a disadvantage is that he reports back to the Education Department instead of the unit based chain of command. He also states that in his role, to create change on the unit, it is essential to have the support of both the unit manager and the neurosciences director. Figure 1 below is a diagram which was drawn and explained to me by my clinical preceptor which described the chain of command on his unit. 3 CLINICAL GUIDED JOURNAL 1 Figure 1: Georgetown University Hospital Chain of Command in the NSICU. Below you will find the job description of the Clinical Educator provided to me by my clinical preceptor: Provides educational leadership for professional nursing practice, to achieve autonomy and accountability, and to advance the mission and goals of the Department of Nursing/GUH, through collaborative relationships within the medical center, as well as through local, regional and national arenas. Provides direct patient care continually monitoring and evaluating the quality of care and services that are provided on the units. In collaboration with central nursing education staff, nursing management, and clinical nurse specialists, exemplifies and promotes excellence in practice, education, and professional growth. Graduate of an NLN accredited School of Nursing; BSN or MSN preferred. Current D.C. licensure as a Registered Professional Nurse. Five years clinical experience including two years in a university teaching hospital. Clinical education experience desirable. Further, another more specific description describes the Neurosciences ICU Clinical Educator: GENERAL DESCRIPTION: The incumbent in this position develops, coordinates, implements and evaluates all educational programs and activities for all staff in the Department of Neurosciences Critical Care. These functions are performed in accordance with all applicable laws and regulations and 4 CLINICAL GUIDED JOURNAL 1 Georgetown University Hospital's philosophy, policies, procedures and standards. EDUCATION AND OR TRAINING REQUIRED: Graduate of an accredited School of Nursing. Master's degree in Nursing, Education and/or related field. LICENSURE AND OR CERTIFICATION: Current D.C. license as a Registered Professional Nurse. Current BCLS Certification as an instructor. EXPERIENCE: Three years of clinical experience in an ICU with at least one year of previous teaching experience. Supervisory experience desirable. SPECIAL KNOWLEDGE/SKILLS/ABILITIES: Current knowledge of Neurosciences Critical Care nursing. Knowledge and skill in the area of program development, adult learning theories as applied to the NSICU setting, A/V equipment. Must be able to facilitate individual and group dynamics. Must also have effective interviewing skills, be flexible and able to work under stress, act as a resource person and work with all levels of staff. Through working with my clinical educator, I have realized that a CNS is certainly an educator; however the CNS is able to take their job and responsibility to the next level of clinical and nursing excellence. However, an educator cannot be a CNS. These two descriptions of the Neuroscience ICU are certainly broad descriptions of the job and responsibility. This job, a Clinical Educator, is targeted for an individual with several years of experience in the NSICU, is either BSN/MSN certified, is good under stress and can act as a resource, not CNS specific. However, when looking closely, one can see that these descriptions do describe many characteristics of the Synergy Model and APN and a CNS can take the description and add in the benefits of the APN. The first description highlights many specific CNS characteristics. The job description first highlights the importance of leadership for professional nursing practice, which places a high responsibility on the educator as a role model including autonomy and accountability. Another Synergy characteristic, collaboration is evident in the description, “collaborative relationships within the medical center, as well as through local, regional and national arenas”. The characteristic of collaboration is also clear in the 5 CLINICAL GUIDED JOURNAL 1 description with the statement of, “In collaboration with central nursing education staff, nursing management, and clinical nurse specialists, exemplifies and promotes excellence in practice, education, and professional growth.” The position requires the individual to be a facilitator of learning and challenge their team through clinical inquiry by “monitoring and evaluating the quality of care and services that are provided on the units”. The individual will also honor systems thinking by honoring and practicing through Georgetown University Hospital's philosophy, policies, procedures and standards. While not clearly defined in the job description, the other four aspects of the Synergy Model, including clinical judgment, moral advocacy, caring practices, and response to diversity are implied as the educator will make sure that all nurses are following best practice standards, advocate for best treatment and patient care, and work with all patients from all patient populations. The second job description has roles that fall outside the CNS responsibilities. The standards of knowledge of Neurosciences Critical Care nursing, having skill in the area of program development, knowledge of A/V equipment, and have effective interviewing skills are not specific to the CNS. While this is a description of a Clinical Educator, my preceptor takes his role and responsibility of the Clinical Educator and then takes his training as an APN and the characteristics of the Synergy Model to fully influence his role in the NSICU. Since there is no formal CNS job description at Georgetown University Hospital, he is able to expand staff training and education through the use of evidence based practice and national standards. Attached to this document are the specific categories in the clinical evaluation of my preceptor. These 12 sections are submitted to each educator to fill out on their own. They can contribute as much or as little to prove that they met these expected standards. The evaluation is then given back to the Educator Director to score and to agree or disagree with the self-reported comments as well as comment themselves. While there are evaluation points that correlate with the job description, it is important that 6 CLINICAL GUIDED JOURNAL 1 the educator understands what they are being evaluated on prior to starting since there are many sections and topics that are not discussed in the job description. It is clear in the job description that the Educator must participate in performance improvement on their unit, provide nursing and new graduate education and training through the Adult Learning Theory, promote the values of Georgetown University Hospital, collaborate with other educators, nurses, and the entire multi-disciplinary team and be a role model. Evaluation criteria not mentioned in the job description include participating on committees, councils and task forces, and working with and providing education for undergraduate and graduate nursing students. While it is the main responsibility of the Education Director to submit the evaluations, there is no place for the Critical Care and Neurosciences Director or Floor Manager to comment on the Educator’s role over the past year. The unit based positions work every day with my preceptor and sees the impact he has on the unit on a daily basis. Therefore, my preceptor is working to change the evaluation criteria to include a place for unit specific feedback of the Educator. If I could change this evaluation, I would have two very different sections of the evaluation. It is appropriate that the Educator is evaluated by the Education Director on specific sections such as new graduate education, committee and task force participation and attendance. However, I think it is equally as important for the units to evaluate their educator regarding other categories such as needs assessment, intervention with the nursing staff, collaboration within the neuroscience team, working to change policies and procedures and making an overall impact on best practice standards on the unit. Steve functions as a clinical expert on a daily basis in the neurosciences ICU. He takes his past experience, knowledge and skill, continues to follow current evidence based guidelines and implements them into the NSICU. He is able to expand on his position as an educator to advance his staff on the Advanced Practice level. Since there is no specific job description of the CNS role, his CNS job 7 CLINICAL GUIDED JOURNAL 1 expectations are all informal while practicing at GUH. To formalize and validate his job and role as a CNS, the Synergy model drives his core actions and interventions as an APN. In his role as an educator, Steve recognizes the importance of going beyond basic education and to fully evaluate what is the best and most recent evidence to provide best practice care to patients. Steve validates and expands his clinical knowledge through clinical inquiry to continue to recognize the importance of best practice and knowledge in the clinical setting. To continue to question and evaluate best practice, Steve consistently investigates new literature and exercises literature reviews and compares them to his unit’s policies and procedures for validation or revision. Recently, Steve included me in this practice as we reevaluated the policy and procedure on insertion and monitoring of the patient with an EVD. The American Association of Neuroscience Nurses recently published the most recent literature describing the care and treatment of the patient with an EVD according to patient outcomes. After reviewing this literature and recommendations, we looked at our policy and were able to revise it so it met and followed national and best practice standards. Also by exercising clinical inquiry, it enables and enhances the ability of my preceptor use his clinical judgment on the unit in clinical practice. I see him using his past clinical experience and skills to reason, critically think, and help make clinical decisions. He places a high priority on his nurses to critically evaluate their patient condition and interventions. Every morning, he goes to each patient’s bedside and evaluates the charting from the previous day and current documentation. He looks at the lab results, recent orders and compares them to the charting. If it took a few hours to implement an order, he discusses with the nurse the delay in the time and has the nurse critically evaluate the benefit of the order as it relates to the patient. Through caring practice, he also looks at environmental factors and how they can affect the patient and their diagnosis and works with the nurse or nurse tech to have them critically think about other cues that can affect their patient care as well as creating a compassionate and 8 CLINICAL GUIDED JOURNAL 1 therapeutic environment aimed at promoting comfort and preventing suffering. Therefore, through his clinical judgment and clinical evaluation he challenges his team to further understand treatment, interventions and outcomes. Working together with the healthcare team is another way that my preceptor takes his educator role and transforms it into a CNS intervention. Steve works hard at recognizing a need and developing an intervention to more effectively provide best care. This past year, Steve recognized that the nurses had a difficult time recognizing what actions to take with patients diagnosed with Subarachnoid Hemorrhages (SAH) when patient has not met the orders and parameters set by the medical team. He recognized a delay in care which affects patient outcomes. He therefore performed a literature review of the management of SAH, what interventions were performed when typical parameters were not met, collaborated with the ICU, Neurology and Neurosurgery teams and developed an algorithm and a more specific physician order set in the treatment of patients with SAH. The orders and algorithm enabled nurses to make quicker decisions and implementations when their patient’s condition changed or did not follow the typical presentation. Just recently, we saw a preceptor grab the algorithm and show her new graduate nurse the interventions she can implement in her care of the patient with an abnormal presentation of SAH. Steve saw a problem, worked with the entire medical team, and together they developed a specific plan to direct their nurses and staff in the evaluation and treatment of their patient. Systems thinking is another value that Steve utilizes in his practice of a CNS as he recognizes the relationships that exist within and across the health care system. A one of his job expectations and evaluation criteria, Steve participates in several committees. Steve steps above and beyond his evaluation responsibility to provide CNS quality implementations. As a participant and member of the Medication Operation Subcommittee, Steve is the nursing liaison to a pharmacy driven committee that includes nurses, physicians, and pharmacists to enhance the safety, proficiency and communication through GUH 9 CLINICAL GUIDED JOURNAL 1 to facilitate fast and effective medication administration. Steve is able to collaborate with all disciplines to evaluate the strengths and benefits of communication, evaluate the needs assessment and plan of pharmacy change according to hospital standards. Another committee Steve participates on is the Stroke Code Response Committee where he helps to evaluate the response of interventions at GUH through ER admission to discharge. As a CNS, he is able to help the team evaluate the results of the medical management through time it takes to implement a specific intervention, type of treatment, days of inpatient care and total outcomes. This data is compared to national standards and best evidence base practice. Even as a participant as an educator in the nursing critical care and educator meeting, Steve implements his systems thinking and CNS role by challenging his team during the discussion if VAP. He mentioned that even though we as a hospital have decreased our rates in VAP, there is an increase in the rates of bacterial colonization in the oral cavity of our ventilated patients. Therefore, this is concern should be addressed as we continue to evaluate the changes in oral care and patient care goals through recent literature and critical care needs. Through the examples described, Steve sets the example of being a facilitator of learning for his patients, staff and system. I think that this characteristic is easily liked through the use of clinical inquiry and systems thinking to bring knowledge and the most recent evidence to practice. As a educator, it is important to teach your team how to do something and validate a skill, but the CNS facilitates this learning through critical thinking, evidence and expansion of knowledge behind that skill to make a difference in our care. The two remaining characteristics are three very important traits of the CNS, but I am only beginning to understand how my preceptor uses them in practice. I understand that moral advocacy is the CNS trait that shows how they advocate for the concerns of patients and families as well as identifying and resolving ethical concerns. During my specific clinical days, I personally have not seen my preceptor 10 CLINICAL GUIDED JOURNAL 1 sit down and validate patient or family concerns and at this time, there really have not been any ethical concerns with our patients. I do know that when present, my preceptor would help clarify concerns and collaborate with the team to address the concerns in a safe and therapeutic manner. Likewise, responding to diversity, Steve is a caring and open APN who addresses his patients to incorporate sensitivity and recognizes differences when providing care. Working with any patient, Steve does go above and beyond to make sure that individual preferences are met and recognizes that each patient needs individualized care. While acting as a CNS and having the liberty and support from his team to use his role as the APN to develop interventions in the NSICU, the main barrier to the CNS at Georgetown University Hospital is the knowledge deficit of the role of the CNS. Since the hospital does not support the CNS position as a specific job, Steve has to use his CNS role as an expansion off the educator role. While on the floor, even after implementing CNS interventions, Steve says that he is still viewed as solely the educator, staff does not understand that these actions are CNS driven, which is very different than an educator intervention, and when working with staff and families, is introduced to the as the Clinical Educator, not CNS. Even when working with patients and their families and introducing himself as a CNS, Steve states that he often gets questioned about what that means and how he is involved in their care. Steve stated that the two roles he has (educator and CNS) should be two separate jobs for the enhancement of care and practice at GUH. It is necessary for the educator to be responsible for staff training and the new graduate nursing education while the CNS takes the best evidence and CNS characteristics and provides it to the multidisciplinary team. Through the evaluation of the job Clinical Educator job description, the Synergy Model and the actions of my preceptor in the clinical setting, there is a need for the CNS in the clinical setting. Without CNS influence on the NSICU, the setting and practice guidelines would be very different.