Dermatologic Emergencies - Calgary Emergency Medicine
advertisement

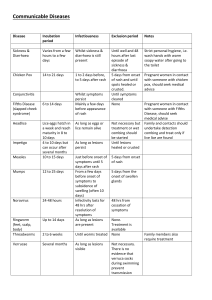
Dermatologic Emergencies History It is important to establish the onset of the first lesion. The location and description of the first lesion may be helpful in determining the cause of the rash. Then the pattern and distribution of subsequent lesions should be established. Are the lesions transient, do they migrate? It is also important to ask about blisters, vesicles, discharge, ulcerated and weeping areas. It is also important to determine whether or not the rash is itchy. This can be followed by a general medical history followed by exposures, travel, sexual history and immunization history. Finally, enquire about meds including otc and alternative meds and allergies Physical Exam Assess vitals Examine the rash: examine in good light, disrobe patient Distribution: Generalized vs Localized Generalized rashes: usually secondary to internal/systemic exposuredrugs, viruses Localized: local exposure (however some systemic illnesses manifest as local rashes i.e. lupus, HSP) Pattern- location, symmetry, configuration Anatomical location – scalp, face, mouth, trunk, axilla, perineum, limbs, palms and soles Symmetry (systemic exposure) vs Asymmetry (local exposure) Configuration – relationship of lesion to other lesions Types of Primary lesions Macule flat circumscribed discolored lesion <1cm Patch flat, circumscribed discolored lesion >1cm Purpura flat non-blanching discoloration of skin Abscess tender erythematous fluctuant nodule Nodule raised palpable solid nodule <1cm Tumor raised palpable solid nodule >1cm Wheal transient edematous papule/plaque w/ erythema Vesicle thin walled circumscribed blister <5mm Bulla thin walled circumscribed blister >5mm Pustule vesicle with pus Papule raised solid palpable lesion < 1cm Plaque raised solid palpable lesion > 1cm Secondary lesions: scar, erosion, excoriation, fissure, ulcer, telangiectasia Diagnostic Tests- in Tintinalli but not that practical -KOH test- place lesion on slide with 20% KOH and examine for hyphae -Scabies and Lice- scrape specimen onto slide, add drop of mineral oil and examine under microscope -Tzanck smear: unroof blistering lesions (HSV) -Woods light: UV @ 365 nm : Erythrasma – red Tinea Versicolor – green/yellow GENERAL TREATMENT MEASURES 1) If its wet- dry it. If its dry, wet it 2) Oral steroids- urticaria, angioedema, toxicodendron dermatitis a. Use in caution in diabetes, PUD, immunodeficiency and some psychiatric disorders 3) Topical steroids – 7 groups based on vasoconstriction. Fluorinated are stronger, but avoid in pregnancy. Group 7 is weakest i.e. 1 and 2.5% hydrocortisone cream and group 1 is strongest i.e. betamethasone. clobetasol 4) Oral antihistamines 5)Antimicrobial agents – topical vs oral a. Antibacterial b. Antifungal- clotrimazole, miconazole, ketoconazole c. Antivirals – acyclovir d. Anti-infestation – premethrin, lindane (don’t use in small kids, may cause neurotoxicity) 10 Life Threatening and Serious Skin Disorders 1) ERYTHEMA MULTIFORME - Definition: hypersensitivity reaction with immunoglobulins and complement component deposition in the cutaneous microvascular. Spectrum of disease: minor (localized papules) to major (generalized vesiculobullous lesions and mucous membrane erosions) Who gets it: More common in males, most common age 20-40 What causes it:1) Idiopathic 2) Infections: Viral- many viruses but HSVI and II are most common, also many bacterial causes- mycoplasma pneumonia is most common 3) Drugs: antibiotics and anticonvulsants Prodrome of fever malaise, myalgia, arthralgias 1-2 weeks prior to onset. Skin burning Characteristic lesions: Maculopapular lesions, target lesions, vesiculobullous lesions on extensor surfaces and mucosal surfaces. Centripetal spread Minor- target lesions/ raised edematous papules, acral distribution Major- same as minor but 1 or more mucous membranes involved. Epidermal detachment usually less than < 10% TBSA. Mucous membrane involvement usually oral and usually not as severe as SJS/TEN Complications: fluid and electrolyte imbalances, secondary infections Treatment 1) Short course of prednisone 60-80mg 2) Analgesics 3) Antihistamines 4) Antibiotics May require ICU Close to 0% mortality with resolution at 2-4 weeks without consequence 2) Toxic Epidermal Necrolysis/SJS Similar etiology and prodrome as EM but more likely drug related, more mucous membrane involvement (eyes, esophagus, airway, ano/genital), more likely to have central lesions, with more hemorrhagic bullae. Histiologically differs from EM Who gets it: all ages, both genders What causes it: 1) Idiopathic, 1) Drugs antibiotics ( pcn, sulfa), anticonvulsants, oxicam/ NSAIDs, 2) Infections: Viral HSV and HIV, bacterial infections 3) Malignancies Characteristic Lesions: Warm tender erythematous skin progresses to vesicles, bullae with mucous membrane involvement and eventual exfoliation Nikolsky sign: touching skin adjacent to bullous lesion results in dislodgement of skin (epidermis from dermis). Large areas of denuded dermis SJS < 10%TBSA epidermal detachment, Between 10=30% BSA is considered overlapping SJS/TEN TEN > 30% TBSA epidermal detachment. Complications: Infection Hypovolemia Perilabial and airway sloughing Ocular involvement: conjunctivitis, conjunctival erosions, eye edema Management: ICU or Burn Unit burns protocol, IV rehydrate, remove offending agent. Consider IVIG and optho consult for eye involvement Mortality: SJS has 5% mortality, TEN 30% mortality 3) Exfoliative Dermatitis ( Erythroderma) Erythematous rash involving 90% of the skin that progresses to diffuse exfoliation Who gets it: all ages, more common in males ( 2:1) and age > 40 What causes it: 1) Preexisting skin disease (10-40%): eczema, psoriasis 2) Malignancies (10-40%)- lymphoma, leukemia, MML, carcinomas, paraneoplastic syndrome 3) Drugs (3-10%) 4) HIV 5) Idiopathic Characteristic Lesion: Warm erythematous skin. Initially burning and itching that progressives to generalized exfoliation. Complications: fluid loss, hypothermia, infections Management: withdraw offending agent, treat underlying condition, replace fluids. May need ICU or burn unit Mortality: 30% 4) Disseminated Gonococcal infection Disseminated gonococcal infections follow 1-2% of GU/mucosal infections with N gonorrhoeae. Joint pain ( arthritis/tenosynovitis) with a rash Who gets it: sexually active adults, more common in females What causes it: disseminated N gonorrhoeae infections Prodrome: Preceding mucosal infection followed by fever, arthralgia, tenosynovitis but may not be systemically unwell and primary infection likely absent by this time Characteristic Lesion: 5-40 lesions- multiple papular vesicular and pustular/hemorrhagic skin lesions on extensor surfaces of wrist, palms, ankles, feet. May be petechial w/ necrotic centres. Complications: septic arthritis ( knee most common), meningitis, endocarditis Treatment: Ceftriaxone Mortality: low 5)Meningococcemia Initially maculopapular or petechial rash that rapidly progresses to prupura, bullae,DIC, shock and death caused by Neisseria Meningitidis 6) Toxic Shock Syndrome Severe syndrome with high fever, diffuse erythroderma, mucousmembrane hyperemia, pharyngitis, GI upset associated with staph infection. Similar but rarer STSS (Strep Toxic Shock Syndrome assoc with GAS) Major criteria Fever: temperature >38.9°C (102°F) Rash: diffuse macular erythroderma (sun burn) followed by desquamation: 1 to 2 wk after onset of illness, particularly of palms and soles. Hypotension: systolic blood pressure <90 mm Hg for adults or <5th percentile by age for children <16 yr of age, or orthostatic syncope, orthostatic drop > 15mmHg Mucous membrane hyperemia Multisystem organ failure- 3 other systems: MSK, GI, Renal failure, ARDS, CNS Who gets it: More common in women (90%) but can effect all ages. What causes it: Staph infections that produce the exotoxin TSST-1 Previously more common in tampon users. Menstrual related TSS remains somewhat common. Other causes include diaphragms, sponges, nasal packing, body piercing, post op Prodrome: malaise, myalgia, headache, n&v, diarrhea. Complications: numerous Treatment Stabilise and remove potential sources of infection anti-staph agents suggested but do not alter course of disease (decrease recurrences) 7) Staph Scalded Skin Syndrome Staph producing exotoxin (exfoliatin) that cleaves skin within epidermis. More superficial then TEN Who gets it: mostly kids under 5 What causes it: staph exotoxins Prodrome: clinically occult staph infection of eyes, naso pharynx or umbilicus Characteristic lesions: Begins around the mouth and leads to erythematous skin (stage 1) followed by exfoliation (stage 2, day 2) and with desquamation and bullae (stage 3 on days 3-5). Nikolksy positive Treatment: Penicillinase resistant antibiotic (Clox or Vanco), fluid replacement 8) Bullous disease Pemphigus Vulgaris- generalized mucocutaneous autoimmune blistering eruption. Begins as clear flaccid fragile blisters. Nikolsky positive. Autoimmune reactio to desmolgein- glue that holds epidermal cells together 95% mucous membrane involvement Who gets it: ages 40-60 but can occur in all ages Treatment- fluid and steroids Bullous pemphigoid- More benign and usually self limited, disease of elderly deeper into dermis therefore blisters are more tense and larger. May begin as hives. Autoimmune reaction to collagen Who gets it: mostly elderly Treatment- fluid and steroids, minocycline or tetracycline, immunosuppresors if severe Pemphigoid Gestationalis- associated with pregnancy 9) Rocky Mountain Spotted Fever Tick born bacteria Rickettsia ricketsii, potentially fatal multisystem disease from necrotizing vasculitis Who gets it: all ages, more common on East Coast What causes it: see above. People in close proximity to deer, cattle, pets, rodents Prodrome: constitutional symptoms up to 1 week after exposure. Classic triad is fever, rash with tick exposure Characteristic lesion: discrete maculopapular blanchable lesions that first appear on wrist and ankles. Evolves into petechiae Complications: hepatosplenomegally, meningismus, renal and hepatic failure, myocarditis. 50% mortality if untreated Treatment: doxy 10)Angioedema Well-circumscribed areas of edema caused by increased vascular permeability. Usually presents as acute swelling of face, extremities or genitals. Also may have abdo pain and airway compromise Who gets it: all ages What Causes it: 1)Meds- AceI, pcn, NSAIDs, contrast material 2)Food allergens 3)Physical agents- trauma, friction, cold 4) C1 Esterase Inhibitor Deficiency- low levels of C1-INH a) hereditary ( autosomal dominant) b) acquired ( autoimmune disorders and B cell malignancies) Complications: airway compromise, unnecessary abdominal surgeries, peripheral edema. To assess for airway compromise in these patients, watch for difficulty swallowing secretions and a change in voice. Peripheral edema is not pitting, non erythematous and no hives. Usually unilateral and may be associated with minor trauma. Treatment If you can’t distinguish between this and anaphylaxis- treat for anaphylaxis Antifibrinolytics (Amicar)- for acquired only Anabolic androgens ( danasol)- increase C1- INH Plasma derived C1-INH (Berinert)- self-administered FFP if Berinert not available Infestations 1) Scabies Definition: itchy polymorphic rash commonly of hands and feet Who gets it: Common in children, low SES, immunocompromised What causes it: Sarcoptes Scabiei T Prodrome: takes 3 weeks from infection to onset of symptoms Characteristic lesion: burrow- red linear line or S shaped with central scale a. Crusted scabies: large mite burden leading to less itchy but thick hyperkeratosis of hands and feet. Highly contagious Treatment: premethrin 5 % or lindane 1% lotion left on overnight, wash clothes in hot water, treat contacts and repeat treatment in 1 week 2) Lice Definition: pediculosis capitis = head lice, pediculosis corporis = body lice, pediculosis pubis = crabs) Who gets it: same as scabies What causes it: see above Prodrome: Itchiness in affected area Characteristic lesion: white nits in hair, may see lice clinging to hair shafts near scalp Ova or nits are adherent to hair shaft and if > 1cm from skin, have likely hatched (need to remain close to scalp because they feed off blood) Treatment: Nix (premethrin 1%) rinse for 10 min, nits can be removed with 50% vinegar solution applied to hair followed by combing with fine toothed comb Rashes of Groin Tinea Cruris (Jock itch) Definition: Fungal rash involving the groin Who gets it: all ages, more common in males Characteristic lesion: erythema with slightly raised scaly edge, may extend to thighs but spares the penis and scrotum Treatment: topical antifungal i.e. clotrimazole, ketoconazole. Consider polysporin to prevent bacteria super infection. Spectazole has antifungal and antibacterial properties. May require oral antifungals Erythrasma Infection caused by Corynebacterium minutissimum. Commonly in groin. Treated with erythromycin. Will illuminate with woods lamp Rashes on Face and Scalp Erysipelas and cellulitis– hot red rash on face. Erysipelas more superficial then cellulitis. Caused by GAS and staph Treatment: Keflex Herpes Simplex I- cold sores (herpes labialis). Treatment antiviral or antiviral ointment ( penciclovir, Zovirax) Herpes Zoster May involve any of the branches of the trigeminal nerve. V1 (ophthalmic branch) with lesions of nose (Hutchinson’s sign) may have associated keratitis. Keratitis responds to ocular steroids. May also cause Ramsay Hunt syndrome (lesions in auditory canal) or Bell’s Palsy. Treatment: antivirals (acyclovir 800mg po 5/day for 1 week, Valtrex 1 g po tid x 1 week, famvir 500mg po tid x 1 week. Refer to ophthalmology if needed Lupus- discoid or malar rash Tinea Capitus Superficial infection caused by dermatophytes Annular configuration with erythema and scaling Treated with antifungals If not improving think secondary infection Rashes of Skin Folds Candida Intertrigo Bright red rash with satellite papules and pustules moist chronically occluded areas. Predisposing factors include antibiotics (topical or oral), steroids, immunocompromised states, obesity. Non infectious intertrigo may also be a result of irritation from moisture, heat and friction. Urine and Feces may also cause non infectious intertrigo Diagnosis: KOH slide prep Treatment Topical antifungals, drying agents (Zeasorb AG), astringent agents (Burow solution), keep the area dry Rashes of lower extremities Lichen Simplex Chronicus Itchy well demarcated hyperpigmented plaques. Affects ankles, shins and feet. May also affect groin. Need to rule out fungal infections Treatment; stop the itch and high potency steroids. Warn pt that it will take a long time to go away Erythema Nodosum Inflammatory eruption of subcutaneous fat (panniculitis) Tends to affect the shins Poorly demarcated warm erythematous nodules Multiple etiologies –NODOSUM NO- no obvious cause (idiopathic) most common D- drugs sulfonamides, ocp, penicillin, vaccines, bromide O- oral contraceptive pill, pregnancy S- sarcoidosis U- ulcerative colitis (IBS), Behcet Disease M- microbiology Bacterial – strep, campy, yersinia, TB, leprosy Fungal- Blastomycosis, coccidiomycosis, histoplasmosis Viral- HSV, Mono Parasites- Leishmaniasis, toxoplasmosis Management: CBC, blood cultures, throat swab if symptomatic, urine HCG, CXR for sarcoid. Should resolve on own.