Click here to the handout
advertisement

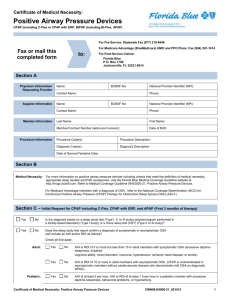
Obstructive sleep apnoea Dr. Wong Ka Chun Specialist in Respiratory Medicine Predisposing Factors 1. Age – increases with age and plateau off at 60-70 2. Sex – male and postmenopausal female 3. Obesity 4. Craniofacial and upper airway abnormalities, it is well recognized in Asian patients. Examples are abnormal maxillary or short mandibular size, a wide craniofacial base, tonsillar hypertrophy, and adenoid hypertrophy. 5. Other factors - nasal congestion, pregnancy, heart failure, COPD, CVA, acromegaly, hypothyroidism. Pathophysiology of obstructive sleep apnoea Recurrent collapse of the pharyngeal airway during sleep (related to narrowed airway ), results in 1. reduced or complete cessation of airflow despite ongoing breathing efforts. 2. leads to intermittent disturbances in gas exchange (eg, hypercapnia and hypoxemia) and fragmented sleep. Symptoms/Impact on patient and his/her bed partner 1. Excessive daytime sleepiness -> impair daily function, induce or exacerbate cognitive deficits, and increase the likelihood of errors and accidents (e.g. traffic accident) 2. Snoring, usually habitual 3. Witnessed apnoea “cessation of breathing”, noticed by bed partner 4. Others- nocturia, fatigue, poor concentration, nocturnal angina, morning headaches, Sexual dysfunction (impotence and decreased libido) Examination Obesity, craniofacial and upper airway abnormalities ( such as small mandible, tonsil enlargement, redundant soft palate) Impact on patient’s health OSA is associated with hypertension, coronary heart disease, atrial fibrillation and other rhythm disturbances, heart failure, stroke, diabetes and metabolic syndrome. Sleep study 1. A Sleep study is necessary to accurately diagnose OSA and to assess treatment benefit. Data are collected in the laboratory in the presence of a qualified technician 2. Out-of-center sleep testing/home sleep study may be an acceptable alternative for patients who are strongly suspected of having OSA and who do not have medical comorbidities (eg, heart failure) that increase the risk for additional or alternative sleep related breathing disorders. What a sleep study will tell? RDI (Respiratory distress index) the number of obstructive apneas, obstructive hypopneas, and respiratory effort related arousals (RERAs) per hour of sleep. The American Academy of Sleep Medicine (AASM) recommends consider CPAP when 1. RDI ≥15 events per hour with or without symptoms, or 2. RDI between 5 and 14 events per hour that is accompanied by any of the followingi. symptoms: sleepiness, nonrestorative sleep, fatigue, or insomnia symptoms; waking up with breath holding, gasping, or choking; habitual ii. snoring and/or breathing interruptions; or co-morbidities -hypertension, mood disorder, cognitive dysfunction, coronary artery disease, stroke, congestive heart failure, atrial fibrillation, or type 2 diabetes. Treatment 1. Behavior modification - Weight reduction, exercising, changing the sleep position (if OSA is positional), abstaining from alcohol, and avoiding certain medications (such as hypnotic.) 2. CPAP (continuous positive airway pressure) provides a pneumatic splint, with positive pressure, usually via an airtight nasal mask, that keeps the upper airway 3. 4. open. Intolerance/poor acceptance/poor compliance of CPAP is the major obstacle to the use of CPAP, and is very common. The key to success of CPAP is good communication/explanation. Common problems with CPAP are discomfort with nasal mask, air-leak, nasal stuffiness, dry nose/thorat, and air ingestion; Treating these problems helps improving compliance. Oral appliance – is a good alternative for mild to moderate cases. It works by holding the soft tissues of the oropharynx away from the posterior pharyngeal wall, thereby maintaining upper airway patency. Surgery – reserved for cases failed CPAP/oral appliance