Surgery, Autumn Term 2013 Question 1. - Ping-Pong
advertisement

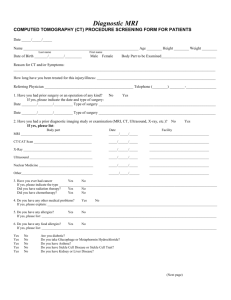
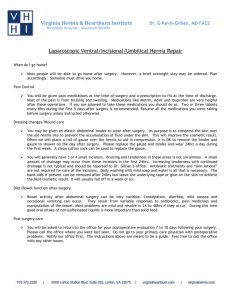
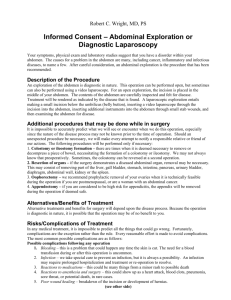
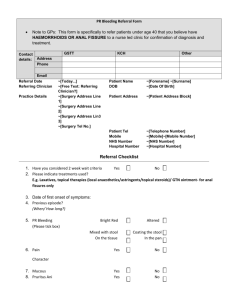
Surgery, Autumn Term 2013 Question 1. A 35-year-old woman, who has been suffering from constipation for many years, comes to the emergency ward because she has noticed red blood in her stools during the last three days. In addition, she has developed a continuous anal pain which is accentuated by defecation. In the days before the bleeding started she had an episode of constipation. You read the following notes in her medical file on arrival: normal temperature, haemoglobin 120, blood pressure 125/70, pulse 70. 1A. Which are the two most common diagnoses causing her symptoms? (1p) Haemorrhoids and anal fissure How should you manage this case in the emergency unit? (3p) Medical history and clinical examination including visual assessment of anus. If possible digital rectal exam. If limited pain on exam, perform procto-rectoscopy. The limitation pain sets for the examination must be commented upon for receiving full score. Xyloproct ointment twice daily for about 14 days and stool softener such as Inolaxol. 1B. How must she be followed up? (2p) Procto-rectoscopy at the emergency unit or in primary health care. If no certainty in detecting the source of bleeding – low threshold for referral to colonoscopy. Anal cancer is an uncommon diagnosis, but it is important to know that anal cancer, too, may give the above described symptoms. 1C. What cell type does anal cancer originate from and how is it treated primarily? (1p) Squamous epithelium / radiotherapy Question 2. Gastric bypass (GBP) surgery is the most common surgical intervention in Sweden to achieve weight loss. Two years after GBP surgery, a woman comes to the emergency unit with intermittent abdominal pain and vomiting. She has lost 35 kilos since the operation. You note that her abdomen is not extended and you can hear sparse bowel sounds. The abdomen is soft on palpation, with left-sided tenderness. You find no signs of peritoneal irritation. 2A. What do you suspect and which mechanism has probably caused the condition? (1p) Ileus due to internal hernia 2B. Which examination do you request? (1p) Computed tomography with oral and intravenous contrast. 2C. How must this be treated? (1p) Surgery for closure of the internal aperture Question 3. You meet a 49-year-old man at the emergency unit who has come because of abdominal pain. He reports that the pain started suddenly about four hours ago. It has been on a constant level since then but is accentuated by deep breaths and movement. He indicates the upper abdomen as the point of maximal pain. On examination you observe: General condition: Orientated regarding time, place and person, slightly pale face, sweaty, some odour of alcohol, breathing rate 24/min, saturation 92% on air, temperature 37.4, GCS 15. Heart: blood pressure 100/50, pulse 110, otherwise without abnormalities. Lung auscultation: mild crackles in basal parts on both sides Abdomen: some overweight, no bowel sounds, marked tenderness on palpation in upper abdomen, generalised peritonitis, no palpable lumps. 3A. Describe management regarding laboratory tests, prescriptions and measures both at the emergency unit and further management after hospital admission. Justify your answer! (6p) Blood tests including glucose levels, blood cell counts, CRP, liver enzymes including pancreatic amylase in order to differentiate from pancreatitis, ABO typing and back typing considering possible surgery, and possibly blood gas considering the patient’s affected general condition. Pain relief (opioids) intravenously, rapid infusion of Ringer’s acetate (for stabilisation) and gastric tube. After stabilisation, CT abdomen/CT abdominal overview should be performed (1p) and the patient planned for urgent surgery. The preoperative prescription of a first dose of antibiotics (Ciproxin+Flagyl or Tazocin) is not wrong. In addition, further intravenous fluids and pain relief with intravenous opioids on demand should be prescribed until surgery. 3B. Which are the two most probable differential diagnoses? (2p) Perforated ulcer (right answer). Pancreatitis and perforated diverticulitis are also plausible. Question 4. As the surgeon on call at a district hospital you are alerted that a 63-year-old is on his way to the emergency room by ambulance. His severe abdominal pain started about one hour ago. In the emergency room you meet a man with substantial persistent pain without fluctuation in intensity. He is in cold sweats and pale and his skin feels sticky. The following parameters are registered: breathing frequency 30, saturation 93% on air, pulse rate 110, systolic blood pressure 110. On abdominal examination you note a pulsating mass. 4A. Describe and justify your management of this patient in the emergency room (4p). The answer should contain blood tests including haemoglobin, electrolytes and creatinine, ABO and back typing. The insertion of two large-calibre intravenous lines to which crystalloid fluids are connected (0.5 p), one litre per line. These must only drip slowly as the systolic blood pressure is adequate or even slightly too high (which should be mentioned). The patient must receive pain relief with intravenous opioids. The senior surgeon and/or vascular surgeon on call and the anaesthetist on call must be contacted. Discussion regarding the choice of two adequate measures: open surgery or endovascular intervention (EVAR). Considering the fact that the patient is stable, a CT must be considered. Despite your efforts the patient deteriorates further and the pulse rate rises to 140 per minute while blood pressure sinks to unmeasurable levels. 4B. What has happened and what is your reaction/measure? (2p) The aneurysm has ruptured into the peritoneal cavity. The patient must urgently be taken to the operating theatre. 4C. Summarily describe risk factors for aneurysm development! (2p) The answer should contain at least two risk factors (hereditary risk, smoking, atherosclerosis, hypertension, age, inflammation, bacterial infection of the aortic wall) Question 5. A 40-year-old man arrives at the emergency unit with a painful mass in his right groin which appeared when moving a sofa four hours ago. The pain has increased since its debut. 5A. What do you suspect? (1p) Incarcerated inguinal hernia 5B. How should you manage the patient? Justify! (3p) Take blood tests which should include blood cell counts, CRP, fluid balance, ABO and back typing. Insertion of an intravenous line and administration of Ringer’s acetate. Pain relief with intravenous opioids and possibly benzodiazepine, thereafter attempt to reduce the hernia. Nil per mouth and hospital admission, regardless whether the hernia has been reduced or not, considering potential bowel injury by incarceration. Surgery if non-reducible hernia, otherwise observation. CT abdominal overview should as a matter of principle not be performed in non-reducible hernia as it delays management.