Amyloidosis
advertisement

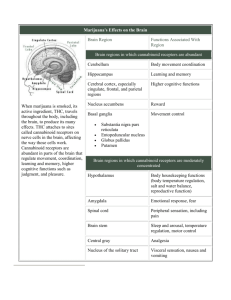
Frequently asked Questions Pathological Anatomy and Physiology Exam – 3rd year Q: Disorders of cell membrane signaling (receptors and membrane channels) and its consequences. A: Question is similar to “Pathophysiology of signal transmission” and part of “Pathophysiology of receptors in the endocrine system” Start with Physiology: Signal is transmitted in various systems (neural, immune, and endocrine) Where are receptors located? (e.g., neuro: presynaptically, postsynaptically; in endocrine: on membranes, in cytoplasm, in the nucleus, etc.) What is the mechanism of signal transport? (e.g., channels) Pathophysiology: The receptors can be influenced by various substances or processes (see slide below – it is for endocrine system – all these situation change membrane signaling): (age, antibodies (inflammation), etc.) Consequences: sensitivity changes (especially insulin), change of function (may be increased or decreased: i.e. by antibodies (agonistic effect of Ab in Graves Basedow, destruction of receptors in myasthenia gravis, block of receptors in myasthenic syndrome) 1 Level of failure Receptors The presence of other substances acting on receptors Mechanism Genetics (increased or decreased amount) Example Decreased amount of receptors for ADH in kidneys (inherited Diabetes Insipidus) Sy of testicular feminization Genetics – decreased sensitivity of Laron dwarfism (receptors for receptors somatomedins) Damage (most often by Ab ) Myasthenia gravis Age Sensitivity of rec. In tumors (ca mammae) Obesity - amount (and also sensitivity) Up and down regulation of insulin receptors Stimulating Ab Binding to TSH rec.- Basedow’s disease Asthma bronchiale (Ab block β Inhibitors Ab adrenergic rec) Myasthenia gravis (block Agonists Amphetamine (Agonist of dopamine) Block trypsin receptors - secretion of Antagonists CCK – hypertrophy of pancreas Grow hormone – galactorrhea in acromegaly Hormone spillover Insulin – hyperandrogenemia Cortisol – mineralocorticoid effect Q: Disorders of regulatory mechanisms in the endocrine system A: Start with physiology: what is necessary for normal hormonal regulation, types of feedback, example of hormones regulation by simple or complex feedbacks? The failure of regulation might be due to adenoma (overproduction without regulation possibility), failure of receptors (normal secretion, no action), failure of channels, G proteins, protein synthesis, i.e. in decreased amount of substrates due to malabsorption, etc. Q: Disorders of the hormonal and nervous control in GIT A: Start with physiology: describe the enteric nervous system, local hormones (from gastrin to motilin, cholecystokinin, secretin, somatostatin or VIP), influences of sympathetic and parasympathetic nervous systems, reflexes. Do not forget the effect of increased thyroid hormones (which increase motility) and aldosterone (increases reabsorption of water in the large intestine). Briefly overview, name the disorders and choose one to describe. The most often consequences of dysregulation in GIT are constipation and diarrhea Acute diarrhea leads to dehydration, loss of ions, metabolic acidosis; chronic – to malabsorption sy. Q: Endocrine causes of mineral metabolism disturbances A: You can speak about aldosterone that regulates metabolism of sodium, however, be aware, that it does not change its concentration (one molecule of sodium binds osmotically to one molecule of water). But aldosterone leads to excretion of potassium in the kidneys. 2 ADH (from the posterior pituitary) increases “free” water retention, thus increased ADH (i.e. in SIADH) decreases concentration (dilutes) all ions but the total amount in the body remains the same. Decreased secretion of ADH (diabetes insipidus) leads to increased concentrations of ions. Depending on the cause of secretion changes of these hormones, different consequences develop. Describe cause>consequence Remember: glucocorticoids in overproduction have mineralocorticoid effect. You can speak also about calcium metabolism and its regulation (PTH, calcitonin, calcitriol). Q: Endothelial dysfunction A: Endothelial cells synthesize and release various factors that regulate angiogenesis, inflammatory responses, hemostasis, as well as vascular tone and permeability. Endothelial dysfunction has been associated with a number of pathophysiological processes. Oxidative stress appears to be a common denominator underlying endothelial dysfunction in cardiovascular diseases. However, additional factors such as age, sex, salt intake, cholesterolemia, glycemia, smoking, hypertension and hyperhomocysteinemia are the mechanisms underlying the endothelial dysfunction. Consequences: hypertension (vasoconstriction due to increased endothelin or decreased NO production), atherosclerosis (due to increased adhesive molecules and pro-inflammatory changes in the endoth. cells), formation of thrombi (due to decreased smoothness of the vessels). Consequences for the organism: hypertension, ictus, lung embolism, ICHS, heart failure... Q: Changes in compliance in individual organs A: Changes of compliance can be seen in the following organs: lungs and chest, heart, blood vessels, urinary bladder, etc. The common causes of the changes (decreased compliance) are fibrotisation (e.g., scaring after MI), inflammation, in vessels it is atherosclerosis and applicable for all organs is physiological aging. The consequences are changed functions. Q: Inborn of defects of glycogen metabolism A: This is a question from pathology. Be aware: diabetes mellitus is a disease of glucose metabolism, not glycogen, so as galactose. Q: Pathophysiology of mineral metabolism (Ca, P) As to phosphate changes – increase: most often in kidney failure, consequence – decreased calcium => as feedback increase in PTH secretion and therefore osteoporosis, calcifications, etc. 3 – decrease: caused by high PTH (increases excretion), low calcitriol (no resorbtion of phosphates in the gut) and phosphate diabetes (loss of phosphate in urine due to failure in transport mechanism). Consequences: osteomalacia, decreased body metabolism, fatigue (decreased ATP synthesis) Regulation together with calcium: calcitriol increases Ca and P; PTH increases Ca, decreases P. Q: Pathophysiology of receptors in the endocrine system A: Start with physiology: where receptors in endocrine system are located (on membranes, in cytoplasm, in the nucleus...) What substances or processes might affect them (age, antibodies (inflammation)...), up- and down-regulation, consequences: sensitivity changes (especially insulin), autoimmune affection by Ab with agonistic effect (Graves Basedow), etc. Q: Role of glucocorticoids in the pathologic states A: Start with physiology: where it is produced, how its production is regulated and when the production increases and what are the effects. Talk about stress, Addison´s, Cushing´s (note: Cushing´s sy x Cushing´s disease). Do not forget the effects on bones (osteoporosis), inflammation, blood pressure and so on. Q: Smooth muscle dysfunction A: Physiology: what are the characteristics of smooth muscles; their regulation (autonomic nervous system, influence of ions, necessity of extracellular calcium for the contraction, own nervous system in GIT, bladder). Important characteristics are compliance and elasticity. Pathophysiology: changes of GIT motility (esophageal achalasia, decreased frequency of stomach emptying in diabetic patients (failure of autonomic nervous system), obstipation – e.g., ileus with colicky pain; increased motility – diarrhea; Hirschsprung’s disease. Vessels – hypertension; ureters – obstruction by calculi – colicky pain; urinary bladder – disorders of emptying with decreased compliance or elastance. 4