Polycythemia Literature Review Spring 14
advertisement

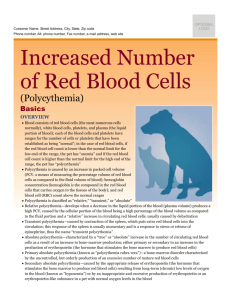
Running head: POLYCYTHEMIA Polycythemia: A Review of Recent Literature Liane Chlus and Christina Riggall State University of New York Institute of Technology 1 POLYCYTHEMIA 2 Polycythemia Polycythemia is a chronic condition that occurs when the body produces too many red blood cells, this in turn causes the blood to become thicker resulting in complications over time (National Heart, Lung and Blood Institute [NHLBI], 2011). There are two types of polycythemia, primary (polycythemia vera) and secondary. Polycythemia vera (PV) is caused by a genetic mutation of the JAK2 V617F gene; secondary is caused by chronic low levels of oxygen (NHLBI, 2011). Treatment of PV is continuing to be studied. Current treatment modalities for primary polycythemia include therapeutic phlebotomy, medications, radiation, and symptomatic treatments. Treatment of secondary polycythemia is based upon managing the underlying cause or lifestyle modifications (Antle, 2010). The focus of this literature review is to explore what the hematocrit goal should be; the current treatments to reach this goal, how to reduce the risk of complications from polycythemia vera and future treatment options. The goal of treatment for polycythemia is to reduce the risk of complications. Complications from polycythemia vera include thrombosis, splenomegaly, puritis, peptic ulcers, or progression to other diseases such as acute leukemia, myelofibrosis or myelodysplastic syndrome (Mayo Clinic Staff, 2014). The family practitioner may initially obtain a complete blood count that may have an elevated hematocrit, hemoglobin, red blood cells or platelet levels. Passamonti (2012a) recommends performing an erythropoietin (EPO) level to differentiate between secondary polycythemia and primary polycythemia vera. In polycythemia vera, the EPO level will be low and in secondary the level will be high (Passamonti, 2012a). Referral to a Hematologist should be ordered for possible bone marrow aspiration and treatment recommendations (Mayo Clinic Staff, 2014). POLYCYTHEMIA 3 Methods The State University of New York Institute of Technology's library database was used to find articles for this literature review. Databases included CINHAL Plus, MEDLINE Plus and Health Source: Nursing/Academic Edition. The Google search engine was used for general internet resources. Search terms included: Polycythemia vera, therapeutic phlebotomy, target hematocrit for polycythemia, treatments for polycythemia, thrombosis, management of polycythemia and JAK2 inhibitors. Through the internet source, national organizations were searched to obtain reputable information on the topic and similar search terms were used. The search was limited to peer-reviewed articles published within the last five years. This literature review included ten articles focused on treatment goals and therapies for polycythemia. Many of the large-scale studies that were found on the topic were over five years old. Several of the studies or articles that were included in our review mention these earlier studies on polycythemia vera. Secondary polycythemia was excluded from our literature review because the treatment is based upon treating the underlying cause. Results One of the main research questions studied was: What the target hematocrit (Hct) should be to reduce the risk of complications? The New England Journal of Medicine published an article by Marchioli et al. (2013) that studied JAK2 positive patients with polycythemia vera and their intensity of treatment. 365 adults were split into two group, a high hematocrit group (45-50%) and a low hematocrit group (<45%) (Marchioli, et al., 2013). The patients were treated with phlebotomy and/or hydroxyurea (HU) to maintain their hematocrit at these levels over time. All patients were treated with low dose aspirin unless contraindicated. The results from this study were that the patients in the high Hct group had a four times higher rate of death from POLYCYTHEMIA 4 cardiovascular problems than the low Hct group (Marchioli, et al., 2013). The number of participants was a limitation of this study. The researchers had initially set up to recruit around 1,000 patients but due to time constraints and lack of participation the study size was reduced (Marchioli, et al, 2013). According to a review by Barbui, Finazzi and Finazzi (2012), the recommended hematocrit for males should be less than 45% and for women less than 42%. Barbui et al. (2012) states that there are no controlled studies to date that adequately confirm higher hematocrit levels lead to more thrombotic events. The current recommendations from the American Society of Hematology are based upon the study from Marchiolo, et al. (2013) to aim treatment to maintain the hematocrit less than 45% (American Society of Hematology, 2013). The second research consideration identified was: How to maintain the hematocrit below 45% in patients with polycythemia vera? A review by Harrison (2010) suggested that the treatment should be based upon the cardiovascular risk group of the patient. According to Harrison (2010), high risk patients includes anyone over age 60, history of previous thrombosis, platelet count over 1000 x109/L, diabetes or hypertension requiring pharmacological management and significant or symptomatic splenomegaly. Significant splenomegaly was defined as the spleen being palpated 5cm below the costal margin (Harrison, 2010). Symptomatic splenomegaly was defined as early satiety or pain (Harrison, 2010). According to Harrison (2010), all patients with polycythemia vera should be treated with low-dose aspirin unless contraindicated. This article did not discuss phlebotomy as an option for maintaining hematocrit levels for low or high risk patients. High risk patients should be placed on either hydroxyurea (if over age 60), or Interferon (less than age 60) for first line treatment (Harrison, 2010). POLYCYTHEMIA 5 The third consideration for patients with PV was: What treatment regime is best for prevention of complications? In an article published in Blood Reviews, Barbui, et al. (2012) seem to take a less aggressive pharmacological management approach for treating polycythemia vera. Their first approach consideration is to educate the person on the disease and what modifying factors the patient can make in their lifestyle. For example, smoking was found to increase the risk of arterial thrombosis and therefore smoking cessation should be highly encouraged in patients with polycythemia vera (Barbui et al., 2012). In this article, Barbui et al. (2012) suggest the first treatment for high hematocrit associated with PV should be phlebotomy. This rapidly reduces the viscosity of the blood, thereby reducing the risk of thrombosis. Recommendations are to complete phlebotomy every other day until the goal hematocrit is reached (Barbui et al., 2012). This article also suggested that a low dose aspirin be given daily to prevent thrombosis (Barbui et al., 2012). For low risk patients, aspirin and phlebotomy were considered the first line treatments (Barbui et al., 2012). For high risk patients, hydroxyurea and interferon-alpha (INFa) were considered first-line drugs of choice to prevent thrombosis (Barbui et al., 2012). HU was also shown to reduce the incidence of myelofibrosis (Barbui et al., 2012). Effects of INF-a were a reduced need for phlebotomy (maintaining lower Hct levels), decrease in spleen size and decreased puritis (Barbui et al., 2012). Reikvam and Tiu (2012) also recommend modifying lifestyle factors to reduce the risk of arterial and venous thrombosis. Reikvam and Tiu (2012) recommended treatment of hyperlipidemia, exercise, smoking cessation, weight reduction, and treatment of hypertension to prevent thrombosis. Similarly to Barbui et al. (2012), Reikvam and Tiu (2012) suggest a low dose aspirin daily for all patients with polycythemia vera and hydroxyurea for patients with a history of thrombosis. One of the research gaps that this article POLYCYTHEMIA 6 mentioned was whether a history of venous thrombosis should be treated differently than a history of arterial thrombosis (Reikvam & Tiu, 2012). Individual hematologists may have their own recommendations for treating polycythemia vera. Passamonti (2012a) recommends a combination of lifestyle modification, antiplatelet therapy, cytoreduction and phlebotomy. Passamonti (2012a) discussed the research obtained from the Polycythemia Vera Study Group (PVSG) in 1997, a study that compared complications with phlebotomy versus hydroxyurea. The study found no significant differences in thrombotic events between the two groups. The hydroxyurea treated group developed more acute myeloid leukemia (AML) and the phlebotomy group developed more myelofibrosis (MF) (Passamonti, 2012a). Passamonti (2012a) argues that other studies have not shown the same results, and his recommendation is to discuss the possible risks associated with each of the treatments with the patient, so they are aware of the potential adverse effects. Similarly to the other recommendations, Passamonti (2012b) treats all of his patients diagnosed with PV a low dose aspirin unless contraindicated and prescribes hydroxyurea for patients with more than one risk factor for thrombosis. Clinical trials are being conducted on JAK-2 inhibitors in their efficacy in treating polycythemia vera and other myeloproliferative neoplasms. In the clinical trials that have been initiated, benefits from these medications include a reduction in spleen size, improved fatigue and a reduction in puritis (Apostolidou, Kantarjian, & Verstovsek, 2009). Side effects that have been reported are gastrointestinal disturbances, myelosuppression and neurotoxicity (Apostolidou et al., 2009). In 2011, the first JAK2 inhibitor was approved for use in the United States for treatment of myelofibrosis, which can be an evolution of polycythemia vera (McCall, 2013). An article by Hensley, Geyer, and Mesa (2013) suggests that JAK-2 inhibitors may POLYCYTHEMIA 7 actually slow the progression of the disease and recommends that further research be completed to test these new agents in comparison to the effects of hydroxyurea or interferon. Conclusion Multiple treatment modalities for polycythemia exist, and treatments need to be individualized for the patient's specific situation. Family Nurse Practitioners may collaborate with the Hematologist/Oncologist to manage the treatment regimen for these patients. The goal of treatment is to reduce the risk of thrombosis, reduce the risk of other complications and slow the progression of the disease. The literature that was reviewed recommended lifestyle modification and low dose aspirin for all patients with polycythemia, unless contraindicated. For secondary polycythemia treatment was geared towards the underlying cause of the disease. Primary treatments for polycythemia vera included aspirin, hydroxyurea, interferon-alpha and phlebotomy. Clinical trials are being completed to inhibit the JAK2 gene to reduce the risk of progression to myelofibrosis or acute leukemia. Current treatment modalities are effective at reducing the risk of thrombosis and mortality associated with this, but more studies need to be conducted to determine which treatments are the most successful. POLYCYTHEMIA 8 References American Society of Hematology. (2013). In polycythemia vera, 45 is the number. The Hematologist. Retrieved from http://www.hematology.org/Publications/ Hematologist/2013/9946.aspx Antle, E. (2010). Who Needs a Therapeutic Phlebotomy?. Clinical Journal Of Oncology Nursing, 14(6), 694-696. doi:10.1188/10.CJON.694-696 Apostolidou, E., Kantarjian, H., & Verstovsek, S. (2009). JAK2 inhibitors: A reality? A hope?. Clinical Lymphoma & Myeloma, 9S340-5. doi:10.3816/CLM.2009.s.033 Barbui, T., Finazzi, M., & Finazzi, G. (2012). Front-line therapy in polycythemia vera and essential thrombocythemia. Blood Reviews, 26(5), 205-211. doi:10.1016/j.blre.2012.06.002 Harrison, C. (2010). Rethinking disease definitions and therapeutic strategies in essential thrombocythemia and polycythemia vera. Hematology / The Education Program Of The American Society Of Hematology. American Society Of Hematology. Education Program, 2010129-134. doi:10.1182/asheducation-2010.1.129 Hensley, B., Geyer, H. & Mesa, R. (2013). Polycythemia vera: Current pharmacotherapy and future directions. Expert opinion, 14(5), 609-617. Marchioli, R., Finazzi, G., Specchia, G., Cacciola, R., Cavazzina, R., Cilloni, D., & ... Rapezzi, D. (2013). Cardiovascular Events and Intensity of Treatment in Polycythemia Vera. New England Journal Of Medicine, 368(1), 22-33. doi:10.1056/NEJMoa1208500 Mayo Clinic Staff. (2014). Diseases and conditions: Polycythemia vera. Retrieved from http://www.mayoclinic.org/diseases-conditions/polycythemiavera/basics/complications/con-20031013 POLYCYTHEMIA McCall, B. (2013). Second JAK2 Inhibitor for Myelofibrosis shows strong data. Medscape Medical News. Retrieved from http://www.medscape.com/viewarticle/806394 Moses, S. (2014). Polycythemia rubra vera. Family Practice Notebook. Retrieved from http://fpnotebook.com/HemeOnc/Marrow/PlycythmRbrVr.htm National Heart, Lung and Blood Institute. (2011). What is polycythemia vera? Retrieved from http://www.nhlbi.nih.gov/health/health-topics/topics/poly/ Passamonti, F. (2012a). How I treat polycythemia vera. Blood, 120(2), 275-284. doi:10.1182/blood-2012-02-366054 Passamonti, F. (2012b). How to manage polycythemia vera. Leukemia (08876924), 26(5), 870874. doi:10.1038/leu.2011.334 Reikvam, H., & Tiu, R. (2012). Venous thromboembolism in patients with essential thrombocythemia and polycythemia vera. Leukemia (08876924), 26(4), 563-571. doi:10.1038/leu.2011.314 9 POLYCYTHEMIA 10 Appendix A # Study Focus Subj ects 1 American Society of Hematology, (2013). Treatment goals N/A 2 Antle, E. (2010). Therapeutic phlebotomy N/A 3 Apostolidou, E., Kantarjian, H., & Verstovsek, S. (2009). JAK 2 Inhibitors 4 Barbui, et al (2012) Current therapies, high/low risk patients 5 Harrison, C. (2010) Indications for cryoreductive therapy, relieving disease related symptoms & minimizing risk of transformatio n to Population Age Methods Findings Pt's with PV Adults Reviewed the current recommendations and the literate that brought about the recommendation. Pt’s with PV N/A The importance of therapeutic phlebotomy in treatment of PV was discussed. JAK 2 + patient's with myeloprolifera tive neoplasms Adults Several clinical trials to determine the effectiveness of these new medications. N/A Pt’s with PV Lifesp an Review of current literature and treatment modalities and effectiveness was assessed N/A Pt's with PV Adults Review of current medications and future direction in treating PV. Discussed the findings of the Marchioli, 2013 study with the low vs. high Hct groups and the results from the study (See Marchioli et al, 2013). Phlebotomy can be used to treat PV and nurses should be aware of the reasoning behind this and monitor labs as needed. Clinical studies have shown a decrease in spleen size & puritis with the new medications. Side effects include GI disturbances & myelosupression Low-dose aspirin & phlebotomy is safe and effective at reducing the risk of thrombosis as 1st line tx. Hydroxyurea can be added to maintain Hct less than 45%. Treatment based upon patient's risk, discussed potential for JAK2 Inhibitors, may reduce splenomegaly and symptoms associated with PV. POLYCYTHEMIA 6 Hensley, Geyer & Mesa, (2013). 7 Marchioli, R., et al. (2013). 8 secondary myeloid malignancy Current pharmacothre rapy 11 N/A Pt's with PV N/A Reviewed the current medications available for the treatment of PV and the results of the studies that had been completed in the past. Determine which treatment intensity had better outcomes N= 365 Pt’s with JAK2 positive PCV Adults Pts were randomly assigned to a low or high Hct group. Median follow up was 31 months and adverse events were recorded. Passamonti, F (2012a) How he treats his pt’s with PV & problems encountered N/A Pt's with PV Adults & special popula tion Discussed diagnostic testing for determining secondary polycythemia vs. PV 9 Passamonti, F (2012b) Discusses case scenarios and current recommendat ions for treatment of PV N/A Pt's with PV Case studies of three patient s discuss ed Describe recommendations for treatment in each case and why 10 Reikvam, H., & Tiu, R. (2012). Manifestation s, treatment modalities and future directions N/A Patient's with DVT/PE related to PV Adultspecial popula tion discuss ed pregna nt female s Discussed treatment modalities for prophylaxis and treatment of DVT/PE such as phlebotomy, hydroxyurea, aspirin, Coumadin, JAK 2 inhibitors Current treatments were phlebotomy, aspirin & hydroxyurea. INFa and JAK 2 inhibitors still being studied but do show benefits. Those with a Hct less than 45% had a lower rate of CV death and thrombosis. *Current recommendation from the American Society of Hematology Explained his personal treatment of PV and reviews the previous studies that have been completed. Significant importance placed on the serum erythropoietin (EPO) level in aiding the diagnosis as well as family history. Discussed the pros and cons of each method. Recommended low-dose aspirin for all PV pt’s unless contraindicated.