Discussion on the contemporary management of tooth wear
advertisement

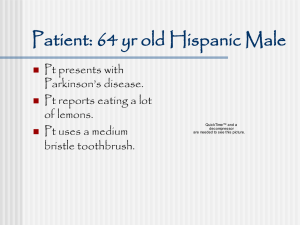
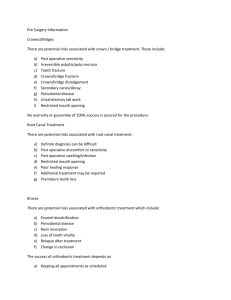
Discussion on the contemporary management of tooth wear 13/12/13 Student: Christopher Barley Student number: CDB275 Epidemiology Tooth wear is an increasing problem for the population on a whole. In the adult dental health survey of 2009, (1), it was found that moderate tooth wear had increased from 11% in 1998 to 15% in 2009. Although severe tooth wear is low, it is increasing and there are an increasing proportion of young adults with tooth wear. The percentage of tooth wear has been shown to increase markedly with age. In adults age 18-24, 52% showed some tooth wear compared with 95% of 75-84 year olds. Diagnosis/Measurement The diagnosis of tooth wear would be made clinically and has been measured historically with the use of stone models following impressions. The diagnostic process would include A full medical history Social/family history and any obvious areas of stress Diet analysis Full clinical examination Clinical features of erosion would include the loss of surface anatomy, the “cupping” of surfaces of anterior teeth along with chipped incisal edges/incisal translucency, and loss of palatal enamel Clinical features of attrition would be flattening of surfaces on the anterior teeth This approach is not ideal due to the difficulty in reproducibilty and so other methods of record taking such as photography and the BEWE (Basic Erosive Wear Examination) can now be useful tools(2). BEWE is a scoring system, which aims to simplify the measurement of tooth loss by means of looking at the sextants of the mouth with their corresponding tooth loss and allowing a reproducible transferable diagnostic aid. Aetiology There are three aspects to tooth wear, with the problem becoming greatest when two or more are present at the same time. Triad of: 1. Erosion-defined as, “the chemical or mechanicochemical destruction of tooth substance, the mechanism of which is incompletely known, which leads to the creation of concavities and many shapes at the cementoenamel junction of teeth. The surface of the cavity, unlike dental caries, is hard and smooth”. Aetiology of erosion; Extrinsic-wines, soft drinks, heavily chlorinated swimming pools Intrinsic-gastrointestinal reflux, bulimia, anorexia nervosa Idiopathic The erosive process can be influenced by factors including; Saliva.ie Flow rates, buffering capacity, reparative ions. Reduced flow rate leads to increased possibility of erosion…i.e. surgery/Sjorgens Tooth composition and structure. i.e. hardness of an individuals enamel/dentine, response to erosive attack Dental anatomy. i.e. shape and contour of teeth, parafunction, tooth flexure (abfraction) Occlusion Soft tissue movements. i.e. increasing/decreasing acid contact with teeth 2. Attrition, which is defined as “the normal loss of tooth substance resulting from friction caused by physiological forces”. This would be the rubbing of tooth surfaces against each other and includes also parafunctional habits of bruxism and clenching. Also included here would be the commonly seen situation of a porcelain restoration opposing a natural, unrestored tooth. 3. Abrasion-“The grinding or wearing away of tooth substance by mastication, incorrect brushing, bruxism or similar causes” (Mosby’s dental Dictionary 2004). This would normally be associated with foreign objects, which most commonly would be tooth-brushing action with abrasive toothpaste. Prevention/Advice Patients suffering erosion should be educated regarding the erosive components of their diet. Avoiding sugary/fizzy drinks, reducing the overall intake of acidic foods and drinks and to cool drinks where possible, and not brushing within 30 – 60 minutes of consumption of these items. The consumption of acidic foods and/or drinks can cause weakening of the tooth surface which will lead possibly to 10 times the rate of wear at the time of consumption. Anorexia Nervosa or Bulimic patients should be advised regarding not brushing their teeth after vomiting but instead to use an antacid mouthwash, and should be referred to their GP or GIT consultant for treatment. This is also the case for those suffering with Gastro-Oesophageal Reflux Disorder. The only symptom of this may be the patient being aware of sometimes having an acidic taste at the back of the mouth. A treatment, which can be very effective, is the use of a protein pump inhibitor prescribed by the patient’s general medical practitioner. Oral hygiene advice regarding tooth brushing technique and the timing of tooth brushing with regards to eating/drinking, the management of dental plaque with its associated acids is another important patient education. Clinical Treatment Treatment of tooth wear needs to have a multidisciplinary approach. Following appropriate diagnosis, this should consist of prevention, patient advice, clinical treatment (restorative/non-restorative) and referral where necessary. The active treatment of tooth surface loss should be aimed at protecting worn and wearing surfaces from further tooth loss first and foremost. Fluoride. The use of a CPP-ACP compound as found in the likes of “GC Tooth Mousse”, can be encouraged. This has been shown (3) to aid the remineralization of enamel and as such should help to reduce enamel loss Composite restorations. The bonding to enamel is straightforward and effective whilst bonding to dentine is less so. It can be argued that the treatment of tooth surface loss is best initiated early while the enamel surface area is greatest. Dahl appliance. Crowning teeth or other laboratory-based treatments should be avoided. The preparation necessary to create such restorations is far too destructive to be deemed necessary. It has been shown that crowned teeth have a 15% likelihood of becoming non-vital after 10 years(4) The Dahl Appliance The “Dahl Principle” of treating worn teeth has been around since 1962. The principle relies on obtaining space for the restoration of worn teeth. Evidence shows that it is an effective treatment that can be confidently used (5). The Dahl Principle works on the basis of building onto the anterior teeth and then allowing the eruption of the posterior teeth to increase the occlusal vertical dimension. This will now be carried out ideally with the use of directly bonded composite to the palatal surfaces of the upper anterior teeth. The initial phase should be the bonding of composite to the upper anterior palatal surfaces and then 1 week later followed by thorough occlusal equalization. The review then following the initial bite equalization should be at three months. Over a period of 1 to 4 months, the posterior teeth will erupt into occlusion. Patient Communication Regarding Restorations Patients need to be aware that composite restorations will need occasional repolishing and that composite will wear approximately at the same rate as enamel. Patients need to understand that the reason for the initial treatment is to correct the problem with the occlusion. It may be the case that the initial treatment also works on an aesthetic level but this is not necessarily always going to be the case and further aesthetic treatment may be required. Longevity Studies show that the long term success of anterior composites (6) is sufficient for this to be a recommended treatment for the treatment of tooth wear. References (1)White DA, Pitts N, Steele J, Cooke P, et al. 2011. NHS Information centre (2) B. Dixon, M. O. Sharif, F. Ahmed, A. B. Smith, D. Seymour & P. A. Brunton.(2012),Evaluation of the basic erosive wear examination (BEWE) for use in general dental practice. British Dental Journal vol:213 iss:3 (3) Ferrazzano, G. F., Amato, I., Cantile, T., Sangianantoni, G. and Ingenito, A. (2011), In vivo remineralising effect of GC Tooth Mousse on early dental enamel lesions: SEM analysis. International Dental Journal, 61: 210–216. doi: 10.1111/j.1875-595X.2011.00059.x (4) Cheung, G. S. P.; Lai, S. C. N.; Ng, R. P. Y. (2005) Fate of vital pulps beneath a metal-ceramic crown or a bridge retainer. International Endodontic Journal Vol. 38 Issue 8 Page Numbers: 521-530 (5) Poyser, N. J., Porter, R. W. J., Briggs, P. F. A., Chana, H. S., & Kelleher, M. G. D. (2005). The dahl concept: Past, present and future. British Dental Journal, 198(11), 669-76; quiz 720. doi:http://dx.doi.org/10.1038/sj.bdj.4812371 (6) Burke, F. J. T., Kelleher, M. G. D., Wilson, N. and Bishop, K. (2011), Introducing the Concept of Pragmatic Esthetics, with Special Reference to the Treatment of Tooth Wear. Journal of Esthetic and Restorative Dentistry, 23: 277–293. doi: 10.1111/j.1708-8240.2011.00462.x