General Guidance for the administration of
advertisement
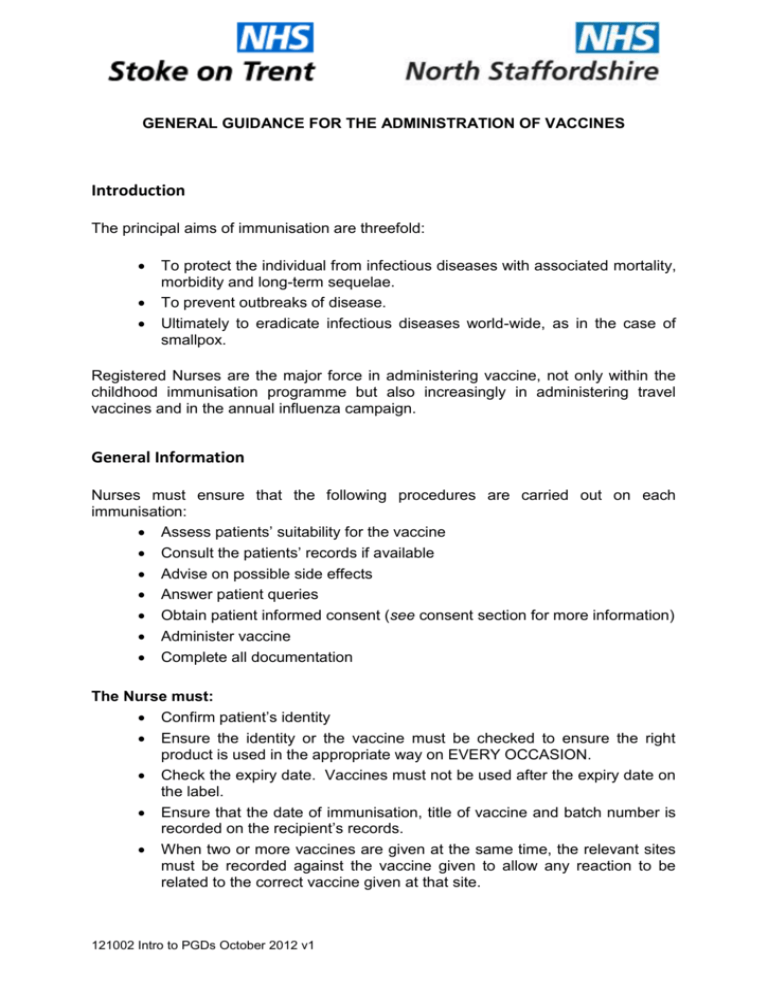
GENERAL GUIDANCE FOR THE ADMINISTRATION OF VACCINES Introduction The principal aims of immunisation are threefold: To protect the individual from infectious diseases with associated mortality, morbidity and long-term sequelae. To prevent outbreaks of disease. Ultimately to eradicate infectious diseases world-wide, as in the case of smallpox. Registered Nurses are the major force in administering vaccine, not only within the childhood immunisation programme but also increasingly in administering travel vaccines and in the annual influenza campaign. General Information Nurses must ensure that the following procedures are carried out on each immunisation: Assess patients’ suitability for the vaccine Consult the patients’ records if available Advise on possible side effects Answer patient queries Obtain patient informed consent (see consent section for more information) Administer vaccine Complete all documentation The Nurse must: Confirm patient’s identity Ensure the identity or the vaccine must be checked to ensure the right product is used in the appropriate way on EVERY OCCASION. Check the expiry date. Vaccines must not be used after the expiry date on the label. Ensure that the date of immunisation, title of vaccine and batch number is recorded on the recipient’s records. When two or more vaccines are given at the same time, the relevant sites must be recorded against the vaccine given to allow any reaction to be related to the correct vaccine given at that site. 121002 Intro to PGDs October 2012 v1 It is considered good practice to record all sites at administration. Recommended storage conditions must be observed at all times. Black triangle vaccines can be given under PGDs, provided they are used in accordance with the schedules recommended by the Joint Committee on Vaccination and Immunisation (JCVI). Unlicensed vaccines that do not have a Marketing Authorisation (previously known as a Product License) in the UK CANNOT be given under PGD. If vaccines are outside 2 to 8 0C and manufacturers can guarantee immunogenicity the vaccines are outside of license please refer to the GP (or Community Nursing Manager) as these vaccines can only be administered via a Patient Specific Direction (PSD). The Nurse should ensure: Neither the vaccine nor the diluent has passed its expiry date. Each dose is drawn up as required. Only one type of vaccine is mixed in each syringe, unless specifically stated by the manufacturer. Any vaccine which contains particles or whose colour differs from the description, in line with the manufacturer’s guidance, must be discarded. Reconstitution Where a vaccine has to be reconstituted prior to administration, when available USE ONLY the diluent supplied. When a vaccine does not need to be reconstituted, follow manufacturer’s recommendation. Note the timescale that the vaccine has to be given once reconstituted (usually one to four hours). A green needle (21G x 38mm - 1½ inch) should be used to draw up the diluent and to inject it slowly into the ampoule containing the vaccine. Draw the appropriate dose up into a clean syringe and change the needle to the appropriate size and gauge for administration to the specific patient. When removing liquid from a vacuum-sealed ampoule, first inject the equivalent measure of air to the volume of liquid to be removed. When drawing up from a glass ampoule, use a needle gauge no larger than 21G to eliminate the possibility of glass fragments being drawn up. Where possible change a needle after it has passed through a rubber bung before administration to a patient. For quantities less than 1ml use a graduated 1 ml syringe. Discard unused reconstituted vaccines at the end of the session or if the vaccine exceeds recommended timescale for use. 121002 Intro to PGDs October 2012 v1 The correct length and gauge of the needle are key in ensuring that the vaccine is delivered to the correct location as painlessly as possible and with maximum immunogenicity. The colour on the hub of the needle refers to the gauge rather than the length of the needle. Standard UK Needle Gauge and Length Colour Length - metric Length imperial Gauge Orange Orange Orange Blue Green 10 mm 16 mm 25 mm 25 mm 38 mm 3/8 inch 5/8 inch 1 inch 1 inch 1½ inches 25 25 25 23 21 A 25mm needle length is preferable and suitable for all ages 16mm needle length is only recommended for pre-term or very small infants In larger adults, a longer length (38mm) may be required – individually assess patients The width of the needle (gauge) may also need to be considered. A 23gauge or 25-gauge needle is recommended for intramuscular administration of most vaccines. For intramuscular injections in infants, children and adults, therefore, a 25mm 23G (blue) or 25mm 25G (orange) needle should be used. Administration Vaccines are routinely given intramuscularly into the upper arm or anterolateral thigh. For individuals with a bleeding disorder, however, vaccines should be given by deep subcutaneous injection to reduce the risk of bleeding. A doctor may delegate responsibility for immunisation to a registered nurse under the conditions of a Patient Group Direction. Whilst there is no legal requirement for a doctor to remain within the premises whilst immunisations are administered, this procedure should only be performed by the nurse involved if she feels competent to undertake the task and there is another member of staff in the surgery to summon emergency help if necessary. 121002 Intro to PGDs October 2012 v1 Very premature infants (born ≤ 28 weeks of gestation) who are in hospital should have respiratory monitoring for 48-72 hrs when given their first immunisation, particularly those with a previous history of respiratory immaturity. If the child has apnoea, bradycardia or desaturations after the first immunisation, the second immunisation should also be given in hospital, with respiratory monitoring for 48-72 hrs. Immunisation in the Home Vaccination in the home must only be carried out with the agreement between the General Practitioner and the Provider Organisation. Nurses will ensure that resuscitation equipment is available on site at the time of immunisation and any action in the event of a collapse is in accordance with the training received. Recipients of any vaccine should be observed for any adverse reactions and should remain under observation until they have been seen to be in good health and not to be experiencing an immediate adverse reaction. The nurse must ensure that there is a competent person on site to obtain medical support in an emergency situation. If the home does not have a telephone, a mobile telephone must be available. If the immuniser has any concern, the immunisation must be delayed. Any difficulties must be communicated to the appropriate senior manager without delay. Immunisation in the School Setting Two practitioners must be present either 2 nurses or doctor/nurse. Practitioners must wait on the school premises for 30 minutes after the last vaccine has been administered. Practitioners must inform the school of action to be taken in the event of a vaccinated child having an adverse reaction. A letter of explanation must be written to the parent of any child excluded from vaccination. 121002 Intro to PGDs October 2012 v1 Consent General Consent must be obtained before starting any treatment or physical investigation or before providing personal care for a patient. This includes the administration of all vaccines. The giving and obtaining of consent is viewed as a process and not a one-off event. There is not legal requirement for consent to be in writing and a signature on a consent form is not conclusive proof that consent has been given, but serves to record the decision and the discussions that have taken place with the patient or the person giving consent on a child’s behalf. Consent obtained before the occasion upon which a child is brought for immunisation is only an agreement for the child to be included in the immunisation programme and does not mean that consent is in place for each future immunisation. Where the immunisation consists of a series of injections consent will be sought for the series as a whole, however this does not remove the requirement to re-affirm consent on each occasion the vaccine is administered. For single course vaccines consent should be still sought on the occasion of each immunisation visit. How consent should be sought The health professional providing the immunisation should ensure that there is consent. The process of obtaining consent for vaccination should be the same whether the consent obtained is written, verbal or implied (e.g. holding out an arm to be vaccinated). Before the patient can make their decision they need to have a clear explanation and an opportunity to ask questions about: The need for vaccination The vaccine and number of doses required The risks associated with the disease the patient is being immunised against The risks/side effects associated with the vaccine It is good practice to check that the person still consents to you providing each immunisation before it is given. The Nursing and Midwifery Council’s The Code: Standards of Conduct, Performance and Ethics for Nurses and Midwives (2008) page 1 http://www.nmc-uk.org/Nursesand-midwives/Standards-and-guidance1/The-code/The-code-in-full/ states “As a professional, you are personally accountable for actions and omissions in your 121002 Intro to PGDs October 2012 v1 practice and must always be able to justify your decisions.” Giving an immunisation without consent could leave the health professional vulnerable to legal action and action by their regulatory body. Who can give consent Adults Adults are those aged 18 or over. An adult must consent to their own treatment. Under English law, no one is able to give consent on behalf of an adult unable to give consent for examination or treatment him or herself. The Mental Capacity Act 2005 sets out how treatment decisions should be made for people of 16 years of age or older who do not have the capacity to make such decisions (more information will be available at www.dh.gov.uk/consent ). If an adult has refused immunisation before losing the capacity to make a decision, this decision will be legally binding, provided that it remains valid and applicable to the circumstances. If an adult has not clearly refused the treatment before losing the capacity to make such a decision, you will be able to treat an adult who is unable to give consent if the treatment would be in their best interests, e.g. in a nursing home situation where the risk of influenza could compromise the individual’s health. This decision would be made by the patient’s doctor in discussion with those close to the patient. Routine Immunisation in school/competency Where immunisations are routinely offered in the school setting, the situation differs depending on the age and competence of the individual child or young person. Information leaflets should be available for the child’s own use and to share with their parents prior to the date that the immunisation is scheduled. Young people aged 16 and 17 are presumed, in law, to be able to consent to their own medical treatment. Younger children who understand fully what is involved in the proposed procedure (Gillick competent as outlined in the Fraser Guidelines) can also give consent, although ideally their parents will be involved. If a person aged 16 or 17 or a child competent under the Fraser Guidelines consents to treatment, a parent cannot override that consent. If the health professional giving the immunisation felt a child was not competent under the Fraser guidelines then the consent of someone with parental responsibility would be sought. If a person aged 16 or 17 or a competent child competent under the Fraser Guidelines refuses treatment that refusal should be accepted. It is unlikely that a person with parental responsibility could overrule such a refusal. It is possible that the court might overrule a young person’s refusal if an application to court is made under section 8 of the Children Act 1989 or the inherent jurisdiction of the High Court. There is no requirement for consent to be in writing. 121002 Intro to PGDs October 2012 v1 Who has parental responsibility Mothers automatically have parental responsibility for their children. Fathers also have parental responsibility if they were married to the mother when the child was conceived or born, or if he married her later. By law, unmarried fathers do not automatically have parental responsibility and before 1st December 2003 they could only obtain this by: Parental responsibility order granted by the court. Residence order granted by the court. Parental responsibility agreement (this must be signed by both parents, their signature witnessed by an officer of the court or a magistrate) Since 1st December 2003 unmarried father’s who is the natural father of the child can also acquire parental responsibility if he is named as the father on the child’s birth certificate. A step parent may acquire parental responsibility of a child where s/he is married to, or a civil partner of, the child’s parent who has parental responsibility and either (i) there is a parental responsibility agreement to this effect or (ii) the court grants a parental responsibility order (see Section 4A of the Children Act 1989). Although the consent of one person with parental responsibility for a child is usually sufficient (see Section 2(7) of the Children Act 1989), if one parent agrees to immunisation but the other disagrees, the immunisation should not be carried out unless both parents can agree to immunisation or there is a specific court approval that the immunisation is in the best interests of the child. Children may be brought for immunisation by a person without parental responsibility, for example, a grandparent or childminder. Where a child is brought for immunisation by some one who does not have parental responsibility the health professional would need to be satisfied that: The person with parental responsibility has consented in advance to the immunisation (i.e. they received all the relevant information in advance and arranged for the other person to bring the child to the appointment) or The person with parental responsibility has arranged for this other person to provide the necessary consent (i.e. they asked the other person to take the child to the appointment, to consider any further information given by the health professional, and then to agree to immunisation if appropriate). If there is any evidence that the person with parental responsibility: May not have agreed to the immunisation (e.g. the notes indicate that the parent(s) may have negative views on immunisation), or 121002 Intro to PGDs October 2012 v1 May not have agreed that the person bringing the child could give the necessary consent (e.g. suggestion of disagreements between the parents on medical matters) then the person with parental responsibility should be contacted for their consent. If there is disagreement between the people with parental responsibility for the child, then immunisation should not be carried out until their dispute is resolved. Further guidance on consent can be found at: http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAnd Guidance/DH_4005762 and in the Green Book Chapter 2. Purpose of the Patient Group Directions PGDs are defined as written instructions for the supply or administration of medicines to groups of patients who may not be individually identified before presentation for treatment (SI 2000/1917). PGDs are not a form of prescribing but provide a legal framework for the supply and/or administration of medicines by a range of qualified healthcare professionals e.g. nurses. Employing organisations must ensure that all users of PGDs are fully competent and trained in their use. These Patient Group Directions apply to all nurses and delegating GPs working in NHS North Staffordshire or NHS Stoke-on-Trent, wherever immunisation is given. Characteristics of Staff Qualifications Required Continuing Training Requirements Additional Requirements Registered nurse with current registration with the NMC Vaccination and Immunisation Training CPR and anaphylaxis training Vaccination and Immunisation training and CPR and anaphylaxis training is a mandatory pre requisite to give vaccines by a PGD. These should be attended annually. However, at a minimum training should be complete at intervals of a maximum period of 18 months. If a new vaccine or programme is introduced, appropriate specific training must be attended. Peer and self assessment is required until competent to administer immunisations. To read and understand the PGDs for the administration of immunisation. Signed agreement for each PGD to be completed by the Practitioner and PCT Manager/GP for each vaccination to be given. Immediate access to adrenaline (epinephrine) 1:1000 All who immunise must be competent to recognise and advise on the management of adverse reactions as detailed in the Green Book and manufacturer’s Summary of Product Characteristics (SPC) Access to ‘Immunisation against Infectious Disease’ (Green Book) and compliance with its recommendations. 121002 Intro to PGDs October 2012 v1 For Black Triangle drugs, all adverse drug reactions (ADRs) should be reported. For other drugs significant ADRs only need be reported. Patients with suspected ADRs should be referred to an appropriate doctor for investigation. If appropriate a report should be made using a yellow card (copies in the BNF) to the Medicines and Healthcare products Regulatory Agency. The difference between prescribing and Patient Group Directions Independent prescribers can give a documented Patient Specific Direction (PSD), which instructs another healthcare professional to supply or administer a medicine to a specified patient. Alternatively, a Patient Group Direction (PGD) is a legal mechanism that allows named registered healthcare professionals to supply and/or administer medicines to groups of patients that fit the criteria laid out in the PGD. So a healthcare professional could supply (e.g. provide an inhaler or tablets) and/or administer a medicine (e.g. give an injection or a suppository) directly to a patient without the need for a prescription or an instruction from a prescriber. Using a PGD is not a form of prescribing. Confusion can arise about the difference between a PGD and the other mechanisms for prescribing, supply and administration of medicines, and which is the most appropriate for the particular circumstances. When a prescriber sees a patient, and following assessment and diagnosis, decides that a medicine is needed as part of the treatment plan; in the majority of cases, a prescription is issued. A pharmacist then dispenses the medicine against the prescription and the patient receives their medicine. Medicines law recognises the value of pharmacists in the checking and dispensing process and this is the main route by which patients get their medicines. However, in some cases, it may be necessary or convenient for a patient to receive a medicine (i.e. have it supplied and/or administered) directly from another healthcare professional. Unless already covered by exemptions to the Medicines Act, there are two ways of achieving this; by Patient Specific Direction (PSD) or Patient Group Direction (PGD). A PSD is used once a patient has been assessed by a prescriber and that prescriber, (doctor, dentist or other independent prescriber) instructs another healthcare professional in writing to supply or administer a medicine directly to that named patient or, to several named patients (e.g. patients on a clinic list). A PSD is a direct instruction and does not require an assessment of the patient by the healthcare professional instructed to supply and/or administer, unlike a PGD. It is the responsibility of the person issuing the PSD to ensure that the individual supplying or administering the medicine is competent to do so. For further information on the difference between a Patient Group Direction (PGD) and a Patient Specific Direction please refer to the NPC document: 121002 Intro to PGDs October 2012 v1 Patient Group Directions December 2009 - A practical guide and framework of competencies for all professionals using patient group directions. http://www.npc.nhs.uk/non_medical/resources/patient_group_directions.pdf Travel Health and excluded vaccines Any vaccines not included within these PGDs please refer to the Green Book. http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAnd Guidance/DH_079917 Inclusion criteria for certain PGDs The SPC for some vaccines means that off-licence recommendations are included. However, the recommendations in these PGDs are in line with Joint Committee on Vaccination and Immunisation (JCVI) guidance as contained in Green Book chapters and represent best clinical practice. Development Team These PGDs contained in the set are based on the previous PGD document “Patient Group Directions for the Administration of Immunisations within Primary Care, (PGD/VI/SEPT/2010, Issued 1 October 2010. Review Date 1 October 2012 V1.02 Amended July 2011.) Development team details for original draft The Patient Group Directions were originally developed for use in the North Staffordshire Health Economy by the following multi-disciplinary team: Dr James Bashford Mrs Julia Briscoe Ms Jan Butterworth Dr Philippa Dove Ms Catherine Jackson Dr Margaret Jones Mrs Jacqueline Kinsey Dr David Phillips Ms Sandra Sheppard Dr Hilary Thurston Ms Diane Walton Mrs Pat Wheeler Mrs Angela Willdigg Dr Hilary Thurston Dr John Chesworth Ms Catherine Jackson Ms Jacqueline Kinsey Ms Rose Dent Mrs Angela Willdigg 121002 Intro to PGDs October 2012 v1 Chairman, District Prescribing Advisory Group Nurse Adviser NSHA Community Pharmacy Facilitator Clinical Governance Lead Newcastle PCG Senior Pharmacist Community Services Medical Director NSHA Pharmaceutical Adviser NSHA Prescribing Lead Central Stoke PCG Practice Nurse, Harley St Surgery Consultant in Communicable Disease NSHA Combined Health Care Community Manager, Newcastle PCT Senior Nurse Manager Consultant in Communicable Disease NSHA Medical Adviser Senior Pharmacist Community Services Pharmaceutical Adviser Practise Nurse Developer Senior Nurse Manager Update September 2008 The Patient Group Directions were reviewed and updated by the following multidisciplinary group: Dr David Prayle Dr John Chesworth Sarah Sellars Melanie Brock Sue Forrester-O’Neil Allison Minshall Senior Community Medicines Advisor, NHS North Staffordshire Medial Director, NHS North Staffordshire Specialist Nurse Practitioner, High Street Practice School Nurse Professional Lead, North Staffordshire Provider Services District Nurse Lead, North Staffordshire Provider Services Professional Lead for Practice Nursing, NHS Stoke on Trent Update October 2009 The Patient Group Directions were reviewed and updated by the following multidisciplinary group: Dr Manir Hussain Emma Maddocks Allison Minshall Head of Medicines Management, NHS North Staffordshire Medicines Management Pharmacist, NHS Stoke on Trent PCT Vaccine and Immunisation Lead/ Co-ordinator, NHS Stoke on Trent Update March 2010 The Patient Group Directions were reviewed and updated by the following multidisciplinary group: Dr Manir Hussain Emma Maddocks Sandra Guerrero Allison Minshall Head of Medicines Management, NHS North Staffordshire Medicines Management Pharmacist, NHS Stoke on Trent Prescribing Advisor, NHS North Staffordshire PCT Vaccine and Immunisation Lead/ Co-ordinator, NHS Stoke on Trent Full review July – November 2010 The PGDs contained in this set were reviewed by the following multidisciplinary group: Dr John Chesworth Mara Cope 121002 Intro to PGDs October 2012 v1 Medial Director, NHS North Staffordshire Prescribing Advisor, NHS North Staffordshire Emma Maddocks Allison Minshall Liesa Coleclough Chris McGrath Rachel Shaw Margaret Welch Medicines Management Pharmacist, NHS Stoke on Trent PCT Vaccine and Immunisation Lead/ Co-ordinator, NHS Stoke on Trent Medicines Management Technician, NHS North Staffordshire Health Visitor, NHS North Staffordshire Health Visiting Team, NHS North Staffordshire Head of Medicines Management, Stoke-on-Trent Community Health Service. Update January 2011 The Patient Group Directions were reviewed and updated by the following multidisciplinary group: Mara Cope Prescribing Advisor, NHS North Staffordshire Emma Maddocks Medicines Management Pharmacist, NHS Stoke on Trent Allison Minshall PCT Vaccine and Immunisation Lead/ Co-ordinator, NHS Stoke on Trent Update July 2011 The Patient Group Directions were reviewed and updated by the following multidisciplinary group: Mara Cope Prescribing Advisor, North Staffordshire CCG Emma Dasey (née Maddocks) Medicines Management Pharmacist, Stoke on Trent CCG Allison Minshall PCT Vaccine and Immunisation Lead/ Co-ordinator, NHS Stoke on Trent Full review July 2012 (Repevax in pregnancy added October 2012) Caroline Acuda Prescribing Advisor, North Staffordshire CCG Fiona Riley Prescribing Advisor, Stoke on Trent CCG Emma Dasey Prescribing Advisor, Stoke on Trent CCG Allison Minshall PCT Vaccine and Immunisation Lead/ Co-ordinator, NHS Stoke on Trent 121002 Intro to PGDs October 2012 v1 References Immunisation Against Infectious Diseases DOH http://immunisation.dh.gov.uk/category/the-green-book/ Department of Health (1998): Review of Prescribing, Supply and Administration of Medicines. A report on the Supply and Administration of Medicines under Group Protocol. Department of Health (2001): Good practice in consent implementation guide: consent to examination or treatment http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAnd Guidance/DH_4005762 NMC standards for Medicines Management 2008 http://www.nmcuk.org/Documents/NMCPublications/238747_NMC_Standards_for_medicines_management.pdf NMC 2008 The code http://www.nmc-uk.org/Nurses-and-midwives/Standards-andguidance1/The-code/The-code-in-full/ Health Service Circular (1998) HSC.98/051. Report on the Supply and Administration of Medicines under Group Protocols Health Service Circular 2000/26 - Patient Group Directions UK Guidance on Best Practice in Vaccine Administration 2001 http://www.rcn.org.uk/__data/assets/pdf_file/0010/78562/001981.pdf 121002 Intro to PGDs October 2012 v1 Patient Group Directions included in this set are: PGD Number 1 2 3a 3b 4 5a 5b 6 7a 7b 8 9 10 11 12 13 14a 14b 15 16 17 18 19 20 21 22a 22b 23 Immunisation PGD name MMR - MEASLES, MUMPS AND RUBELLA LIVE VACCINE(MMR) INACTIVATED INFLUENZA VACCINE MENINGOCOCCAL A,C,W 135,Y CONJUGATE VACCINE (MENACWY) MENVEO®▼ MENINGOCOCCAL A,C,W 135,Y CONJUGATE VACCINE (MENACWY) ACWY VAX® PNEUMOCOCCAL POLYSACCHARIDE VACCINE (23 VALENT) (PPV) HEPATITIS A FOR CHILDREN HEPATITIS A FOR CHILDREN (VAQTA PAEDIATRIC®) Reference and version number for PGD 1MMRv1 2Influenzav1 3aMenACWYMenveov1 3bMenACWYVaxv1 4PPVv1 5aHepAchildv1 5bHepAchildVaqtaPaedv1 HEPATITIS A FOR ADULTS 6HepAadultv1 TYPHOID FEVER 7aTyphoidv1 TYPHOID FEVER ORAL (VIVOTIF® CAPSULES) MENINGOCOCCAL GROUP C CONJUGATE VACCINE 7bTyphoidoralVivotifv1 8MenCv1 HEPATITIS B VACCINE FOR ADULTS 9HepBadultsv1 HEPATITIS B VACCINE FOR CHILDREN 10HepBchildv1 HEPATITIS A (INACTIVATED) AND HEPATITIS B (RDNA) (HAB) VACCINE (ADSORBED) TWINRIX® ADULT HEPATITIS A (INACTIVATED) AND HEPATITIS B (RDNA) (HAB) VACCINE (ADSORBED) TWINRIX® PAEDIATRIC HEPATITIS A (INACTIVATED) AND HEPATITIS B(RDNA) (HAB) VACCINE (ADSORBED) FOR CHILDREN AMBIRIX® HEPATITIS A (INACTIVATED, ABSORBED ) AND TYPHOID POLYSACCHARIDE VACCINE HEPATYRIX® HEPATITIS A (INACTIVATED, ABSORBED ) AND TYPHOID POLYSACCHARIDE VACCINE VIATIM® OXYGEN ADRENALINE (EPINEPHRINE) 1MG/1ML INJECTION 11HepABtwinadultv1 12HepABtwinchildv1 13HepABambirixv1 14aHepatyrixv1 14bViatimv1 15Oxygenv1 16Adrenalinev1 DIPHTERIA, TETANUS/ACELLULAR PERTUSSIS, INACTIVATED POLIO VACCINE AND HIB (DTaP/IPV/Hib) PEDIACEL® DIPHTHERIA, TETANUS, PERTUSSIS (ACELLULAR COMPONENT) AND POLIOMYELITIS (INACTIVATED) VACCINE - REPEVAX® / INFANRIX-IPV DIPHTHERIA, TETANUS AND INACTIVATED POLIO VACCINE Td/IPV (REVAXIS®) PNEUMOCOCCAL POLYSACCARIDE CONJUGATE VACICNE (13-VALENT, ADSORBED) PREVENAR 13®▼ HAEMOPHILUS INFLUENZAE TYPE B AND MENINGOCOCCAL C CONJUGATE VACCINE MENITORIX® HUMAN PAPILLOMAVIRUS (HPV) CERVARIX® 22aHPVCervarixv1 HUMAN PAPILLOMAVIRUS (HPV) GARDASIL® ▼ 22bHPVGardasilv1 LOW DOSE DIPHTHERIA, TETANUS, ACELLULAR PERTUSSIS AND INACTIVATED POLIOMYELITIS VACCINE - REPEVAX® FOR PREGNANT WOMEN 121002 Intro to PGDs October 2012 v1 17Pediacelv1 18Rep/Infanv1 19Revaxisv1 20Prevenarv1 21Menitorixv1 23Repevax_Pregnancy_v1 Please note that there are two PGDs for certain vaccines, e.g. HPV vaccines. In some cases vaccines are not interchangeable – please refer to the relevant PGD and SPC. Please ensure you are familiar with the content of these PGDs and select the vaccines with care. 121002 Intro to PGDs October 2012 v1