104******* *********** ********* *****1* 5103043003
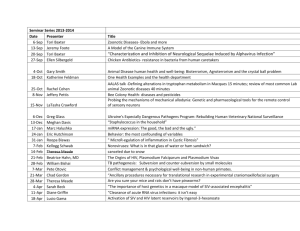
advertisement

國立中興大學 104 學年度第一學期 食品暨應用生物科技學系 碩士在職專班二年級 專題討論第 1 位 5103043003 顏珀玟 TITLE: Establishment of the intestinal microbiota and its role for atopic dermatitis in early childhood 建立腸道菌相及其在幼兒異位性皮膚炎的影響 SOURCE: Journal of Allergy and Clinical Immunology 2013;132: 601-7. SPEAKER: Yen Po-wen, 顏珀玟 (ID: 51030043003) MODERATOR: 粘宏堃 DATE & TIME: 2014/12/6 09:00 (NO. 1) 1. Abstract Background: Several epidemiologic studies showed that gut microbiota is the key of developing immunologic tolerance. The present study examined the composition of the intestinal microbiota in infancy in association to the subsequent development of atopic dermatitis (AD) and sensitization to common food allergens. Method: The study was conducted within the context of a randomized, placebo-controlled trail on the prevention of AD by oral supplementation of a bacterial lysate between the age of 5 weeks and the end of month 7, feces was collected at the age of 5 (n=571), 13 (n=332), 31 weeks (n=499) and subjected to quantitative PCRs to detect target bacteria. Results: If colonized, infants delivered by C-section had lower counts of bifidobacteria and bacteriods and higher count of clostridia than infants delivered spontaneously. With increasing number of siblings, the colonization of clostridia decreased (P for trend < 0.001), and lactobacilli (P for trend < 0.001) and bacteroides (P for trend = 0.02) increased in GI of infant at the age of 5 weeks. Mediation analyses showed a statistically significant indirect effect of increased risk of clostridia colonization on AD development. (OR adjusted, 2.51; 95% CI, 1.304.86) Conclusion: Birth mode, birth order and breast-feeding were strong associated with GI microbiota composition. Clostridium cluster I colonization in infant at the age of 5 weeks is positive associated with the increasing development of AD. 2. Introduction Some epidemiologic studies found that the differences in the composition and diversity of the gut microbiota preceded the development of allergic sensitization. The colonization of microorganisms in intestine begins after delivery. The bacteria in the intestine waxes and wanes if diet changes and the host develops. On the establishment of the intestine microbiota in infancy, the authors investigated the nonhost factors by oral supplementation of a bacterial lysate to examined the composition of the infant intestinal microbiota, and they also examined the association the intestinal microbiota composition and the development of AD and sensitization to common food allergens. 3. Methods 3.1 Study population: a randomized, placebo-controlled trail was devised to assess the prevention of AD by an oral supplementation with heat-killed bacterial lysate from the age of week 5 until the end of week 31 postpartum. The feces of 606 healthy newborns with a single or double heredity for atopy (AD, allergic rhinitis, and/or asthma) were collected at the age of 5 week (n=571), 13 weeks (n=332), 31 weeks (n=499) as samples. 3.2 DNA purification from feces: at the laboratory approximately 200mg feces was diluted in and stored at -80 ℃. For DNA isolation, the diluted feces was added to a vial with glass beads and buffer, and the samples were disrupted in a mechanical bead beater at 5000 rpm for 3 minutes. DNA yields were measured with an 國立中興大學 104 學年度第一學期 食品暨應用生物科技學系 碩士在職專班二年級 專題討論第 1 位 5103043003 顏珀玟 Eppendorf Photometer. 3.3 Microbial analysis of fecal samples: DNA from the samples was subjected to quantitative real-time PCR assays for the quantification of bifidobacteria, E. coli, Clostridium difficile, Clostridium cluster I, bacteroides fragilis group, and lactobacilli. 3.4 Diagnosis of AD: AD was clinically assessed by a pediatrician at 13, 21, 31 weeks of infants, also at the age of 1, 2, and 3 years for follow-up. 3.5 Sensitization to food allergens: sensitization to common food allergens was examined by blood sample at 31 weeks, 1 year, and 2 years of age. 4. Results 4.1 Birth mode: infants delivered by C-section were less frequently colonized by bifidobacteria, bacteroides, and E. coli, but more frequently colonized by Clostridium cluster I and C . difficile. 4.2 Number of older siblings: with increasing number of siblings, the colonization rate of clostridia (Pfor trend < .001) decreased and lactobacilli (Pfor trend < .001) and bacteroides (Pfor trend = 0.02) increased at the age of 5 weeks. 4.3 breast-feeding: a longer duration of breast-feeding was associated with a lower prevalence of C. difficile and bacteroides, and higher prevalence of lactobacilli and bifidobacteria. 4.4 Development of AD and sensitization to food allergens: colonization with Clostridium cluster I at age 5 weeks was associated with an increased risk of developing AD before the age of 31 weeks. However, sensitization to food allergens was not associated with any of bacteria under study at ages 5, 13, or 31 weeks. 4.5 Mediation analyses demonstrated that there was a statistically significant indirect effect on AD via Clostridium cluster I colonization for both birth mode and birth order. 5. Discussion 5.1 The microbiota composition of infant is profoundly different between those who were breast-fed for more than 6 months and for shorter period. Numerous bioactive compounds in breast milk might contribute to the beneficial effect on microbiota composition. 5.2 Infant delivered by C-section harbored bacterial communities which were similar to those on the skin surface, however, vaginal-delivered infants acquired bacterial communities resembling their own mother’s vaginal microbiota. 5.3 It is the first time to report that a dose-response relationship between birth order and microbiota composition in the present study. 5.4 The limitations of the present study: (1) the study includes only children with a positive family history of atopy, and the results may not be generalizable to the general population. (2) the consistency of the results make it unlikely that the mail associations reported in this study are due to spurious findings. (3) they had no information on the indication or the C-section (eg. obstetric history, anthropometric measures). 5.5 The indigenous microbiota composition is likely to be one of the underlying mechanisms explaining the birth order effect in the cause of allergies. 6. Reference Lau S, Gerhold K, Zimmermann K, Ockeloen CW, Rossberg S, Wagner P, et al. Oral application of bacterial lysate in infancy decreases the risk of atopic dermatitis in children with 1 atopic parent in a randomized, placebo-controlled trial. J Allergy Clin Immunol 2012;129:1040-7.