The Predictive Value of Kidney Allograft Baseline Biopsies for Long
advertisement

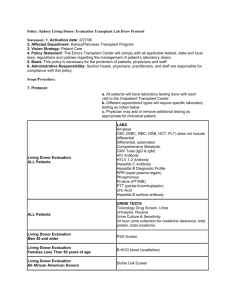
H-13: pathology in renal transplant H-15: Late rejection The Predictive Value of Kidney Allograft Baseline Biopsies for LongTerm Graft Survival Katrien De Vusser* † , Evelyne Lerut‡§ , Dirk Kuypers* † , Yves Vanrenterghem* † , Ina Jochmans‖¶ , Diethard Monbaliu‖¶ , Jacques Pirenne‖¶ and Maarten Naesens* † JASN November 2013 vol. 24 no. 11: 1913-1923 Correspondence: Dr. Maarten Naesens, Nephrology and Renal Transplantation, University Hospitals Leuven, Herestraat 49, 3000 Leuven, Belgium. Email: maarten.naesens@uzleuven.be ABSTRACT The effect of baseline histology and individual histologic lesions at the time of transplantation on long-term graft survival has been evaluated using different scoring systems, but the predictive capacity of these systems has not been adequately validated. All kidney recipients transplanted in a single institution between 1991 and 2009 who underwent a baseline kidney allograft biopsy at transplantation were included in this prospective study (N=548). All baseline biopsies were rescored according to the updated Banff classification, and the relationship between the individual histologic lesions and donor demographics was assessed using hierarchical clustering and principal component analysis. Survival analysis was performed using Cox proportional hazards analysis and log-rank testing. Mean follow-up time was 6.7 years after transplantation. Interstitial fibrosis, tubular atrophy, and glomerulosclerosis associated significantly with death-censored graft survival, whereas arteriolar hyalinosis and vascular intimal thickening did not. Notably, donor age correlated significantly with interstitial fibrosis, tubular atrophy, and glomerulosclerosis and associated independently with graft survival. On the basis of these findings, a novel scoring system for prediction of 5-year graft survival was constructed by logistic regression analysis. Although the predictive performance of previously published histologic scoring systems was insufficient to guide kidney allocation in our cohort (receiver operating characteristic area under the curve ≤0.62 for each system), the new system based on histologic data and donor age was satisfactory for prediction of allograft loss (receiver operating characteristic area under the curve = 0.81) and may be valuable in the assessment of kidney quality before transplantation. COMMENTS The demand for kidney grafts exceeds the supply of available organs. As a result, there is an increasing use of older and extended criteria donor kidneys. This is not without consequences. The risk of graft failure after an extended criteria donor kidney transplant is 70% higher than after transplantation with a standard criteria donor. The intrinsic quality of the kidney at transplantation becomes increasingly important for the post-transplant histologic evolution and long-term graft survival The Predictive Value of Kidney Allograft Baseline Biopsies for LongTerm Graft Survival Univariate and multivariate Cox proportional hazards analysis of death-censored graft survival based on baseline histology and donor demographic variables (n=542) Variables Univariate Analysis Multivariate Analysis Hazard Ratio(95% P Confidence Interval) Hazard Ratio(95% P Confidence Interval) 1.72 (1.2 до 2.46) 0.003 1.90 (1.24 до 2.9) 0.003 Stroke as reason of donor 1.38 (0.83 до 2.29) death 0.60 – – Donor history of hypertension 1.18 (0.61 до 2.29) 0.62 – – Donor diabetes mellitus 1.69 (0.23 до 12.2) 0.60 – – Donor history of smoking 0.90 (0.49 до 1.69) 0.75 – – (present 1.60 (0.99 до 2.58) 0.05 0.98 (0.59 до 1.76) 0.90 0.40 – – Donor demographics Donor age ( 60 yr) Baseline biopsy histology Tubular atrophy versus absent) Arteriolar hyalinosis (present 1.230 (0.71 до 2.38) versus absent) Interstitial fibrosis versus absent) (present 1.85 (1.32 до 2.57) 0.0003 1.51 (1.02 до 2.26) 0.03 Vascular intimal thickening 1.08 (0.26 до 4.43) (present versus absent) 0.92 – – Glomerulosclerosis versus <10%) 0.01 1.32 (0.73 до 2.39) 0.35 (≥10% 1.98 (1.21 до 3.26) De Vusser and colleagues propose a novel scoring system, the Leuven Donor Risk Score that predicts 5-year graft survival with 81% sensitivity and 85% specificity.3 The proposed score is a sum score based on known histologic (glomerulosclerosis, interstitial fibrosis, tubular atrophy) and demographic (donor age) characteristics that are, as noted above, individually associated to varying degrees with graft survival. The strengths of De Vusser and colleagues’ study include a large cohort of patients, long-term follow-up data, in-depth statistical analyses, and comparative evaluation of historical, previously published alternative scoring systems. Although these data are intriguing, the Leuven Donor Risk Score they propose is so far the most accurate predictive model. It is important to note that they have certain limitations, some of which are outlined by the authors themselves. The analysis is based on single center central European observations accounting for region-specific demographic characteristics. The authors report excellent graft survival, 94% at 2 years and 90% at 5 year.