Protocol Development Guidance for Clinical Investigations
advertisement

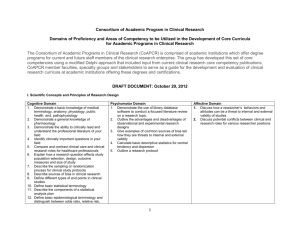
Investigational Drug Products: Protocol Development Resource & Checklist Protocol Development Guidance for Clinical Investigations Using FDA Regulated Drug Products ICTR Navigators December 16, 2011 Version 1.0 1.0 TABLE OF CONTENTS Section 1.0 Table of Contents 2.0 Introduction 3.0 Content Checklist 4.0 FDA Guidance Information 2.0 Page 2 2 2 12 INTRODUCTION The clinical protocol is the blueprint that directs the conduct of the clinical trial. The protocol must contain concise and logically arranged information that fully describes the intent of the clinical investigation. A comprehensive protocol is one of the central components of any FDA submission (e.g. IND application and IND exemption request, etc.) involving the use of an investigational device in a clinical trial as it provides specific and consistent direction to the study team, ensures that the rights and welfare of the human participants are protected, and promotes collection of quality research data. Conversely, a poorly written and incomplete protocol is likely to encounter significant delay in both the IRB and FDA review processes as reviewers may not completely understand the intent of the research or may not feel that sufficient attention has been paid to patient safety or aspects of good clinical practice. Therefore, the more comprehensive the protocol, the easier it will be for FDA and IRB reviewers to find the information they need in order to complete their analysis of the project. Using regulatory references including 21CFR50, 21CFR56, 21CFR312, ICH E:6, and the Johns Hopkins Medicine Office of Human Subjects Research policies, the ICTR DDRS has developed this resource in order to help ensure that the protocol being submitted contains essential information that FDA and IRB reviewers need to see. 3.0 PROTOCOL CONTENT DEVELOPMENT RESOURCES AND CHECKLIST The following table of suggested content may be used as a ‘checklist’ when drafting the clinical protocol to help ensure that discussion of all applicable elements is included. Within the table, the minimum suggested and optional information is noted. Also provided is the regulatory reference from which the suggested information is cited. Ultimately, the content and format of the protocol is left to the discretion of the sponsor-investigator. Page 2 of 12 Protocol Section Description and Regulatory Reference (if applicable) Title Page Minimum Suggested Information Optional Information Protocol title, Version Date, Phase, Investigation Product Name(s), IDE/IND number(s), IDE/IND sponsor(s), Financial Sponsor, and Principal Investigator (Regulatory Reference: ICH E:6, Section 6.1.1) Short Protocol Title or Acronym, Protocol number, Version Number, IRB of Record (single site or multisite with one IRB), and IRB application number. (Regulatory Reference: ICH E:6, Section 6.1.1) Amendments When amendments are made to the protocol, the title page should include, at a minimum, the date of the amendment and optionally, the amendment number. (Regulatory Reference: ICH E:6, Section 6.1.1) Table of Contents Minimum Suggested Information Include a table of contents for the protocol. Signature Page(s) Optional Information If this is a multicenter protocol, the sponsor should consider including a signature page that each site’s Principal Investigator can sign and date the protocol stating she/he will conduct the protocol as written by the Sponsor. (Regulatory Reference: ICH E:6, Section 6.1.3) List of Abbreviations Optional Information Include a list of all abbreviations and/or acronyms used throughout the protocol. Synopsis Minimum Suggested Information Optional Information Protocol title, Version Date, Phase, IDE/IND number(s), IDE/IND sponsor(s), Financial Sponsor, Principal Investigator, Study Agent/Intervention Description, Sample Size, Study Population, Study Design, Study Duration, Objective (primary, secondary, etc…), and Endpoints Short Protocol Title or Acronym, Protocol number, Version Number, IRB of Record (single site or multisite with one IRB), IRB application number, and Accrual Period A schematic flow diagram or table of the study design Page 3 of 12 General Information Name and address of the sponsor and monitor (if other than the sponsor). (Regulatory Reference: ICH E:6, Section 6.1.2 and 21 CFR 312.50) Minimum Suggested Information Name and title of the investigator(s) and sub-investigators who is (are) responsible for conducting the trial, and the address and telephone number(s) of the trial site(s). Additionally, indicate beside each name who is the qualified physician (or dentist, if applicable), who is responsible for all trial-site related medical (or dental) decisions (if other than investigator). (Regulatory Reference: ICH E:6, Section 6.1.5 & Section 6.1.6 and 21 CFR 312.23(a)(6)(iii)(a )) Name(s) and address (es) of the clinical laboratory (ies) and other medical and/or technical department(s) and/or institutions involved in the trial. (Regulatory Reference: ICH E:6, Section 6.1.7 and 21 CFR 312.23(a)(6)(iii)(a )) Key Study Team Members/Key Personnel/Key Roles Optional Information Investigators may want to consider including names, titles, and contact information for other key study team members. If not included in this section of the protocol, the names of other key study team members should be documented in the Duties and Delegation Log, in a Manuel of Procedures (MOP), or in the appendix. Examples of other key study team members include, but are not limited to: Protocol Data Manager(s) Protocol Epidemiologist(s) Protocol Pharmacologist(s) Protocol Regulatory personnel Protocol Statistician(s) Protocol Behavioral Scientist (s) NIH Representatives(s) Industry Representative(s) Other significant representative(s) Major Collaborators, if not included as site investigators (add brief statement of role) Medical Monitor (If applicable) Independent Safety Monitor (If applicable) (Regulatory Reference: 21 CFR 312.23(a)(6)(iii)(a )) Name and title of the person(s) authorized to sign the protocol and the protocol amendment(s) for the sponsor. NOTE: Only include this information if you include a signature page. If applicable (Regulatory Reference: ICH E:6, Section 6.1.3) Name, title, address, and telephone number(s) of the sponsor's medical expert (or dentist when appropriate) for the trial. NOTE: If there is no ‘medical expert’ besides the principal investigator, then this does not need to be included. (Regulatory Reference: ICH E:6, Section 6.1.4) Abstract / Précis Optional Information A written version of the synopsis that can be published where required and/or could be used in a manuscript. Background and Significance Page 4 of 12 Name and description of the investigational product(s). (Regulatory Reference: ICH E:6, Section 6.2.1) A summary of findings from nonclinical studies that potentially have clinical significance and from clinical trials relevant to the trial. (Regulatory Reference: ICH E:6, Section 6.2.2) Summary of the known and potential risks and benefits, if any, to human subjects. Minimum Suggested Information (Regulatory Reference: ICH E:6, Section 6.2.3) Description of and justification for the route of administration, dosage, dosage regimen, and treatment period(s). If an investigational device will be used in the protocol, include a general description here of the device and all major components as well as and how it will be utilized throughout the course of the trial. (Regulatory Reference: ICH E:6, Section 6.2.4) Description of the population to be studied. (Regulatory Reference: ICH E:6, Section 6.2.6) If applicable A statement that the trial will be conducted in compliance with the protocol, GCP and the applicable regulatory requirement(s). (Regulatory Reference: ICH E:6, Section 6.2.5) Trial Hypothesis, Objectives, Specific Aims, and/or Purpose Minimum Suggested Information A detailed description of the objectives, hypothesis, specific aims, and/or the purpose of the trial. (Regulatory Reference: 21 CFR 312.23(a)(6)(i)-(ii),(iii)(a ) and ICH E:6, Section 6.3) General study design Minimization of potential bias Describe the specific measures (e.g., randomization, blinding) that will be taken to minimize/avoid bias on the part of the subjects, investigators, and analysts. (Regulatory Reference: ICH E:6, Sections 6.4.3 & 6.5.3 and 21 CFR 312.23(a)(6)(i),(ii),(iii)(d )) Anticipated number of research subjects Minimum Required Information Define ‘enrollment’. Specify the estimated total number of subjects to be enrolled into the clinical study and the anticipated number of subjects expected to complete the study. (Regulatory reference: 21 CFR 312.23(a)(6)(i),(ii),(iii)(c ) and ICH E:6, Section 6.9.2) Recruitment Plan Federal regulations require that IRBs ensure that the selection of subjects for a study is equitable. As such, each protocol must explain how subjects will be identified and recruited for the study. Any approach to subjects must be non-coercive and the potential subjects must voluntarily participate in the recruitment process. (Regulatory Reference: Johns Hopkins Patient Recruitment and Referral for Research guidelines) Page 5 of 12 Informed Consent As the FDA’s primary objectives in reviewing an IND are, in all phases of the investigation, to assure the safety and rights of subjects the protocol should include discussion of the consent processes to be followed. (Regulatory references: ICH E:6, Section 4.8, 21CFR50, 21CFR60, 21CFR312.62(b), and 21CFR312.88) Screening procedures Describe or list the procedures that will be performed to verify a subject’s eligibility for participation in the clinical study. Study Treatment Study treatment and/or diagnostic product procedures Minimum Suggested Information Describe, in detail, the study treatment or diagnostic products (e.g., the investigational device and, if applicable, comparative devices or products) that will be administered to each study group or arm of the proposed clinical investigation; to include, for each study treatment or diagnostic product, the product name and FDA-approval status, dose or dose range (if applicable), route/mode of administration, dosing or exposure schedule, and treatment or exposure duration. Describe, if applicable, any plans for dose or exposure reductions or increases based on the data accrued with study progression. (Regulatory reference: ICH E:6, Section 6.6.1 and 21 CFR 312.23(a)(6)(i),(ii),(iii)(e )) Treatment adherence/ Study compliance Specify the criteria and procedures for withdrawing subjects from study participation due to non-compliance with the study treatment or diagnostic product regimen, if applicable, and/or the study procedures or investigators instructions. (Regulatory reference: ICH E:6, section 6.5.3 (a)) Investigational Drug Information If applicable, include a description of the trial treatment(s) and the dosage and dosage regimen of the investigational product(s) should be included. Also include a description of the dosage form, packaging, and labeling of the investigational product(s). Minimum Suggested Information, If applicable Insert Drug Name Other names: Classification: How supplied: Storage: (Where and how) Stability: Route of Administration: Method of Preparation: Drug Ordering and Drug Accountability: Prohibited Medications and Procedures: (Regulatory reference: ICH E:6, Section 6.4.4 and 21 CFR 312.23(a)(6)(i),(ii),(iii)(e ) ) Page 6 of 12 Investigational Device Information If applicable, provide a detailed description of each important component, ingredient, property, and principle of operation of the device and of each anticipated change in the device during the course of the investigation. Insert Device Name Classification: Manufacturer: Storage: (Where and how) Accountability: Instructions for Use: (Regulatory reference: ICH E:6, Section 6.4.4 and 21 CFR 812.25) Allocation to treatment Incorporate only if the proposed clinical study involves multiple treatment arms. Describe the plan and procedures for allocating subjects to the various treatment or diagnostic arms of the study so as to ensure comparability between test groups and any control groups with regard to pertinent variables such as gender, severity or duration of disease, and use of therapy other than the investigational device. (Regulatory Reference: ICH E:6, Sections 6.4.3 and 21 CFR 312.23(a)(6)(i),(ii),(iii)(d-e )) Breaking the blind Incorporate only if the proposed clinical study is blinded. Describe the procedures for breaking the blind should a given subject suffer a serious adverse event wherein knowledge of the identity of the study treatment or diagnostic product received by the subject is necessary for effective emergency treatment of the event (Regulatory reference: ICH E:6, Section 6.4.8) Treatment adherence/ Study compliance If applicable, describe the procedures that will be used to assess subject compliance/adherence with the assigned study treatment or diagnostic product regimen. If applicable, specify whether or not subjects withdrawn from study participation due to noncompliance will be replaced and, if so, the corresponding procedures for their replacement. (Regulatory reference: ICH E:6 Section 6.6.3 & Section 6.5.3 (c)) Follow-up Procedures Schedule of evaluations and study activities Minimum Suggested Information Incorporate, as a referenced attachment (i.e., Appendix ___), a table that summarizes the protocol procedures that will be performed at screening, for treatment or diagnosis, and at follow-up (if applicable). (Regulatory reference: ICH E:6, Section 6.6.1 and 21 CFR 312.23(a)(6)(i),(ii),(iii)(f-g)) Procedures to assess efficacy If applicable Specify the parameters (i.e., observations and/or measurements) that will be used to evaluate the efficacy of the study treatment or diagnostic product(s); to include the methods and timing for assessing, recording, and analyzing these parameters (Regulatory reference: ICH E:6, Sections 6.7 and 21 CFR 312.23(a)(6)(i),(ii),(iii)(f )) Page 7 of 12 Procedures to assess safety Specify the parameters (i.e., procedures, laboratory tests, or other measures) that will be used to evaluate the safety of the study treatment or diagnostic product(s); to include the methods and timing for assessing, recording, and analyzing these parameters. (Regulatory reference: ICH E:6, Section 6.8 and 21 CFR 312.23(a)(6)(i),(ii),(iii)(g )) Supportive care Describe any supportive care (i.e., procedures, laboratory tests, or other measures) that will be administered in the course of trial follow-up. (Regulatory reference: ICH E:6, Section 6.6.1) Statistical Considerations and Study outcome evaluations Study endpoints Summarize the primary and, if applicable, secondary endpoints or outcomes that will be evaluated in the clinical study. (Regulatory reference: ICH E:6, Section 6.4.1) Sample size determination Specify the number of subjects planned to be enrolled into the clinical study (i.e., to complete the clinical study) and the reason(s) for the choice of this sample size. Include, if applicable, calculations of the power of the study or provide an alternate explanation for the proposed sample size. For example, if the purpose of the proposed clinical study is to obtain pilot data upon which to base a subsequent pivotal study of the investigation device, state this and provide a clinical justification for the sample size selected. (Regulatory reference: ICH E:6, Section 6.9.2) Minimum Suggested Information Outcome data and data analysis Describe the specific observations and/or measurements that will form the basis for evaluating the primary and, if applicable, secondary endpoints or outcomes of the clinical study. (Regulatory reference: ICH E:6, Section 6.7.1 & 6.8.1) Efficacy analysis Describe the analysis population(s) and statistical methods that will be employed in the analysis (analyses) of primary and secondary (if any) endpoints related to evaluation(s) of the efficacy of the study treatment or diagnostic product(s). Include the level(s) of significance to be used. (Regulatory reference: ICH E:6, Section 6.7.2) Safety analysis Describe the analysis population(s) and statistical methods that will be employed in the analysis of the safety of the study treatment or diagnostic product(s). Include the level of significance to be used. (Regulatory reference: ICH E:6, Section 6.9.3) Page 8 of 12 Interim analysis If applicable Incorporate only if an interim analysis is planned. Describe the timing and nature of the planned interim analysis. Address corresponding procedures; such as who will perform the interim analysis and to whom the results of the analysis will be provided. (Regulatory reference: ICH E:6, Section .9.1) Data and Safety Monitoring (DSM) Plan Data and Safety Monitoring (DSM) Plan Describe the Data and Safety Monitoring Plan. If a Data Safety Monitoring Committee/Board will provide oversight, describe the composition and operations or include DSM Charter as a referenced attachment (i.e., Appendix ___). (Regulatory reference: Johns Hopkins 103.6c Organization Policy on Data & Safety Monitoring of Proposed Research and 21 CFR 312.50) Minimum Suggested Information Early stopping rules Describe the early stopping rules of the trial. (Regulatory reference: ICH E:6, Sections 6.4.6 & 6.5.3) Study Interruption or withdrawal Include any potential reasons for interruption or discontinuation of the protocol. (Regulatory reference: ICH E:6, Section 6.9.4) Risk Analysis Anticipated risks Describe all increased risks to which the subjects (patients-subjects and normal controls, if applicable) will be exposed as a result of their participation in the clinical study. Address the steps that will be taken to minimize these risks. Provide an analysis of the benefitto-risk ratio of study participation (i.e., for each of the study populations, as applicable) and a corresponding justification for conducting the clinical study. (Regulatory reference: ICH E: 6, Section 6.2.3) Minimum Suggested Information Adverse event recording/ reporting Detail specific adverse event definitions (e.g. unanticipated adverse device effect (UDAE), unexpected adverse effect, serious adverse effect, adverse effect, etc.) (Regulatory reference: ICH E:6, Section 4.11) Eliciting adverse effect information Detail specifically how adverse effect information will be elicited from study participants. (Regulatory reference: ICH E:6, Section 6.8.3) Page 9 of 12 Recording and assessment of adverse effects Specifically describe here what criteria will be used in order to classify an abnormal test finding as an adverse effect (e.g. the test finding is accompanied by clinical symptoms, the test finding necessitates additional diagnostic evaluations or interventions, the test finding leads to a change in study dosing or exposure or discontinuation of subject participation, the test finding is considered an adverse effect by the Sponsor-Investigator, etc.) Detail specifically how adverse effect information will be documented (e.g. in research chart) and plan to ensure that sufficient information will be pursued as to permit adequate determination of the outcome of the effect and assessment of the causal nature of the relationship between the investigational device and or other study treatment/products. (Regulatory reference: ICH E:6, Section 6.8.2 & 6.8.3) Assessment of causality and severity Describe here the process to be followed by the sponsor-investigator for review of documented adverse effects and abnormal test findings in order to determine classification as an adverse effect, whether or not the adverse effect was caused by the investigational device or other study treatment, or if the adverse effect meets the criteria for a serious adverse effect. Additionally, describe how determinations of causality that are “unknown” and/or “questionable” in relation to the investigational device will be addressed, documented and reported. Reporting of adverse effects to the FDA If the sponsor-Investigator will report any observed or volunteered adverse effects determined to be an unanticipated adverse device effect to the FDA (e.g. via FDA Form 3500 (for voluntary reporting), FDA Form 3500A (required reporting) describe the process for initial reporting, follow up, and notification of co-investigators. (Regulatory reference: http://www.fda.gov/Safety/MedWatch/HowToReport/ucm085568.htm and ICH E:6, Section 6.8.3) Reporting of adverse effects to the responsible IRB Describe the process to be followed for reporting of adverse effects to the IRB and time frames in which this will be done. (Regulatory reference: 103.6b Organization Policy on Reports of Unanticipated Problems Involving Risks to Participants or Others and ICH E:6, Section 6.8.3)) Monitoring Monitoring procedures Minimum Suggested Information Describe the nature and timing of any quality control/quality assurance reviews (i.e., independent of the previously described monitoring activities) that will be undertaken by the Sponsor-Investigator to ensure appropriate conduct of the clinical study and quality and completeness of the accrued study data. I.e., describe the data and safety monitoring plan for the clinical study as outlined in the IRB application or include DSM plan/charter in the appendices and reference same here. (Regulatory reference: ICH E:6, Section 6.11 and 21 CFR 312.56) Page 10 of 12 Additional Records and Reports Data handling and record-keeping Describe the procedures for management and retention of study data including accounting for any missed, unused, and/or spurious data. In appendices, include a copy of Case Report Forms (CRF) and reference “See Appendix__. Minimum Suggested Information (Regulatory reference ICH E:6, Sections 5.5 & 6.13) Record maintenance and retention Describe how the subject-specific data and Case Report Forms will be coded and how these materials, and the subject identification code list, will be stored so as to protect the subjects confidentiality. Specify that subject names or other directly identifiable information will not appear on any reports, publications, or other disclosures of clinical study outcomes (Regulatory reference ICH E:6, Sections 5.5 & 6.13) Dissemination of Results and Publication Policy Optional information The investigator may consider adding information describing the dissemination of results and publication policy. When describing this section, include specific criteria set forth by the funding agency, contracts with sponsor, and/or institutional polices. Additionally, the investigator can also include information on Clinicaltrials.gov registration and result reporting requirements, if applicable. References Minimum Suggested Information List all references cited throughout the protocol. Where possible include DOI (Digital Object Identifier) number, PMID (PubMed ID number), and/or PMCID (PubMed Central ID number) as this may make it easier for reviewers to find electronic copies of publications if they want to review the paper. (Regulatory reference ICH E:6, Section 6.2.7) Appendices If applicable Appendices can include but not limited to Site roster, Schedule of events, lab processing procedures, case report forms, package inserts, manual of procedures, advertisements, patient education materials, study diaries, behavioral evaluations/tests, or other signification information. Page 11 of 12 4.0 FDA GUIDANCE INFORMATION Below are links to a number of FDA guidance documents and FDA guidance sites that may be useful with regard to choice of study design and drafting of a clinical protocol involving use of an investigational drug. FDA Guidance Documents on Clinical Pharmacology: http://www.fda.gov/Drugs/GuidanceComplianceRegulatoryInformation/Guidances/ucm064982.htm FDA Guidance Documents on Clinical / Medical: http://www.fda.gov/Drugs/GuidanceComplianceRegulatoryInformation/Guidances/ucm064981.htm FDA Guidance Documents on Biopharmaceutics: http://www.fda.gov/Drugs/GuidanceComplianceRegulatoryInformation/Guidances/ucm064964.htm FDA Guidance Documents on Drug Safety: http://www.fda.gov/Drugs/GuidanceComplianceRegulatoryInformation/Guidances/ucm064993.htm FDA Guidance Documents on International Conference on Harmonisation – Efficacy: http://www.fda.gov/Drugs/GuidanceComplianceRegulatoryInformation/Guidances/ucm065004.htm FDA Guidance Document: Collection of Race and Ethnicity Data in Clinical Trials http://www.fda.gov/cder/guidance/5656fnl.htm International Committee on Harmonization (ICH) E: 6 Good Clinical Practices http://www.ich.org/fileadmin/Public_Web_Site/ICH_Products/Guidelines/Efficacy/E6_R1/Step4/E6_R1__ Guideline.pdf Page 12 of 12