Gulf War deployment-related exposures and health outcomes at
advertisement

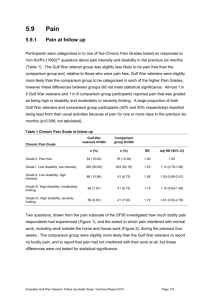
5.26 Gulf War deployment-related exposures and health outcomes at follow up The associations between Gulf War-deployment related exposures and health outcomes at follow up are shown in the following Tables. The association between taking PB during the Gulf War and health outcomes at follow up are shown in Table 1, which indicates that there are some statistically significant associations between use of PB and number of health symptoms, multisymptom illness and IBS at follow up. Those participants who were categorised as having ‘high uptake’ PB exposure based on their deployment group, had an increased risk of IBS at follow up compared to those who were categorised as ‘low uptake’ PB exposure based on their deployment group. Using self-reported PB exposure categories, Gulf War veterans who reported taking ‘any’ number of PB tablets, and those who reported taking 1-80 PB tablets, also had a greater risk of having IBS at follow up, compared to Gulf War veterans who reported that they did not take any PB tablets. Gulf War veterans who reported taking ‘any’ number of PB tablets, also those who reported taking 81-180 PB tablets, or >180 PB tablets, had a higher health symptom count on average compared to Gulf War veterans who reported no PB tablets. Gulf War veterans who reported that they did not know whether they took PB tablets or not, however, also had a higher health symptom count on average compared to Gulf War veterans who reported no PB tablets. Gulf War veterans who reported taking 81-180 PB tablets were at increased risk of multisymptom illness compared with Gulf War veterans who reported none. The association between number of vaccinations received as part of the Gulf War deployment and health outcomes at follow up are shown in Table 2. Table 2 indicates that there are some statistically significant associations between self-reported numbers of Gulf War vaccinations and SF-12 defined physical health status, average health symptom count, average neuropathic symptom count, risk of multisymptom illness and risk of chronic fatigue. Compared with Gulf War veterans who reported receiving no vaccinations, those who reported 10 or more vaccinations had a significantly higher average health symptom and neuropathic symptom count, a higher risk of multisymptom illness and a higher risk of chronic fatigue. For every increment of one vaccine reported to be received during the Gulf War, there was on average a 1.03-fold increase in average health symptom count, a 10% increase in risk of multisymptom illness and a 16% increase in risk of chronic fatigue. Australian Gulf War Veterans’ Follow Up Health Study: Technical Report 2015 Page 202 The association between anti-malarials taken as part of the Gulf War deployment and health outcomes at follow up are presented in Table 3. There were no clear associations between anti-malarials and health outcomes at follow up. Compared with Gulf War veterans who reported no anti-malarials, those who reported ‘any’ anti-malarials and those who did not know whether they took anti-malarials or not, both had a slightly higher health symptom count and neuropathic symptom count on average. There were no associations between anti-malarials and any of the other health outcomes shown in Table 3. The association between exposure to pesticides during the Gulf War deployment and health outcomes at follow up are presented in Table 2. Based on self-reported exposure to pesticides, but not possible exposure based on deployment group, there were statistically significant associations between pesticide exposure and poorer SF12 physical health status, higher average health symptom count, higher risk of multisymptom illness and higher risk of chronic fatigue. Compared to Gulf War veterans who reported no Gulf War-related pesticide exposure, veterans who reported pesticide exposure scored an average of three points lower on the SF12 PCS, approximately 1.3 times higher on their health symptom count, and had approximately double the risk of multisymptom illness and chronic fatigue. The association between exposure to intense smoke, and SMOIL, during the Gulf War deployment and health outcomes at follow up are presented in Table 5 and Table 6 respectively. There was no association between deployment-based exposure to intense smoke and any of the health outcomes in Table 5, including asthma and chronic bronchitis at follow up. Relative to Gulf War veterans who reported no SMOIL exposure, veterans who reported any, low or high SMOIL exposure had lower SF12 PCS scores and higher health symptom counts. For every increase in reported SMOIL exposure category from ‘none’ to ‘low’ to ‘high’, SF12 PCS score decreased by an average of 2.1 points and there was a 1.2fold increase in average health symptom count. There was also a marginally significant association between reported low SMOIL exposure and increased risk of IBS, however there was no association between reported high SMOIL exposure and IBS and there was no dose response association. As presented in Table 7, there were no statistically significant associations between likely exposure to oil in water during the Gulf War deployment, based on deployment group, and SF12 physical health status, average health symptom count and ROME III-defined IBS at follow up. The associations between exposure to dust during the Gulf War deployment and health outcomes at follow up are presented in Table 8. There was no clear pattern to the Australian Gulf War Veterans’ Follow Up Health Study: Technical Report 2015 Page 203 associations between dust and health outcomes at follow up. Self-reported exposure to dust during the Gulf War, but not exposure level based on deployment group, was associated with poorer physical health status at follow up and higher average health symptom count. However, high dust exposure based on deployment group, relative to low dust exposure, was associated with lower risk of symptom-based chronic bronchitis. There was no association between Gulf War-related dust exposure and doctor-confirmed asthma at follow up. Australian Gulf War Veterans’ Follow Up Health Study: Technical Report 2015 Page 204 Table 1 Association between use of PB during the Gulf War and health outcomes at follow up in Gulf War veterans Level of PB exposure Health symptom count SF12 PCS score Neuropathic symptom Multisymptom illness count (N=203) Chronic fatigue (N=86) CFQ case (N=232) Rome III IBS case (N=90) Mean (sd) Adj diff (95% CI) Mean (sd) Adj ratio* (95% CI) Mean (sd) Adj ratio† (95% CI) n (%) Adj RR (95% CI) n (%) Adj RR (95% CI) n (%) Adj RR (95% CI) n (%) Adj RR (95% CI) Low uptake 46.9 (10.5) 0.0 16.1 (11.1) 1.0 2.1 (2.8) 1.0 92 (26.9) 1.0 42 (12.2) 1.0 113 (32.9) 1.0 34 (10.2) 1.0 High uptake 46.5 (10.1) -0.54 (-2.2,1.2) 17.8 (12.4) 1.1 (<1.0-1.2) 2.3 (3.1) 0.9 (0.7-1.2) 111 (31.6) 1.2 (0.9-1.6) 44 (12.5) 0.9 (0.6-1.4) 119 (33.8) 1.0 (0.8-1.2) 56 (16.4) 1.7 (1.1-2.7) None 47.4 (10.5) 1.0 1.7 (2.5) 1.0 48 (24.4) 1.0 20 (10.2) 1.0 54 (27.4) 1.0 17 (8.9) 1.0 Any 46.7 (10.0) -1.0 (-3.0,1.0) 18.1 (12.3) 1.3 (1.1-1.5) 2.3 (3.1) 1.2 (0.9-1.6) 110 (31.4) 1.3 (<1.0-1.9) 45 (14.3) 1.1 (0.7-1.9) 121 (34.6) 1.2 (0.9-1.6) 55 (16.2) 1.9 (1.1-3.3) 1-80 tablets 48.0 (9.0) 0.2 (-2.4, 2.8) 15.2 (11.6) 1.1 (0.9-1.4) 1.6 (2.2) 0.9 (0.6-1.4) 24 (28.9) 1.3 (0.8-2.0) 8 (9.6) 1.0 (0.5-2.1) 25 (30.1) 1.1 (0.7-1.6) 13 (16.5) 2.2 (1.1-4.8) 81-180 tablets 46.6 (9.4) -1.3 (-4.0, 1.4) 18.5 (12.5) 1.4 (1.1-1.7) 2.4 (3.0) 1.0 (0.6-1.5) 28 (37.8) 1.7 (1.1-2.6) 11 (14.9) 1.4 (0.7-2.8) 26 (35.1) 1.2 (0.8-1.8) 11 (15.1) 1.9 (0.9-4.0) >180 tablets 46.9 (11.0) -1.0 (-4.4, 2.4) 17.9 (12.4) 1.3 (1.1-1.6) 2.2 (3.2) 1.1 (0.7-1.8) 21 (32.8) 1.5 (0.9-2.4) 8 (12.5) 1.1 (0.5-2.6) 24 (37.5) 1.3 (0.8-2.0) 8 (12.9) 1.5 (0.6-3.7) 1.05 (0.83-1.34) - 1.03 (0.67-1.61) - 1.04 (0.82-1.32) - 0.86 (0.56-1.32) 1.5 (0.8-2.6) 57 (38.8) 1.4 (>1.0-1.9) 18 (12.7) 1.5 (0.8-3.2) Deploymentbased metric Self-report based metric Dose response§ Don’t know‡ - 0.0 14.0 (11.1) -0.42 (-2.19, 1.35) - 1.08 (0.97-1.22) 45.7 (10.7) -2.5 (-4.9, 0.02) 18.2 (10.8) 1.3 (1.1-1.6) 2.7 (3.2) 1.12 (0.89-1.40) - 1.4 (1.1–2.0) 45 (31.3) 1.4 (<1.0-2.1) 21 (14.3) * Calculated using negative binomial regression † Calculated using zero inflated negative binomial regression due to the approximately 40% of participants with no neuropathic symptoms. Adjusted for age (<20; 20-24; 25-34; >=35 years), service branch (Navy; Army; Air Force) and rank (CO, NCO, enlisted ranks) each estimated as at August 1990, and alcohol (AUDIT score > 10) and self-reported doctor-diagnosed diabetes ‡ Reference category is those who reported ‘none’ § Dose response per categorical increase in number of PB tablets taken in those who reported taking at least one Australian Gulf War Veterans’ Follow Up Health Study: Technical Report 2015 Page 205 Table 2 Association between vaccinations for the Gulf War deployment and health outcomes at follow up in Gulf War veterans Level of vaccination exposure SF12 PCS score Health symptom count Neuropathic symptom count Multisymptom illness (N=203) Chronic fatigue (N=117) Mean (sd) Adj diff (95% CI) Mean (sd) Adj ratio* (95% CI) Mean (sd) Adj ratio† (95% CI) n (%) Adj RR (95% CI) n (%) Adj RR (95% CI) Low 46.4 (10.1) 0.0 16.6 (11.1) 1.0 2.3 (3.0) 1.0 47 (30.0) 1.0 22 (13.8) 1.0 Medium 46.9 (10.4) 0.7 (-2.9, 3.0) 15.6 (10.9) 1.0 (0.8-1.2) 1.9 (2.4) 1.1 (0.7-1.6) 36 (27.3) 1.0 (0.6-1.5) 15 (11.4) 1.1 (0.5-2.4) High 46.7 (10.4) 0.5 (-1.4, 2.3) 17.5 (12.2) 1.0 (0.9-1.2) 2.3 (3.1) 1.0 (0.8-1.3) 120 (29.8) 1.0 (0.7-1.3) 49 (12.1) 0.8 (0.5-1.3) None 45.7 (11.1) 0.0 16.9 (12.0) 1.0 2.1 (3.0) 1.0 31 (27.4) 1.0 15 (13.3) 1.0 Any 47.7 (9.8) 1.7 (-0.6, 4.0) 15.8 (11.4) 0.9 (0.8-1.1) 2.0 (2.6) 1.0 (0.8-1.4) 117 (27.6) 1.1 (0.8-1.5) 49 (11.5) 0.9 (0.5-1.5) 1-4 48.4 (9.6) 2.3 (-0.2, 4.8) 14.4 (10.4) 0.9 (0.7-1.0) 1.6 (2.2) 1.0 (0.7-1.4) 35 (20.6) 0.8 (0.5-1.2) 16 (9.4) 0.7 (0.4-1.4) 5-9 48.0 (9.8) 1.8 (-0.6, 4.3) 15.8 (11.3) 0.9 (0.8-1.1) 1.9 (2.6) 1.0 (0.7-1.4) 64 (29.1) 1.1 (0.8-1.7) 22 (10.0) 0.8 (0.4-1.4) 10 or more 43.0 (9.8) -3.0 (-7.1, 1.0) 23.3 (14.4) 1.4 (1.1-1.7) 1.9 (2.6) 1.8 (1.1-2.9) 18 (52.9) 2.1 (1.3-3.3) 11 (32.4) 2.5 (1.2-5.0) - -0.39 (-0.80, 0.01) - 1.03 (1.01-1.06) - not computed - 1.10 (1.03-1.16) - 1.16 (1.05-1.28) Don’t know‡ 44.5 (10.7) -1.3 (-4.3, 1.7) 19.9 (11.9) 1.1 (0.9-1.3) 3.0 (3.7) 1.3 (0.9-1.9) 54 (35.1) 1.3 (0.9-2.0) 22 (14.2) 1.0 (0.5-1.9) No clustering 47.0 (10.2) 0.0 16.3 (11.5) 1.0 2.0 (2.7) 1.0 135 (27.9) 1.0 57 (11.8) 1.0 Any clustering 47.9 (9.8) 0.5 (-1.9, 2.9) 16.1 (12.1) 1.01 (0.8-1.2) 2.0 (3.0) 1.1 (0.7-1.5) 20 (27.4) 1.0 (0.7-1.5) 11 (15.1) 1.4 (0.8-2.6) Deployment-based metric Self-report based metric Dose response§ * Calculated using negative binomial regression † Calculated using zero inflated negative binomial regression due to the approximately 40% of participants with no neuropathic symptoms. Adjusted for age (<20; 20-24; 25-34; >=35 years), service branch (Navy; Army; Air Force) and rank (CO, NCO, enlisted ranks) each estimated as at August 1990, and alcohol (AUDIT score > 10) and self-reported doctor-diagnosed diabetes ‡ Reference category is those who reported ‘none’ § Dose response per unit increase in number of vaccinations in those who received at least one Australian Gulf War Veterans’ Follow Up Health Study: Technical Report 2015 Page 206 Table 3 Association between anti-malarial tablets taken during the Gulf War deployment and health outcomes at follow up in Gulf War veterans Level of antimalarial exposure Self-report based metric None Any Don’t know‡ SF12 PCS score Health symptom count Neuropathic symptom count Multisymptom illness (N=203) Chronic fatigue (N=117) Mean (sd) Adj diff (95% CI) Mean (sd) Adj ratio* (95% CI) Mean (sd) Adj ratio† (95% CI) n (%) Adj RR (95% CI) n (%) Adj RR (95% CI) 48.2 (9.7) 46.1 (10.9) 0.0 -1.6 (-3.6, 0.5) 14.6 (11.0) 17.7 (12.5) 1.0 1.2 (>1.0-1.3) 1.6 (2.3) 2.4 (3.2) 1.0 1.5 (1.1-2.0) 42 (25.9) 88 (31.8) 1.0 1.2 (0.9-1.6) 13 (8.0) 43 (15.5) 1.0 1.8 (<1.0-3.3) 46.3 (10.0) -1.7 (-3.8, 0.4) 17.5 (11.2) 1.2 (>1.0-1.4) 2.4 (3.0) 1.5 (1.1-2.0) 72 (28.8) 1.1 (0.8-1.5) 30 (12.0) 1.4 (0.7-2.6) * Calculated using negative binomial regression † Calculated using zero inflated negative binomial regression due to the approximately 40% of participants with no neuropathic symptoms. Adjusted for age (<20; 20-24; 25-34; >=35 years), service branch (Navy; Army; Air Force) and rank (CO, NCO, enlisted ranks) each estimated as at August 1990, and alcohol (AUDIT score > 10) and self-reported doctor-diagnosed diabetes ‡ Reference category is those who reported ‘none’ Table 4 Association between exposure to pesticides during the Gulf War and health outcomes at follow up in Gulf War veterans Level of exposure to pesticides Deployment-based metric Unlikely Possible Self-report based metric No Yes SF12 PCS score Health symptom count Neuropathic symptom count Multisymptom illness (N=203) Chronic fatigue (N=117) Mean (sd) Adj diff (95% CI) Mean (sd) Adj ratio* (95% CI) Mean (sd) Adj ratio† (95% CI) n (%) Adj RR (95% CI) n (%) Adj RR (95% CI) 46.8 (10.3) 44.3 (10.9) 0.0 -0.5 (-5.2, 4.3) 16.8 (11.7) 19.5 (13.6) 1.0 1.0 (0.7-1.4) 2.2 (2.9) 3.1 (4.0) 1.0 1.0 (0.6-1.8) 193 (29.1) 10 (33.3) 1.0 0.7 (0.4-1.4) 80 (12.0) 6 (20.7) 1.0 1.8 (0.7-4.5) 47 7 (9.8) 43.9 (11.0) 0.0 -3.1 (-5.0, -1.2) 15.5 20.8 1.0 1.3 (1.1-1.5) 2.0 (2.8) 2.9 (3.4) 1.0 1.1 (0.9-1.4) 120 (23.7) 79 (44.1) 1.0 1.8 (1.4-2.3) 47 (9.3) 39 (21.7) 1.0 2.3 (1.6-3.5) * Calculated using negative binomial regression † Calculated using zero inflated negative binomial regression due to the approximately 40% of participants with no neuropathic symptoms. Adjusted for age (<20; 20-24; 25-34; >=35 years), service branch (Navy; Army; Air Force) and rank (CO, NCO, enlisted ranks) each estimated as at August 1990, and alcohol (AUDIT score > 10) and self-reported doctor-diagnosed diabetes Australian Gulf War Veterans’ Follow Up Health Study: Technical Report 2015 Page 207 Table 5 Association between intense smoke exposure during the Gulf War and health outcomes at follow up in Gulf War veterans Level of smoke exposure SF12 PCS score Mean (sd) Adj diff (95% CI) Health symptom count Mean (sd) Adj ratio* (95% CI) Rome III IBS case (N=90) Self-reported doctor Symptom-based-Chronic confirmed Asthma (N=87) bronchitis (N=144) Adj RR (95% CI) n (%) n (%) Adj RR† (95% CI) n (%) Adj RR† (95% CI) Deployment-based metric Low High 46.6 (10.2) 0.0 17.0 (11.9) 1.0 85 (13.8) 1.0 81 (12.7) 1.0 133 (20.9) 1.0 47.2 (11.4) 0.6 (-2.6, 3.7) 16.1 (10.1) 0.9 (0.8-1.1) 5 (8.9) 0.6 (0.3-1.5) 5 (9.3) 0.7 (0.3-1.5) 11 (19.6) 1.0 (0.6-1.8) * Calculated using negative binomial regression † Adjusted for age (<20; 20-24; 25-34; >=35 years), service branch (Navy; Army; Air Force) and rank (CO, NCO, enlisted ranks) each estimated as at August 1990, atopy at baseline and current smoking status (never; former; current smoker) Table 6 Association between SMOIL exposure during the Gulf War and health outcomes at follow up in Gulf War veterans Level of SMOIL exposure SF12 PCS score Mean (sd) Adj diff (95% CI) Health symptom count Mean (sd) Adj ratio* (95% CI) Rome III IBS case (N=90) Self-reported doctor Symptom-based-Chronic confirmed Asthma (N=87) bronchitis (N=144) Adj RR (95% CI) n (%) n (%) Adj RR† (95% CI) Self-report based metric None Any Low High Dose response§ n (%) Adj RR† (95% CI) 48.3 (9.5) 0.0 14.9 (10.3) 1.0 34 (10.7) 1.0 35 (10.7) 1.0 60 (18.3) 1.0 -2.9 (-4.4, -1.4) 1.2 (1.1-1.4) 45.3 (10.8) 18.8 (12.8) 55 (15.7) 1.4 (<1.0-2.2) 50 (14.0) 1.3 (0.8-1.9) 82 (22.9) 1.2 (0.8-1.6) -2.8 (-4.4, -1.2) 1.2 (1.1-1.3) 1.5 (>1.0-2.3) 45.3 (10.8) 18.4 (12.6) 49 (16.8) 39 (13.2) 1.2 (0.7-1.8) 65 (22.0) 1.1 (0.8-1.6) -3.4 (-6.4, -0.5) 1.4 (1.1-1.6) 45.3 (10.8) 20.5 (13.4) 6 (10.2) 0.9 (0.4-2.1) 11 (18.0) 1.7 (0.9-3.1) 17 (27.4) 1.6 (<1.0-2.6) -2.14 (-3.33, -0.94) 1.18 (1.10-1.28) 1.17 (0.89-1.55) 1.26 (0.93-1.71) 1.22 (0.96-1.55) * Calculated using negative binomial regression † Adjusted for age (<20; 20-24; 25-34; >=35 years), service branch (Navy; Army; Air Force) and rank (CO, NCO, enlisted ranks) each estimated as at August 1990, atopy at baseline and current smoking status (never; former; current smoker) § Dose response per categorical increase in SMOIL where participants are categorised as either “none’, “low” or “high” Table 7 Association between exposure to oil in water during the Gulf War and health outcomes at follow up in Gulf War veterans Level of exposure to oil in water SF12 PCS score Mean (sd) Deployment-based metric Unlikely Possible Adj diff (95% CI) 46.8 (10.4) 0.0 46.1 (10.1) -0.9 (-2.8, 1.0) * Calculated using negative binomial regression Health symptom count Rome III IBS case Mean (sd) Adj ratio* (95% CI) n (%) Adj RR (95% CI) 16.7 (11.5) 17.8 (12.8) 1.0 1.0 (0.9-1.2) 65 (12.4) 25 (16.8) 1.0 1.3 (0.8-2.1) Australian Gulf War Veterans’ Follow Up Health Study: Technical Report 2015 Page 208 Table 8 Association between dust exposure during the Gulf War and health outcomes at follow up in Gulf War veterans Level of dust exposure Deployment-based metric Low High Self-report based metric Absent Present SF12 PCS score Health symptom count* Self-reported doctor confirmed Asthma (N=87) Symptom-based-Chronic bronchitis (N=144) Mean (sd) Adj diff (95% CI) Mean (sd) Adj diff (95% CI) n (%) Adj RR† (95% CI) n (%) Adj RR† (95% CI) 46.7 (10.2) 46.7 (10.3) 0.0 -0.1 (-1.9, 1.7) 16.6 (10.8) 17.1 (12.1) 1.0 1.0 (0.9-1.2) 24 (13.1) 62 (12.2) 1.0 1.0 (0.6-1.5) 52 (63.4) 92 (45.5) 1.0 0.7 (0.6-0.9) 48.0 (9.6) 0.0 15.4 (10.5) 1.0 46 (12.5) 1.0 68 (46.3) 1.0 -2.9 (-4.4, -1.3) 1.2 (1.1-1.4) 45.1 (11.0) 18.7 (12.9) 39 (12.4) 1.1 (0.7-1.6) 76 (56.3) 1.3 (<1.0-1.6) * Calculated using negative binomial regression † Adjusted for age (<20; 20-24; 25-34; >=35 years), service branch (Navy; Army; Air Force) and rank (CO, NCO, enlisted ranks) each estimated as at August 1990, atopy at baseline and current smoking status (never; former; current smoker) Australian Gulf War Veterans’ Follow Up Health Study: Technical Report 2015 Page 209 Table 9 shows that there was no statistically significant association between possible exposure to gastroenteritis outbreaks during the Gulf War, based on deployment group, and ROME III-defined IBS at follow up. Table 9 Association between possible exposure to gastroenteritis outbreaks during the Gulf War and health outcomes at follow up in Gulf War veterans Level of exposure to gastroenteritis outbreak Deployment-based metric Unlikely Possible Rome III IBS case (N=90) n (%) Adj RR (95% CI) 28 (10.9) 62 (14.8) 1.0 1.3 (0.8-2.0) Table 10 shows the associations between Gulf War deployment era, and MSEQ score, with health outcomes at follow up. Compared with those Gulf War veterans whose deployment ended prior to the combat phase of the Gulf War, veterans whose deployment included the combat phase had a higher risk of multisymptom illness, alcohol disorder as measured by AUDIT caseness, 12 month major depression and a higher average health symptom count (for the latter two health outcomes the differences only just met statistical significance). Gulf War veterans whose deployment commenced after the combat phase were at greater risk of 12 month alcohol disorder compared to Gulf War veterans whose deployment ended prior to the combat phase. Increasing number of reported Gulf War-related stressors, as indicated by increasing MSEQ score, was strongly associated with decreased SF12 mental health status score, increased average health symptom and neuropathic symptom count, increased depressive symptom severity score, and increased risk of multisymptom illness, chronic fatigue, 12 month major depression, 12 month PTSD, alcohol disorder as measured by AUDIT caseness (the association with CIDI-defined alcohol disorder was only marginal), and psychological distress as measured by GHQ-12 caseness. The greatest risk was amongst those who reported 12 or more Gulf War-related stressors. Those Gulf War veterans were at six times greater risk of multisymptom illness, five times greater risk of 12 month PTSD, three times greater risk of 12 month major depression and irritable bowel syndrome, and double the risk of chronic fatigue, for example, compared with those veterans who reported four or fewer Gulf Warrelated stressors. Every increase in MSEQ score of one Gulf War-related stressor was associated with increased morbidity on a number of measured outcomes including a 13% increase in 12 month PTSD, a 9% increase in multisymptom illness, a 7% increase in chronic fatigue and a 6% increase in 12 month major depression. Australian Gulf War Veterans’ Follow Up Health Study: Technical Report 2015 Page 210 Table 10 Association between Gulf War deployment era and MSEQ score with health outcomes at follow up in Gulf War veterans Gulf War deployment exposure SF12 MCS score Health symptom count Neuropathic symptom count Multisymptom illness (N=203) Chronic fatigue (N=86) Irritable Bowel Syndrome (N=90) Adj ratio† (95% CI) n (%) Adj RR (95% CI) n (%) Adj RR (95% CI) n (%) Adj RR (95% CI) 2.1 (2.9) 1.0 44 (22.5) 1.0 27 (13.7) 1.0 17 (9.0) 1.00 1.1 (>1.0-1.3) 2.3 (3.0) 0.9 (0.7 – 1.1) 133 (32.0) 1.4 (1.1-1.9) 48 (11.5) 0.8 (0.5-1.3) 61 (15.0) 1.65 (0.99-2.73) 1.0 (0.9-1.2) 2.1 (3.0) 0.8 (0.5 – 1.3) 26 (32.1) 1.3 (0.8-2.0) 11 (13.6) 0.9 (0.5-1.8) 12 (15.2) 1.58 (0.82-3.06) 10.3 (8.4) 1.0 1.1 (1.8) 1.0 14 (9.0) 1.0 13 (8.4) 1.0 10 (6.5) 1.00 14.9 (9.7) 1.5 (1.3-1.7) 1.7 (2.7) 1.2 (0.9 – 1.7) 43 (20.9) 2.4 (1.3-4.2) 19 (9.2) 1.0 (0.5-2.0) 24 (12.1) 1.88 (0.91-3.87) 19.5 (12.4) 1.9 (1.6-2.2) 2.9 (3.4) 1.7 (1.2 – 2.4) 62 (35.6) 4.0 (2.3-6.8) 21 (12.0) 1.3 (0.7-2.6) 29 (17.2) 2.65 (1.31-5.37) -10.3 (-12.9, -7.8) 23.3 (12.3) 2.3 (2.0-2.7) 3.1 (3.3) 1.9 (1.4 – 2.8) 84 (53.5) 6.1 (3.6-10.4) 33 (20.9) 2.3 (1.2-4.3) 27 (17.7) 2.86 (1.42-5.77) -0.72 (-.08, -0.56) - 1.06 (1.05-1.07) - 1.05 (1.03-1.09) Mean (sd) Adj diff (95% CI) Mean (sd) Adj ratio* (95% CI) Mean (sd) before combat 46.6 (11.1) 0.0 15.5 (11.0) 1.0 during combat 45.7 (12.3) -0.5 (-2.5, 1.5) 17.6 (12.1) after combat 46.9 (11.4) -0.0 (-3.0, 2.9) 17.1 (11.8) 51.2 (9.3) 0.0 5-8 47.5 (11.0) -3.8 (-6.0, -1.7) 9-12 44.6 (12.3) -6.9 (-9.3, -4.5) >12 40.9 (12.4) - Deployment era MSEQ score 0-4 Dose response‡ Gulf War deployment exposure 12 month Major depression (N=63) n (%) Deployment era before combat during combat after combat MSEQ score 0-4 5-8 9-12 >12 Dose response† PHQ-9 depressive symptom score Adj RR (95% CI) Median (IQR) 1.04 (1.02 – 1.07) - 12 month PTSD (N=47) Adj diff (95% CI) n (%) Adj RR (95% CI) - 1.09 (1.08-1.11) 12 month Alcohol disorder (N=40) n (%) Adj RR (95% CI) - 1.07 (1.04-1.10) AUDIT case (N=199) n (%) Adj RR (95% CI) GHQ-12 case (N=264) n (%) Adj RR (95% CI) 11 (6.1) 1.0 3 (1-6) 0.0 10 (5.5) 1.0 5 (2.8) 1.0 42 (21.5) 1.0 81 (41.1) 1.0 46 (11.9) 1.9 (>1.0-3.6) 4 (0-8) 1 (-0.1-2.1) 32 (8.3) 1.4 (0.7-2.8) 27 (7.0) 2.4 (0.9-6.4) 134 (32.4) 1.5 (1.1-2.0) 155 (37.4) 0.9 (0.7-1.1) 6 (7.5) 1.3 (0.5-3.8) 4 (1-7) 1 (-0.7, 2.7) 5 (6.3) 0.7 (0.2-2.3) 8 (10.0) 3.5 (1.1-10.9) 23 (28.1) 1.4 (0.9-2.2) 28 (34.2) 0.8 (0.6-1.2) 7 (4.8) 1.0 1 (0-4) 0.0 0 - 5 (3.5) 1.0 33 (21.3) 1.0 36 (23.2) 1.0 17 (8.7) 1.9 (0.8-4.4) 3 (0-6) 1 (-0.3-2.3) 11 (5.6) 1.0§ 10 (5.1) 1.4 (0.5-4.1) 50 (24.3) 1.1 (0.7-1.6) 73 (35.3) 1.5 (1.1-2.2) 16 (10.1) 2.2 (0.9-5.2) 4 (2-8) 2 (0.6-3.4) 12 (7.6) 2.2 (>1.0-4.9) 11 (7.0) 1.9 (0.7-5.5) 58 (33.5) 1.5 (1.1-2.2) 75 (42.9) 1.9 (1.3-2.6) 23 (15.6) 3.2 (1.4-7.4) 7 (3-12) 5 (3.6-6.4) 24 (16.3) 4.6 (2.3-9.1) 14 (9.5) 2.5 (0.9-6.7) 57 (36.5) 1.6 (1.1-2.4) 80 (51.3) - 0.36 (0.27-0.46) - 1.13 (1.10-1.17) - 1.05 (>1.00-1.10) - 1.06 (1.02-1.09) 1.04 (1.02-1.06) 2.2 (1.6-3.1) 1.04 (1.03-1.06) * Calculated using negative binomial regression † Calculated using zero inflated negative binomial regression due to the approximately 40% of participants with no neuropathic symptoms. Adjusted for age (<20; 20-24; 25-34; >=35 years), service branch (Navy; Army; Air Force) and rank (CO, NCO, enlisted ranks) each estimated as at August 1990, and alcohol (AUDIT score > 10) and self-reported doctor-diagnosed diabetes ‡ The dose response slope is the expected proportionate increase in the adj RR (or adj difff) per unit increase in the MSEQ score § Because there are no PTSD cases with an MSEQ score of 0-4, the reference category for this regression was MSEQ score 0-8 Australian Gulf War Veterans’ Follow Up Health Study: Technical Report 2015 Page 211 5.26.1 Key findings There were a number of statistically significant associations between Gulf War deployment exposures and health outcomes at follow up. Typically, significant associations were found for self-report based-metrics of exposure level rather than metrics based on deployment group. The use of pyridostigmine bromide during the Gulf War was associated with an increased number of health symptoms, multisymptom illness and IBS at follow up. Gulf War veterans who were categorised as having ‘high uptake’ of PB exposure based on their deployment group, compared with ‘low uptake’, and those who reported taking ‘any’ number of PB tablets, or 1-80 PB tablets, compared with none, had a greater risk of having IBS at follow up. Gulf War veterans who reported taking ‘any’ number, 81-180 PB tablets, or >180 PB tablets, had a higher health symptom count on average compared to veterans who reported no PB tablets. Gulf War veterans who reported that they did not know whether they took PB tablets or not, however, also had a higher health symptom count on average compared to veterans who reported no PB tablets. Gulf War veterans who reported taking 81-180 PB tablets were at increased risk of multisymptom illness compared with veterans who reported no PB tablets. Compared with Gulf War veterans who reported receiving no vaccinations, those who reported 10 or more vaccinations as part of the Gulf War deployment had a significantly higher average health symptom and neuropathic symptom count, and a higher risk of multisymptom illness and chronic fatigue at follow up. For every increment of one vaccine reported to be received during the Gulf War, there was a 1.03-fold increase in average health symptom count, a 10% increase in multisymptom illness risk and a 16% increase chronic fatigue risk. Compared to Gulf War veterans who reported no Gulf War-related pesticide exposure, veterans who reported pesticide exposure scored an average of three points lower on the SF12 PCS, approximately 1.3 times higher on their health symptom count, and had approximately double the risk of multisymptom illness and chronic fatigue. Relative to Gulf War veterans who reported no SMOIL exposure, veterans who reported any, low or high SMOIL exposure had lower SF12 PCS scores and higher health symptom counts. For every increase in reported SMOIL exposure category from ‘none’ to ‘low’ to ‘high’, SF12 PCS score decreased by an average of 2.1 points and there was a 1.2-fold increase in average health symptom count. Australian Gulf War Veterans’ Follow Up Health Study: Technical Report 2015 Page 212 There was no clear pattern to the associations between dust and health outcomes at follow up. Self-reported exposure to dust during the Gulf War was associated with poorer physical health status at follow up and higher average health symptom count. However, high dust exposure based on deployment group, relative to low dust exposure, was associated with lower risk of symptom-based chronic bronchitis. There was no association between Gulf War-related dust exposure and doctor-confirmed asthma at follow up. Compared with those Gulf War veterans whose deployment ended prior to the combat phase of the Gulf War, veterans whose deployment included the combat phase had a higher average health symptom count, depressive symptom severity, multisymptom illness risk and major depression risk. Gulf War veterans whose deployment commenced after the combat phase were at greater risk of alcohol disorder compared to veterans whose deployment ended prior to the combat phase. Increasing number of reported Gulf War-related stressors, as indicated by increasing MSEQ score, was associated with decreased mental health status score, and increased average health symptom and neuropathic symptom count, depressive symptom severity, and risk of multisymptom illness, chronic fatigue, major depression, PTSD, AUDIT alcohol disorder and psychological distress at follow up. There were no clear patterns to the associations observed between anti-malarials and health outcomes at follow up. There were no statistically significant associations between deployment-based metrics for likely exposure to oil in water, intense smoke, or possible exposure to gastroenteritis outbreaks during the Gulf War deployment, and health outcomes at follow up. Australian Gulf War Veterans’ Follow Up Health Study: Technical Report 2015 Page 213