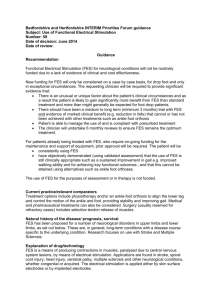
Bedfordshire and Hertfordshire Priorities Forum guidance Subject
advertisement

Bedfordshire and Hertfordshire Priorities Forum guidance Subject: Use of Functional Electrical Stimulation Number: 59 Date of decision: December 2010 Date of review: December 2014 Guidance Overall recommendation Functional Electrical Stimulation for neurological conditions will not be routinely funded due to a lack of evidence of clinical and cost effectiveness. Current practice/relevant comparators Treatment options include physiotherapy or an ankle-foot orthosis to align the lower leg and control the motion of the ankle and foot, providing stability and improving gait. Medical therapy includes oral administration of muscle relaxant drugs or botulinum toxin type A injections. Surgery (usually reserved for refractory cases) includes selective tendon release of muscles. Natural history of the disease/ prognosis, survival FES has been proposed for a number of neurological disorders in upper limbs and lower limbs, as set out below. These are, in general, long-term conditions with a disease course specific to the underlying condition. Explanation of drug/technology FES is a means of producing contractions in muscles, paralysed due to central nervous system lesions, by means of electrical stimulation. Applications are found in stroke, spinal cord injury, head injury, cerebral palsy, multiple sclerosis and other neurological conditions, whether congenital or acquired. The electrical stimulation is applied either by skin surface electrodes or by implanted electrodes. Motor dysfunction in the upper and/or lower limbs is a common complication of a number of neurological disorders. In the upper limb, it can lead to painful subluxation of the shoulder and problems with shoulder, elbow, wrist and hand movement. In the lower limb, drop-foot resulting from peroneal nerve damage causes abnormal gait, reduced walking speed and increased risk of falls. Epidemiology There is no good estimate of the numbers affected in Derbyshire County, but it could be up to 5,000 new patients per year. Evidence of clinical and cost effectiveness There has been a number of trials into the effectiveness of electrical stimulation in limb dysfunction and several recent systematic reviews. All published clinical studies have substantial methodological weaknesses. Positive outcomes have been shown for shoulder pain/subluxation, range of movement and motor function in the upper limb and for walking speed in the lower limb. However, these outcomes were not consistent across all studies and were limited by problems with study design. The significance of some outcomes measured, e.g. walking speed, and their impact on quality of daily life are unclear. Most published evaluations of FES have shown positive results although benefits were often not observed at longer-term follow-up. However, the identified trials are generally small and of low methodological quality. Studies lack descriptions of randomisation methods, blinding and intention-to-treat analyses. They also vary in the patient groups studied and the exact nature of the intervention. Although suggestive at least of short-term benefit, the evidence to date is insufficient to comment reliably on the effectiveness of FES for people with motor dysfunction. There is a lack of studies comparing electrical stimulation with other rehabilitation modalities including various forms of physiotherapy, orthoses and interventions to reduce spasticity. The place of electrical stimulation in pathways for rehabilitation is therefore unclear. It is not currently possible to identify any sub-groups of patients who would derive particular benefit from electrical stimulation compared to other interventions. FES is not mentioned in The National Service Framework for Long-Term Conditions. NICE IPG 278 states that “Current evidence on the safety and efficacy (in terms of improving gait) of functional electrical stimulation (FES) for drop foot of central neurological origin appears adequate to support the use of this procedure provided that normal arrangements are in place for clinical governance, consent and audit. 1.2 Patient selection for implantable FES for drop foot of central neurological origin should involve a multidisciplinary team specialising in rehabilitation. 1.3 Further publication on the efficacy of FES would be useful, specifically including patient-reported outcomes, such as quality of life and activities of daily living, and these outcomes should be examined in different ethnic and socioeconomic groups.” The NICE Clinical Guidelines on the management of Multiple Sclerosis refer to FES only in the context of the management of urinary incontinence. Evidence of cost effectiveness There are currently no studies that examine the cost effectiveness of FES. References 1. The National Service Framework for Long-Term Conditions. 2. NICE IPG 278: Functional electrical stimulation for drop foot of central neurological origin 3. NICE Clinical Guidelines on the management of Multiple Sclerosis 4. Review articles: Minimizing fatigue for functional electrical stimulation of muscle. Clinical Rehabilitation, Vol. 3, No. 4, 333-340 (1989) 5. Functional electrical stimulation for limb motor dysfunction following stroke. Thomas Dent. STEER 2001; Vol 1: No.16 6. Clinical Policy Bulletin: Functional Electrical Stimulation and Neuromuscular Electrical Stimulation. AETNA 7. South Central Priorities Committees (Buckinghamshire/Milton Keynes PCTs) Policy Statement 75: Electrical Stimulation (including Functional Electrical Stimulation) for Upper and Lower Limb Dysfunction: May 2008 Acknowledgements: Adopted from NHS Derbyshire County The Human Rights Act has been considered in the development of this guidance