Physiology 27 [5-11
advertisement
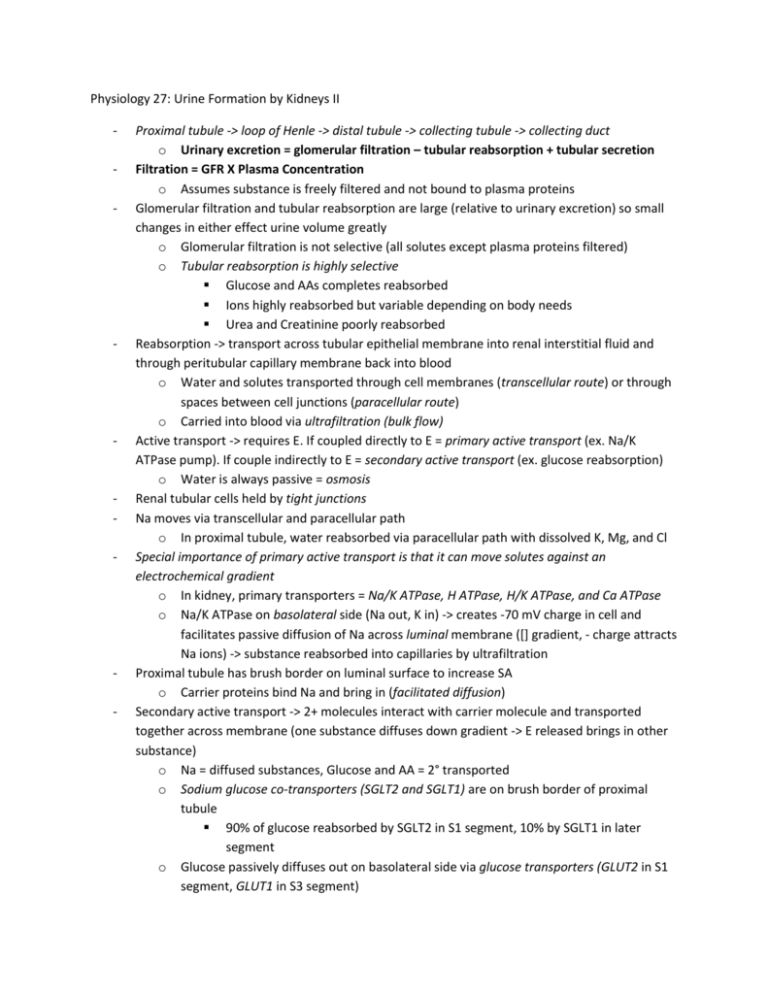
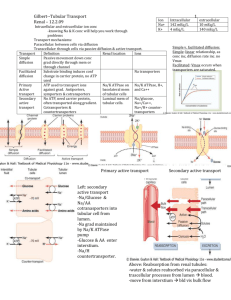
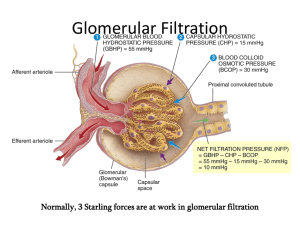
Physiology 27: Urine Formation by Kidneys II - - - - - Proximal tubule -> loop of Henle -> distal tubule -> collecting tubule -> collecting duct o Urinary excretion = glomerular filtration – tubular reabsorption + tubular secretion Filtration = GFR X Plasma Concentration o Assumes substance is freely filtered and not bound to plasma proteins Glomerular filtration and tubular reabsorption are large (relative to urinary excretion) so small changes in either effect urine volume greatly o Glomerular filtration is not selective (all solutes except plasma proteins filtered) o Tubular reabsorption is highly selective Glucose and AAs completes reabsorbed Ions highly reabsorbed but variable depending on body needs Urea and Creatinine poorly reabsorbed Reabsorption -> transport across tubular epithelial membrane into renal interstitial fluid and through peritubular capillary membrane back into blood o Water and solutes transported through cell membranes (transcellular route) or through spaces between cell junctions (paracellular route) o Carried into blood via ultrafiltration (bulk flow) Active transport -> requires E. If coupled directly to E = primary active transport (ex. Na/K ATPase pump). If couple indirectly to E = secondary active transport (ex. glucose reabsorption) o Water is always passive = osmosis Renal tubular cells held by tight junctions Na moves via transcellular and paracellular path o In proximal tubule, water reabsorbed via paracellular path with dissolved K, Mg, and Cl Special importance of primary active transport is that it can move solutes against an electrochemical gradient o In kidney, primary transporters = Na/K ATPase, H ATPase, H/K ATPase, and Ca ATPase o Na/K ATPase on basolateral side (Na out, K in) -> creates -70 mV charge in cell and facilitates passive diffusion of Na across luminal membrane ([] gradient, - charge attracts Na ions) -> substance reabsorbed into capillaries by ultrafiltration Proximal tubule has brush border on luminal surface to increase SA o Carrier proteins bind Na and bring in (facilitated diffusion) Secondary active transport -> 2+ molecules interact with carrier molecule and transported together across membrane (one substance diffuses down gradient -> E released brings in other substance) o Na = diffused substances, Glucose and AA = 2° transported o Sodium glucose co-transporters (SGLT2 and SGLT1) are on brush border of proximal tubule 90% of glucose reabsorbed by SGLT2 in S1 segment, 10% by SGLT1 in later segment o Glucose passively diffuses out on basolateral side via glucose transporters (GLUT2 in S1 segment, GLUT1 in S3 segment) - - - - - - - Active transport is when at least 1 step in reabsorption involves primary or secondary active transport Secondary active secretion involves counter-transport of susbstance o E from downhill movement of 1 substnace (Na) enables uphill movement of 2nd opposite o Ex. H secretion by Na/H counter-transporter (sodium-hydrogen exchanger) Pinocytosis -> protein attaches to brush border, invaginates, and vesicle formed with protein, digested to AAs and reabsorbed (active transport) Transport maximum = limit to rate at which solute transported (due to saturation of system when tubular load exceeds capacity) o Ex. Hyperglycemia exceeds load. Transport max for glucose = 375 mg/min, filtered load = 125 mg/min When plasma [glucose] >200 mg/dL (filtered load 250 mg/min) -> glucosuria = threshold for glucose (occurs before transport maximum is reached) Not all nephrons have same transport max so some excrete glucose Overall transport max for kidneys reached when all nephrons reached max capacity to reabsorb glucose Transport max for substance: o Glucose = 375 mg/min o Lactate = 75 mg/min o Phosphate = 0.10 mM/min o Plasma protein 30 mg/min o Sulfate = 0.06 mM/min o Creatinine = 16 mg/min o Amino acids = 1.5 mM/min o Para-aminohippuric acid = 80 o Urate = 15 mg/min mg/min Creatinine and para-aminohuppuric acid are actively secreted Some substance that are passively reabsorbed do not have transport maximum (rate or transport determined by electrochemical gradient, permeability of membrane, time fluid remains in tubule = gradient-time transport) o Some actively transported substances have characteristic of gradient-time transport Ex. Na reabsorption in proximal tubule -> backleak of Na through tight jxns (depends on permeability and interstitial physical force) Slower flow rate of tubular fluid, greater %age Na reabsorption In distal nephron, Na regulated by transport max (increased by aldosterone) Proximal tubule highly permeable to water through tight junctions between epithelial cells by osmosis, coupled to Na reabsorption o Carries with is solutes = solvent drag o In distal nephron, tight junctions less permeable but ADH increases H2O permeability (except in loop of Henle where no water reabsorbed) Na reabsorption allows Cl to diffuse passively though paracellular pathway. o Cl also goes down [] gradient created when H2O reabsorbed o Also reabsorbed by 2° active transport (co-transport with Na) Urea passively reabsorbed (down [] gradient from H2O reabsorption) o - - - In inner medullary collecting duct, facilitated by urea transporters Only ½ of urea filtered is reabsorbed (90% of waste nitrogen excreted) Creatinine is impermeant to tubular membrane (none reabsorbed) Proximal tubular (PT) reabsorption: o 65% Na and H2O, Cl reabsorbed o High capacity for active and passive reabsorption Large # of mitochondria to support, have brush border (↑ SA) with protein carrier molecules (co-transport and counter-transport mechanisms) o Na/K ATPase pump provides major reabsorptive force In first ½ of PT, Na reabsorbed by co-transport (glucose, AA, etc) and in second ½, Na reabsorbed with Cl ions (high [] here) o Amount of Na decreases but concentration of Na remains constant (H2O reabsorption); glucose, AA, and HCO3 concentrations ↓ ; creatinine [] increases along PT o Secretion of organic acids and bases (bile salts, oxalate, urate and catecholamines) plus filtration with lack of reabsorption -> rapid excretion Kidney also secretes harmful drugs (penicillin and salicylates) and toxins. Problem in maintaining therapeutically effective drug [] o Secretes para-aminohippuric acid (PAH) -> clear 90% from plasma used to estimate renal plasma flow Solute and water transport in Loop of Henle: o 3 segments: thin descending segment, thin ascending segment, and thick ascending segment Thin segments have no brush border, few mitochondria, and minimal activity o Descending segment -> highly permeable to water (20% reabsorbed) and moderately permeable to urea and Na (allow simple diffusion) o Ascending limb -> impermeable to water (concentrates urine) Thick segment has high metabolic activity (active reabsorption of Na, Cl, and K > 25% of filtered load)/ Ca, HCO3 and Mg also reabsorbed. Linked to Na/K ATPase on basolateral side In TAL, movement of Na across luminal side mediated by 1-sodium, 2chloride, 1-potassium co-transporter (uses potential E of Na; slight backlwak of K) and Na/H counter-transport Site of action of “loop” diuretics furosemide, ethacrynic acid, and bumetanide (inhibit 1-Na, 2-Cl, 1-K co-transporter) Paracellular reabsorption of Mg, Ca, Na, Aand K in TAL, too Distal Tubule: o First portion = macular densa (part of juxtaglomerular complex), next part highly convoluted (same reabsorption as TAL = diluting segement) o 5% of NaCl reabsorbed in early DT Na/Cl co-transporter coupled with Na/K ATPase and Cl channels Thiazide diuretics inhibit Na/Cl co-transporter - - - - - - Late Distal Tubule and Cortical Collecting Tubule: o Composed of principal cells and intercalated cells o Principal cells -> reabsorb Na and H2O, secrete K (depend on Na/K ATPase) K secretion involves K enter cell via Na/K ATPase (high []) and diffusion down [] gradient into tubular fluid Primary site of action of potassium-sparing diuretics (spironolactone, eplerenone, amiloride, and triamterene) Spironolactone/eplerenone -> mineralocorticoid receptor antagonists; compete with aldosterone (inhibit Na reabsorption and K secretion) Amiloride/triamterene -> Na channel blockers; directly inhibit Na entry (so ↓ Na/K ATPase activity and K secretion) o Intercalated cells -> reabsorb K and HCO3, secrete H (via H ATPase transporter) H generated via carbonic anhydrase, secreted (allowing HCO3 to be reabsorbed) o Impermeable to urea, reabsorb Na (controlled by hormones aka aldosterone), secrete K and H (key role in acid-base regulation), impermeable to H2O without ADH Medullary Collecting Duct: o Reabsorb <10% of H2O and Na (final site for processing urine) o Cells = cuboidal, few mitochondria o H2O permeability controlled by ADH (concentrates), permeable to urea (urea transporters), secretes H ions against large [] gradient If more H2O reabsorbed, substance is concentrated o Greater than 1.0 = concentrated; less than 1.0 = diluted Inulin = used to measure GFR because not reabsorbed or secreted (so changes in [] reflect H2O presence) o Ex. if inulin is 3.0 at end, means 3x as great as in plasma and only 1/3 of H2O filtered remains (2/3 reabsorbed) Intrinic ability of tubules to increase reabsorption in response to increased tubular inflow = glomerulotubular balance (independent of hormones, prevents overloading with GFR increases) o Total rate of reabsorption increases as filtered load increases o Second line defense (first-line = autoregulatory tubuloglomerular feeback) Peritubular capillary and renal interstitial fluid hydrostatic and colloid osmotic forces govern reabsorption o >99% of H2O and most solutes reabsorbed at normal rate of 124 ml.min o Reabsorption = Kf x Net reabsorptive force Net force from sum of hydrostatic and colloid forces o Normal peritubular cap pressure ~13mmHg, and renal interstitial fluid hydrostatic pressure ~6mmHg (opposes reabsorption) o Plasma colloid osmotic P ~32 mmHg and of interstitium ~15 mmHg (favors reabsorption) More than opposing so reabsorptive force ~10 mmHg o Kf normally 12.4 ml/min/mmHg Peritubular capillary hydrostatic pressure influenced by arterial pressure and resistnace of afferent and efferent arterioles - - - - - - - - o ↑ AP decreases reabsorption, ↑ arteriolar resistance increases reabsorption Colloid osmotic pressure of peritubular capillaries determined by systemic plasma colloid osmotic pressure and filtration fraction o High filtration fraction increases reabsorption (angiotensin II increases) Change in peritubular capillary Kf influences reabsorption (↑ raise reabsorption) Tight jxns between epithelial cells of proximal tubule = leaky so Na diffuse in both directions (net movement into capillaries) o Through hydrostatic and colloid osmotic pressure changes in renal interstitium, H2O and solute uptake match to net reabsorption of H2O and solutes Forces ↑ peritubular capillary reabsorption increase reabsorption from renal tubbules Small increase in AP -> pressure natriuresis and diuresis (between 75-160 mmHg of AP little effect because of GFR autoregulation) o If impaired autoregulation, increase in AP causes large increase in GFR o Increase AP also decreased percent of filtered load of Na and H2O reabsorbed o Reduced angiotensin II occurs with pressure natriuresis/diuresis Aldosterone (zona glomerulosa of adrenal cortex) -> increases Na reabsorption and K secretion o Site of aldosterone action is principal cells of cortical collecting tubule o Stimulates Na/K ATPase pump and Na permeability of luminal side o Stimuli for aldosterone: hyperkalemia, ↑ angiotensin II o Addison’s disease = loss of aldosterone -> loss of Na and accumulation of K o Conn’s syndrome = excess aldosterone -> Na retention and low K o More important regulator of [K] than for Na Angiotension II -> increases Na and H2O reabsorption o Increased with low BP (hemorrhage, excessive seating, severe diarrhea) o Stimulates aldosterone secretion, constricts efferent arteriole (increase reabsorption), directly stimulates Na reabsorption in proximal tubules, loop of Henle, distale tubules, and collecting tubules Stimulate Na/K ATPase pump, Na/H exchanger, and Na/HCO3 co-transport o Allows Na and H2O retention without retention of metabolic waste products ADH -> increases H2O reabsorption o Increase H2O permeability in distal and collecting tubule and collecting duct o Binds to V2 receptors -> cAMP -> protein kinase activation -> movement of aquaporin-2 (AQP-2) to luminal side of membrane forming water channels AQP-3 and AQP-4 on basolateral side allow water to exit (not regulated by ADH) Atrial Natriuretic Peptide -> decreases Na and H2O reabsorption (in collecting ducts), inhibits renin secretion as well o From cardiac atria when distended (in congestive heart failure) Parathyroid hormone -> increases Ca reabsorption (in distal tubules and loops of Henle), inhibits phosphate reabsorption in proximal tubule, Mg reabsorption in loop of Henle Sympathetic nervous system -> increase Na reabsorption in proximal tubule, TAL, and distal renal tubule, increase renin release - - - - - o Activates α-adrenergic receptors Renal clearance = volume of plasma completely cleared of substance by kidney per unit time o Quantifies rate of BF thru kidney, glomerular filtration, tubular reabsorption/secretion o Cs x Ps = Us x V, Clearance of substance, plasma [], urine [], and urine flow rate Inulin clearance used to estimate GFR (filtered but not reabsorbed or secreted) o GFR x Ps = Us x V, o Found in roots of plants, administered IV to pt to measure GFR Radioactive iothalamate and creatinine also used to estimate GFR Creatinine = by-product of muscle metabolism, entirely cleared by filtration o Not a perfect marker because small amount secreted by tbules o If can’t collect urine to measure CCr, approximation of changes in GFR obtained by measuring PCr GFR ~ CCr = UCrx V/PCr If GFR decreases, plasma [] of creatinine increases until reaches high enough level to cause normal excretion levels PAH clearance used to estimate renal plasma flow (completely cleared from plasma so = to renal plasma flow) o RPF = Us x V/Ps = Cs o %age of PAH removed from blood = extraction ratio of PAH (90% in normal kidney) Total RPF = PAH Clearance/PAH extraction ratio EPAH = (PPAH-VPAH)/PPAH, arterial and venous PAH Total BF through kidney = total RPF and Hct Filtration fraction depends on RPF (PAH clearance) and GFR (inulin clearance) o FF = GFR/RPF If clearance rate of substance = that of inulin -> only filtered, not reabsorbed or secreted If clearance rate of substance < inulin clearance -> reabsorbed (glucose, Na, Cl, K, and phosphate) If clearance rate of substance > inulin clearance -> secreted (creatinine)