pubdoc_10_1171_938

MAJOR SYMPTOMS OF DIGESTIVE TRACT DISORDERS
Vomiting
Definition Vomiting is a highly coordinated reflex process that may be preceded by increased salivation and begins with involuntary retching. Violent descent of the diaphragm and constriction of the abdominal muscles with relaxation of the gastric cardia actively force gastric contents back up the esophagus. This process is coordinated in the medullary vomiting center, which is influenced directly by afferent innervation and indirectly by the chemoreceptor trigger zone and higher central nervous system (CNS) centers
Mechanism
Vomiting is a very common symptom in many childhood illness, and is caused by various mechanisms:
Incompetence of GE sphincter leading to gastric contents refluxing up the esophagus.
•
Inflammation in the stomach (viral gastritis, stress ulceration).
•
Obstruction of the gut prevents the free passage of stomach contents down the GIT.
•
CNS problems can provoke vomiting by direct action on the vomiting center. A variety of drugs and toxins can induce vomiting in this way.
Causes
•
Causes are many and can be divided into groups:
A non-specific symptoms of acute illness: Number of infections lead to vomiting by causing the child to cough ( raising the intra-abdominal pressure) combined with a degree of gastric irritation ( e.g. viral upper airway infections and pertussis). In case of UTI general toxemia will act on vomiting center leading to vomiting.
•
Acute or chronic GIT illnesses: As GE, pyloric stenosis, appendicitis, intestinal obstruction, hepatitis, GER, peptic ulcer, food allergy, etc.
CNS conditions: Meningitis, raised ICP, migraine, and abdominal migraine (cyclic vomiting) which is • characterized by numerous episodes of vomiting ( about 9/mo) interspersed with well intervals, the onset is usually between 3-5 years of age and the episode last for 2-3 days with 4 or more emesis episodes per hour. Patients may have prodrome of nausea, lethargy, and headache or fever. Precipitants include stress and excitement. Treatment includes hydration and ondansetron (Zofran)and may be prevented by antimigraine agent.
Others: Metabolic disorders, poisoning, bulimia.
•
•
Management
History:
Vomiting itself: Color, content, amount, frequency, time of onset, and how long it has been a problem.
•
Associated symptoms: Diarrhea, abdominal pain, fever, symptoms of URTI (rhinitis, earache, etc.), symptoms of UTI, symptoms of DM, headache.
Past medical history: This is vital in identifying pre existing cause of vomiting e.g. previous abdominal surgery
(adhesion), IBD, DM, chronic use of steroid, IC shunt.
•
If vomiting is a chronic problem: •
• Vomiting occur after a feed or when winding, worse when lying flat, baby hungry after the vomit, and vomiting improve at time of weaning, suggest GER
•
Recurrent episodes of vomiting, with no symptoms in between, suggest cyclic vomiting.
Recurrent abdominal pain, suggest IBD or peptic ulcer.
•
Intermittent headache with vomiting, photophobia and visual disturbance, suggest migraine.
•
•
Clinical examination:
General examination: Fever (infection), hydration state (resuscitation), LAP (mesenteric adenitis), jaundice (hepatitis), anaemia and weight loss ( IBD).
Abdomen: RIF tenderness, enlarged tender liver ( hepatitis), signs of intestinal obstruction, strangulated hernia, visible peristalsis and pyloric mass ( pyloric stenosis) sausage-shape mass ( intussusceptions).
Other systems: Examination of RS and ENT should be performed, while CNS exam done if indicated.
Investigations:
Urine exam.: For UTI and DM.
•
Full blood count: Increased neutrophil count in bacterial infection.
•
Urea and electrolyte: Essential in managing fluid replacement.
Blood glucose.
•
•
LFT.
•
Abdominal X ray: For intestinal obstruction.
•
Abdominal US: For pyloric stenosis and intussusception.
•
Barium studies: For GER, intestinal obstruction, and IBD.
PH study : GER.
•
Lumber puncture : For meningitis.
•
CT/MRI of brain: For IC cause other than meningitis.
•
•
Constipation:
Definition
Any definition of constipation is relative and depends on stool consistency, frequency, and difficulty in passing the stool.
However, the consistency of the stool, not the frequency is the basis for the diagnosis. So, a normal child may have a soft stool only every 2 or 3 days without difficulty; this is not constipation. However, hard stool passed with difficulty every 3 days should be treated as constipation.
Mechanism
The mechanism of defecation begins with peristaltic waves in the colon which advances the faeces into the rectum. Constipation may arise from defects either in filling or emptying the rectum.
Defective rectal filling occurs when colonic peristalsis is ineffective e.g., hypothyroidism, opiate use and intestinal obstruction
(structural or Hirschspring disease).
Emptying the rectum depends on defecation reflex initiated by pressure receptors in the rectal muscles, afferent fibers to the sacral spinal cords, efferent fibers to the anal sphincter and abdominal and pelvic floor muscles. Lesions involving any parts of this reflex can cause constipation.
Constipation tend to be self-perpetuating, whatever its cause. Hard ,large stool in the rectum become difficult and even painful to evacuate; thus more retention occurs and vicious circle ensues. Distention of the rectum and colon lessens the sensitivity of the defecation reflex and the effectiveness of peristalsis. eventually watery content from the proximal colon may percolate around hard retained stool and pass per rectum unperceived by the child. this is involuntary encopresis may be mistaken for diarrhea.
Causes
Organic causes: Mechanical intestinal obstruction ( anal atresia, intestinal atresia, Meconium ileus, intussusceptions, malrotation, adhesion, Crohns disease, etc..), absence of normal peristalsis (Hirschspring disease, paralytic ileus, hypothyroidism, hypercalcaemia, drugs as codeine, vincristine and antidepressant), spinal cord lesion and myotonic dystrophy.
• Non-organic cause (functional constipation): responsible for 90-95% of cases of chronic constipation in young children. Bowel itself is normal, but there is irregular and incomplete defecation, due to voluntary withholding of faeces.causes include the following:
Painful defecation.
•
•
Poor potty training: voluntary control of defecation is usually achieved around the 2 nd birthday, and potty training is a common time for functional constipation. Excessive coercive potty training or attempted training at too early age results in the child becoming unwilling, and afraid of, opening their bowels.
•
Poor diet: inadequate fluid intake, inadequate fiber intake and diet high in fat or protein (excessive milk ingestion) can result in the formation of hard stool that are painful to pass.
•
Management
History
Consistency, frequency and difficulty in passing stool.
Age of onset.
•
Is it acute or chronic problem.
•
•
Any history of delay in passing Meconium in neonatal period (put in mind H. disease, CF or hypothyroidism).
Dietary history.
•
How potty training was managed.
•
•
Are there urinary symptom; severe constipation may cause urinary retention or predispose to UTI.
Any motor or sensory symptoms in the legs (spinal cord lesion).
•
•
Clinical examination
•
General examination: Growth and nutritional assessment ( IBD.
CF), general wellbeing ( septicemia may cause paralytic ileus), dysmorphic features (increase the risk of congenital anomalies of the gut).
Abdomen: Signs of intestinal obstruction, sausage shaped mass or any other mass, position and patency of anus, lowe r spine exam .
Other : If there is spinal anomaly or the history suggests spinal lesion, neurological examination of the lower limbs is indicated.
Investigations
Full blood count : Preoperative assessment.
•
Urea and electrolytes : Electrolytes abnormalities are likely in the presence of obstruction. Also helpful in assessing state of hydration.
Abdominal X ray: Diagnose intestinal obstruction ( distended loops of bowel with air fluid levels).
•
Abdominal ultrasound: Diagnose intussusception.
Contrast studies : D iagnose atresia and malrotation.
•
•
•
Air enema: Diagnostic and therapeutic value in intussusception.
•
Rectal biopsy: The gold standard for diagnosis of Hirschspring disease.
•
Abdominal pain
Mechanism
Tow types of nerve fibers transit painful stimuli in the abdomen. In skin and muscle, A fibers mediate sharp localized pain; and
C fibers from viscera, peritoneum and muscle transmit poorly localized, dull pain. Pain is perceived in the cortex of central gyrus. Visceral pain tends to be experienced in dermatome from which the affected organ receives innervation. Painful stimuli originated from liver, pancreas, biliary tree, stomach, or upper bowel are felt in the epigastrium; pain from distal small bowel, caecum, appendix, or proximal colon is felt at the umbilicus; and pain from distal large bowel, UT, or pelvic organs is usually suprapubic. When pain is referred to remote areas it is usually means an increased intensity of provoking stimuli.
In the gut, the stimuli provoking pain a re:
Tension and stretching.
•
Inflammatory lesions: The mechanisms producing pain are not clear, but inflammation may lower the pain threshold.
Ischemia: The metabolites released near nerve endings probably account for the pain.
•
•
Perception of these painful stimuli can be modulated by input from both cerebral and peripheral sources ( psychologic factors are particularly important).
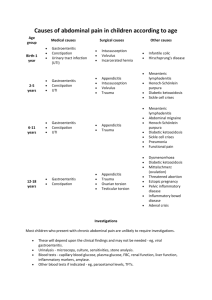
Causes
Acute abdominal pain: Pancreatitis, hepatitis, gastroenteritis, renal stone, gallstone, surgical causes, UTI, pneumonia, e tc..
Recurrent abdominal pain : Defined as a pain that occurs at least monthly for 3 successive months with severity that interrupts routine functioning. It affect 15% of children and classified into:
Organic RAP ( 5-10%): Chronic constipation, lactose intolerance, giardiasis, excessive fructose or sorbitol ingestion, IBD, peptic ulcer, chronic appendicitis, UTI, renal stone, gall stone, abdominal migraine, sickle cell disease, lead poisoning, Henoch-Schonlein purpura, angioneurotic edema, familial Mediterranean fever, etc..
•
•
Non-organic RAP ( 90%): The pain can not explained on structural or biochemical basis. Characteristic presentation includes:
Onset > 6 years.
•
• Midline paroxysm ( periumbilical, epigastric, suprapubic).
Interrupt normal activity.
•
No symptoms of organic disease.
•
Usually no relationship with meals.
•
•
Symptoms positively related to anxiety and depression especially in IBS.
Improvement of symptoms during weekend is suggestive,
•
Non-organic RAP is a spectrum of clinical disease involving the followings:
RAP syndrome ( functional abdominal pain): Non-specific pain, often periumbilical.
•
Irritable bowel syndrome : Account for 1/3 of the cases of RAP. Suprapubic cramps, bloating, abdominal distention and altered bowel pattern.
Non-ulcer dyspepsia: Epigastric pain frequently associated with symptoms of early satiety, nausea, bloating, in the presence of negative evaluation and no response to acid-
• blocking medication.
•