Universal Precautions Policy and Procedure Template
advertisement
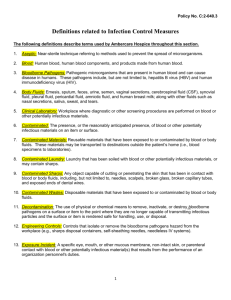
DEPARTMENT OF FAMILY AND SUPPORT SERVICES CITY OF CHICAGO Infectious Disease Control Any employee with the potential for occupational exposure to blood or other potential infectious materials is at risk for transmission of blood borne pathogens which may lead to disease. In accordance with the OSHA Blood borne Pathogen standard 29, CFR 1910.1030, the following Infectious Disease Control Plan has been developed. A copy of the Infectious Disease Control Plan is accessible to all employees. It is distributed to all current employees as a part of the Risk Management Plan. Occupational Exposure Occupational exposure is defined as the reasonable anticipation of skin, eye, mucous membrane, or other contact with blood or other potentially infectious bodily fluids that may result from the performance of an employee’s duties. Exposure Determination In the following job classifications, employees may come into contact with blood or other potentially infectious bodily fluids: 1. Early Childhood Teaching Staff: The duties of these employees require them to render physical care and to clean up after incontinent acts and vomiting, and/or injuries producing blood. 2. Facilities Staff: The duties of these employees require them to clean up and dispose of waste, and fix and maintain areas which may be contaminated with blood or other potentially infectious materials. 3. All other staff in the provision of first aid. In the following procedures performed during the course of the child care program day, occupational exposure may occur during: The daily health check. Care of wounds. Clean up of body fluids such as emesis, feces, urine, or blood. Disposal of waste. First aid. (This list does not exhaust all tasks which may result in the potential for exposure.) Contaminated means the presence or the reasonably anticipated presence of blood or other potentially infectious materials on an item or surface. The blood or other potentially infectious materials may be liquid, semi-liquid, or dried. Occupational Exposure Plan In the event of an exposure to blood or other potentially infectious body fluids, immediately clean a skin injury thoroughly with soap and running water for 10-15 seconds using friction. In the event of a mouth splash, immediately rinse the mouth with running water. Immediately flush eyes with running water, sterile water, or saline solution in the event of an eye splash. Notify the program director or supervisor to assist you in obtaining first aid if necessary. Per Exposure Control Plan, employee should go to nearest E.R. A written incident report must be completed within one working day of the incident and submitted to the program director and executive director. A complete history of the circumstances surrounding the accidental exposure must be submitted, including where, when, and how the incident occurred, the nature of the injury, the source of the exposure, personal protective equipment in use at the time of the incident, actions taken by the employee. The employer may be referred to their primary physician for follow-up care or evaluation. Any necessary follow up care or lab work will be conducted by an accredited laboratory will be done at no cost to an employee. Follow-up procedures will include a confidential medical evaluation documenting the circumstances of exposure, identifying and testing the source if feasible, testing the exposed employee’s blood if he/she consents, and counseling on the reported illness. Health care professionals must be provided specified information from the agency to facilitate the evaluation and the health care professional’s written opinion on the need for hepatitis B vaccination following the exposure. Information such as the employee’s ability to receive the hepatitis B vaccine must be supplied to the employer. However, all diagnoses must remain confidential. In accordance with OSHA standards, records for all employees who have been exposed must be kept for the duration of employment plus an additional thirty years. Records must be kept confidential and include: name, social security number, hepatitis B vaccination status (including dates), results of any examinations, medical testing and follow-up procedures, and a copy of information provided to the health care professional. Universal Precautions The practice of using “Universal Precautions” is followed to prevent or limit contact with blood and other potentially infections materials since any exposure could result in transmission of blood borne pathogens, which could lead to disease or death. It is not always known if human blood and bodily fluids are contaminated, therefore, all blood and bodily fluids are to be treated as if it is known to be infectious for HBV, HIV, or other blood borne pathogens. Universal precautions require the use of personal protective equipment and hand washing to prevent or minimize employee exposure of skin and mucus membranes to blood and other potentially infectious materials. Human body fluids include the following substances: amniotic fluid, bodily tissues, broken skin, cerebrospinal fluid, nasal secretions, pleural fluid, pericardial fluid, peritoneal fluid, saliva, sputum, semen, synovial fluid, urine, vaginal secretions, vomit, wound drainage, feces, and any bodily fluid that is visibly contaminated with blood. In circumstances where it is difficult or impossible to differentiate between bodily fluid types, it should be assumed that all bodily fluids are potentially infectious. Universal precautions should be used by all HACC personnel when examining, treating, and caring for all participants, staff, or community member regardless of age, race, gender, HIV status, lifestyle, or ethnic background. Universal precautions involves a two part system of using proper hand washing techniques and using protective equipment to minimize exposure to bodily fluids. Hand washing Proper hand washing technique is as follows: 1. Vigorously lather hands with soap and rub them together, using friction to all surfaces for fifteen seconds. Hold hands lower than wrists. Do not touch fingertips to inside of sink. 2. Rinse hands thoroughly under a moderate stream of water at a comfortable temperature. Hot water is unnecessarily rough on hands. 3. Dry hands well with paper towels, and then turn off faucets with those towels. 4. Discard paper towels in trash. 5. In areas where sinks are not readily accessible, a waterless antiseptic solution may be used between tasks that would normally require hand washing. Hands should be washed with soap and water at the first opportunity. 6. The use of gloves does not replace hand washing. Hands must be washed immediately after removing gloves. Signs visually illustrating proper hand washing technique are located in all early childhood bathrooms. Staff members are required to wash their hands at the following times: 1) Upon arrival at the center; 2) After using the bathroom or helping a child use the bathroom; 3) After changing a diaper; 4) After wiping or blowing their nose, or helping a child to wipe or blow his/her nose; 5) After handling items soiled with body fluids or wastes (e.g., blood, drool, urine, stool or omit); 6) After handling pets or other animals; 7) After handling or caring for a sick child; 8) Before and after eating or drinking; 9) Before preparing, handling or serving food; 10) Before dispensing any medication; 11) Before and after administering first aid; and 12) When changing rooms or caring for a different group of children. Antiseptic hand cleaner with paper towels or sanitary cloth towels, or antiseptic towelettes may be used in emergency cases only when soap and running water are not available. Soap and running water should be used immediately when it becomes available. Personal Protective Equipment Personal protective equipment (PPE) is specialized clothing or equipment, including gloves, masks, mouthpieces, and resuscitation bags, that is worn or used by an employee for protection against occupational exposure to blood or other potentially infectious materials. PPE will be provided to employees at no cost and must be used, as appropriate, to protect themselves against exposure to blood borne pathogens. Not all tasks involve the same type or degree of risk, and therefore, do not require the same kind or extent of protection. PPE is considered appropriate only if it does not permit blood or other potentially infectious materials to pass through or to reach the employee’s clothes, skin, eyes, mouth, or mucus membranes. PPE usage guidelines are summarized at the end of this section. PPE includes, but is not limited to gloves, gowns, laboratory coats, masks, protective eye wear (face shields, safety glasses), or ventilation devices (resuscitation bags or seal-easy masks). First-aid kits, as well as blood borne pathogen clean-up kits, which include absorbent powder, protective exam gloves, protective eye wear, shoe covers, apron, isolation masks, MSDS sheets, disposable towels, antiseptic wipes, disposable red biohazard bags with ties, disinfectant wipe, and instruction sheets are located in all major areas or the agency, including the early childhood office and all four early childhood classrooms. PPE should be removed before leaving a work area. It is the employer’s responsibility to provide, launder, repair, replace, or dispose of PPE. Latex gloves should be worn at all times when dealing with any bodily fluids, potentially infectious material, or when handling/touching contaminated surfaces (including, but not limited to changing diapers or clothing with urine or feces, applying first-aid, cleaning bathrooms, or cleaning animal cages and working in the dental clinic). Hypoallergenic gloves will be provided to all employees who are allergic to standard gloves, and should request them with his/her program director. Gloves are to be removed without exposing the skin to the outer surface of the glove. Soiled gloves must be placed in a sealable bag and disposed of so that further exposure will not occur. All staff members must wash their hands upon removing the latex gloves. Warning labels, including the orange or orange-red biohazard symbol are affixed to containers of regulated waste, refrigerators and freezers and other containers which are used to store or transport blood or other potentially infectious materials. Red bags or containers may be used instead. Laundry must always be handled with universal precautions, and therefore, does not need to be labeled. Work Practice Controls The following work practice controls are adhered to by __________________ (insert program name) in compliance with the OSHA Blood borne Pathogens Standard: 1. Proper hand washing immediately, or as soon as feasible, after removal of latex gloves or any other personal protective equipment. 2. Following any contact of body area with blood or any other potentially infectious material, employees must wash their hands and any exposed skin with soap and water as soon as possible. They also must flush exposed mucus membranes with water. 3. Contaminated sharps are placed in appropriate containers as soon as possible after use. Sharps containers are to be replaced routinely and not allowed to overfill. Containers for contaminated sharps must be puncture resistant, leak-proof on the sides and bottom, and color-coded or labeled with a biohazard warning label. 4. Contaminated needles are not to be removed from syringes by hand. Contaminated needles and sharps are not to be bent, broken, re-capped, or removed unless it can be demonstrated that there is no feasible alternative. 5. Eating, drinking, smoking, and applying cosmetic or lip balm and handling contact lenses is prohibited in work areas where there is potential for exposure to blood borne pathogens. 6. Food and drink are not to be kept in refrigerators, freezers, on countertops, or in other storage areas where blood or other potentially infectious materials are present.