Integument - Austin Community College
advertisement

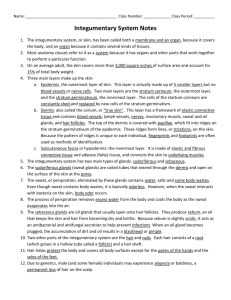
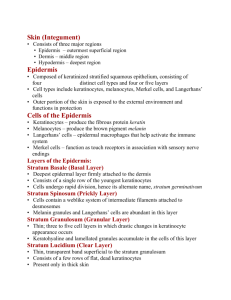
Integumentary System Cutaneous layer – the skin (most superficial) Cutaneous = “of the skin” Skin accounts for 7% of body weight Divided into two distinct layers: Epidermis Dermis Subcutaneous layer (hypodermis) – Subcutaneous = “below the skin” Consists of areolar (connective tissue) and adipose (fat) tissues Functions Of The Integument Cushions and insulates deeper organs Protects body from abrasion, trauma, chemicals, pathogens, temperature extremes, and UV rays Waterproofing; Prevention of water loss Holds sensory receptors associated with nerve endings Synthesis and storage of nutrients (vitamin D3) Excretion and secretion (urea, water, salts via sweat) Integumentary Structures The Epidermis - Four Main Cell Types Melanocytes - produced basal layer Manufacture and secrete melanin pigment Melanin is passed from melanocytes to keratinocytes Merkel cells – located in basal layer Attached to sensory nerve endings Serve as tactile (touch) receptors Keratinocytes – arise from deepest layer of epidermis to stratum spinosum Constitute 95% of the cells in the epidermis Produce keratin – a tough fibrous protein Produce antibodies and enzymes that detoxify harmful chemicals Corneocytes - keratinocytes that have lost their nucleus & organelles (considered dead cells) Langerhans cells – located in stratum spinosum A dendritic cell; part of immune system Phagocytic The Epidermis The Epidermis Stratified squamous epithelium Several distinct cell layers Thick skin – five layers on palms and soles Thin skin – four layers on rest of body Layers of The Epidermis Stratum corneum (cornified layer) Most superficial layer Corneocytes – dead, flattened squamous cells; Cornified – filled with keratin, a tough, waterresistant protein Protects skin against abrasion and penetration Sheds in flakes (desquamation) Stratum lucidum (clear layer) Occurs only in thick skin (palms and soles) Composed of a few rows of flat, dead keratinocytes At times visibly indistinguishable from adjacent layers Stratum granulosum (grainy layer) Contain tonofilaments (intermediate filament) Bundled at desmosomes Resist tension Contain protein prekeratin Keratohyaline granules – help form keratin in dying keratinocytes Lamellated granules – release a waterproofing glycolipid Stratum spinosum (spiny layer) “Spiny” appearance a result of histological preparation Cells shrink but maintain desmosome connections Contain tonofilaments Contains star-shaped Langerhans cells (dendritic immune cells) Stratum basale (basal layer) Single row of cells Deepest layer of epidermis Attached to underlying dermis High mitotic rate - stem cells actively divide, forming new keratinocytes Merkel cells – associated with sensory nerve ending Melanocytes (10 – 25%) – secrete the pigment melanin Sources of Skin Color Melanocytes Produce melanin from the amino acid tyrosine using the enzyme tyrosinase Melanin moves from melanocytes to keratinocytes Melanin provides UV protection Gives reddish-brown to brown-black color Carotene Yellow-orange pigment Obtained from vegetable sources (carrots and tomatoes) Hemoglobin - blood pigment The blood pigment Caucasian skin contains little melanin- nearly transparent- which allows crimson color of blood to show through Dermis Second major layer of the skin Provides mechanical strength, flexibility, and protection for underlying tissues Highly vascular and contains a variety of sensory receptors that provide information about the external environment Two layers: Papillary layer – includes dermal papillae Reticular layer – deeper layer – 80% of thickness of dermis Flexure lines – creases on palms Layers of the Dermis Papillary layer Underlies epidermis Named for dermal papillae Aerolar connective tissue Supports, nourishes epidermis Provides sensory nerves, lymphatics, and capillaries Reticular layer Tough, dense, fibrous layer Dense irregular connective tissue Collagen fibers - limit stretch Elastic fibers - provide flexibility Blends into papillary layer above Blends into subcutaneous layer below Dermal Components Epidermal accessory organs Cells of connective tissues proper Communication with other organ systems Cardiovascular Lymphatic Nervous Sensation Control of blood flow and secretion Subcutaneous Layer – Hypodermis Composed of loose connective tissue types: areolar and adipose Stabilizes skin position Loosely attached to dermis Loosely attached to muscle Contains many fat cells Provides thermal insulation Cushions underlying organs Safely receives hypodermic needles Appendages of the Skin Hair Nails Glands Sebaceous Glands Sweat Glands Hair Flexible strands of dead keratinized cells Produced by hair follicles Contains hard keratin which is tougher and more durable than the soft keratin of the skin Chief parts of a hair: Root – imbedded in the skin Shaft – projects above skin's surface Cross Section of a Hair Hair Shaft organized into three concentric layers Medulla – central core Cortex – surrounds medulla Cuticle – outermost layer Pigmented by melanocytes at the base of the hair Hair Follicle Root sheath extending from the epidermal surface into the dermis Deep end is expanded forming a hair bulb Papilla - nipple-shaped indentation with blood vessels and nerves Matrix - germinal layer of cells (actively dividing cells) right above the papilla Sensory nerve endings – afferent nerve receptors (a root hair plexus) wrapping around each hair bulb Bending a hair stimulates these endings, hence our hairs act as sensitive touch receptors Arrector pili muscle - bundle of smooth muscle contracts to make hair stand erect Longitudinal Section of Follicle Shape of Hair Shaft Hair Color Melanocytes in the matrix of the hair bulb Melanin is transferred to the cells in the hair shaft. Different proportions of brown-black, yellow and reddish melanin combine to produce varieties of hair color, from blond to black. Gray hair occurs because of a decline in the enzyme (tyrosinase), inhibiting the conversion of tyrosine to melanin White hair is an accumulation of air bubbles in hair shaft combined with lack of pigment (decrease in tyrosinase) In red hairs, nearly all the melanin is present in the form of phaeomelanin (a lighter pigment found in red and blonde hair) Hair Function and Distribution Functions of hair include: Helping to maintain warmth Alerting the body to presence of insects on the skin Guarding the scalp against physical trauma, heat loss, and sunlight Hair is distributed over the entire skin surface except: Palms & soles Lips Nipples and portions of the external genitalia Glands Holocrine glands Whole glandular cells break apart to form the product Used by sebaceous glands to produce sebum (oil) at hair follciles Eccrine (Merocrine) glands Vesicles release product via exocytosis Most numerous type of integumentary gland Produce “true sweat” Apocrine glands Apical portion of glandular cells pinch off as product Mostly confined to axillary (armpit), anal, and genital areas Made of true sweat plus fats and proteins Sebaceous (Oil) Glands Sebaceous glands (oil glands) secrete oil onto hair shafts Occur over entire body, except palms and soles Holocrine secretion Entire cell breaks up to form secretion Simple alveolar glands Secretes an oily substance called sebum Most are associated with a hair follicle Sebum (oil) Composed of lipids, wax, and the debris of dead, fat-producing cells. Softens and lubricates hair and skin; Prevents drying & cracking Waterproofs skin Collects dirt Sudoriferous (Sweat) Glands Two types of Sudoriferous Glands: Eccrine (Merocrine) Vesicles release product via exocytosis Ducts form individual pores directly on skin surface Produce “True sweat” o 99% water with some salts o Traces of metabolic wastes ~ 2% urea Role in thermoregulation Most abundant sweat gland (~500/cm2) Apocrine Apical portion of glandular cells pinch off as product Ducts merge with hair follicle, superior to sebaceous (oil) glands Milky, viscous, sweat made of true sweat, plus fats and proteins Odorous secretion until digested by bacteria Secretion begins at puberty Present in axillary, areolar, anal, and genital areas Product contains pheromones, responsible for synchrony of menstrual cycle in females Sudoriferous (Sweat) Glands Modified Sudoriferous (Sweat) Glands Ceruminous glands Localized in outer auditory canal Produce cerumen (ear wax) waterproofs the canal kills bacteria traps foreign particles (dust, fungal spores) by coating guard hairs, making them sticky Mammary glands Localized in anterior thorax Produce colostrum and milk in pregnant and nursing females Nails Scale-like modification of epidermis made of hard keratin Parts of the nail: Free edge Body (dense mass of keratinized cells) Root Nail folds Eponychium (cuticle) Nail matrix Skin Injury and Repair Four Stages in Skin Healing: Inflammation Blood flow increases Phagocytes attracted Scab formation Cell division and migration Scar formation Skin Injury and Repair 1) Bleeding occurs at the site2 of injury immediately after the injury, and mast cells in the region trigger an inflammatory response. 2) After several hours, a scab has formed and cells of the stratum germinativum are migrating along the edges of the wound. Phagocytic cells are removing debris, and more of these cells are arriving with the enhanced circulation in the area. Clotting around the edges of the affected area partially isolates the region. 3) One week after the injury, the scab has been undermined by epidermal cells migrating over the meshwork produced by fibroblast activity. Phagocytic activity around the site has almost ended, and the fibrin clot is disintegrating. 4) After several weeks, the scab has been shed, and the epidermis is complete. A shallow depression marks the injury site, but fibroblasts in the dermis continue to create scar tissue that will gradually elevate the overlying epidermis. Aging of the Skin Major Age-Related Changes Telomeres (DNA caps) shorten with every mitotic divide Cells enter “retirement” stage of the Cell Life Cycle (Stage G0) Cells eventually stop dividing Fibroblasts in connective tissue decrease in collagen or elastin production; Skin sags, wrinkles, and becomes thin Skin becomes dry, scaly Injury and infection increase; Repair slows Immune cells decrease Sun protection by melanocytes diminishes Hair thins, grays Thermoregulation decreases Effects of UV Radiation Beneficial effect Activates synthesis of vitamin D3 Harmful effects: Sun burn Wrinkles, premature aging Malignant melanoma Basal cell carcinoma Types and Growth of Hair Vellus hairs Body hairs of women and children Terminal hairs Hair of scalp Axillary and pubic area (at puberty) Hair thinning and baldness Due to aging Male pattern baldness X-linked recessive Men (XY) need only one affected X chromosome to cause hair loss Women (XX) need two affected X chromosomes for hair loss Burns Classified by severity: First-degree burn – only upper epidermis is damaged Redness Second-degree burn – upper part of dermis is also damaged Blisters appear Skin heals with little scarring Third-degree burn Consumes thickness of skin Burned area appears white, red, or blackened Estimating Burns Using the Rule of Nines Head = 9% Chest (front) = 9% Abdomen (front) = 9% Back = 9% Buttocks = 9% Left Arm = 9% (front = 4.5%, back = 4.5%) Right Arm = 9% (front = 4.5%, back = 4.5%) Front of Left Leg = 9% Back of Left Leg = 9% Front of Right Leg = 9% Back of Right Leg = 9% Groin = 1% Total: 100% Skin Cancer Basal cell carcinoma Least malignant and most common Squamous keratinocytes in basal layer Squamous cell carcinoma Arises from keratinocytes of stratum spinosum Melanoma The most dangerous type of skin cancer A cancer of melanocytes Most serious type, affects melanocytes Development of Integument Epidermis Develops from embryonic ectoderm Dermis and hypodermis Develop from mesoderm Melanocytes Develop from neural crest cells Fetal skin Well formed after the fourth month At 5-6 months The fetus is covered with lanugo (downy hairs) Fetal sebaceous glands produce vernix caseosa the waxy or cheese-like white substance found coating the skin of newborn babies