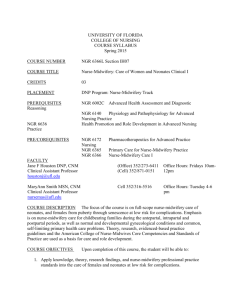
COURSE NUMBER NGR 6361C sections 7683

UNIVERSITY OF FLORIDA
COLLEGE OF NURSING
COURSE SYLLABUS
SUMMER 2012
COURSE NUMBER
COURSE TITLE
NGR 6361C sections 7683, 8462
Nurse-Midwifery Care II
CREDITS
PLACEMENT
6 (2 credits didactic, 4 credits laboratory)
Second course in Nurse-Midwifery Clinical Track
PREREQUISITE
FACULTY
NGR 6360C: Nurse-Midwifery Care I
Jane F Houston DNP, CNM e-mail: houstonj@ufl.edu
Clinical Assistant Professor
Office Hours: Friday 10-12 or by appointment
MaryAnn Smith MSN, CNM
352/273-6411 (Office)
352 871-0151 (Cell)
Cell 352/316-5516 Office Hours: Tuesday 4-6 pm Clinical Assistant Professor nursemas@ufl.edu
DEPARTMENT CHAIR Susan Schaffer, PhD, ARNP, FNP-BC (Gainesville)
Phone: 352/273-6366 e-mail: sdschaf@ufl.edu
CAMPUS DIRECTOR:
Office Hours: by appointment
Andrea Gregg, RN, DSN (Jacksonville)
Phone: 904-244-5172 e-mail: greggac@ufl.edu
Office Hours: by appointment
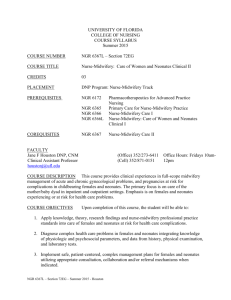
COURSE DESCRIPTION This is the second of two courses presenting specialized knowledge of current theories and techniques in nurse-midwifery care. The emphasis is on the development of nurse-midwifery management skills in the care of at-risk women seeking primary care, gynecological, antepartal, intrapartal, or postpartal care and at-risk neonates. Care of at risk women from diverse backgrounds across the lifespan is a focus of this course.
COURSE OBJECTIVES Upon completion of this course, the student will be able to:
1. Integrate scientific theories and research findings from nursing and other disciplines into nurse-midwifery practice to provide primary care, gynecological, antepartal, intrapartal, and postpartal care to at-risk clients.
2. Synthesize and apply knowledge of abnormal physiologic and psychosocial aspects to at-risk women and neonates receiving nurse-midwifery care.
COURSE SYLLABUS NGR 6361C
Page 1
3.
Demonstrate the role and professional responsibilities of the nurse-midwife in the provision of culturally sensitive care and management of at-risk women and neonates.
4.
Collaborate with other health care providers to ensure continuity of care and optimal health care delivery for at-risk nurse-midwifery clients.
5. Analyze major factors contributing to infant and maternal morbidity and mortality in
Florida and in the nation.
6.
Utilize legal and ethical principles to formulate decisions in an advanced nurse- midwifery practice role.
TEACHING METHODS
Online lecture via Voice Thread, case studies, discussion boards with live discussion via
Adobe Connect (Tuesdays 7-8pm, mandatory attendance), demonstration, electronic sources, audiovisual materials, supervised clinical practice.
Note: Student attendance is required for a two-day intensive session at beginning of the semester
(see schedule).
E-Learning (Sakai) is the course management system that you will use for this course.
E-Learning is accessed by using your Gatorlink account name and password at http://lss.at.ufl.edu
. There are several tutorials and student help links on the E-Learning login site. If you have technical questions call the UF Computer Help Desk at 352-392-HELP or send email to helpdesk@ufl.edu
.
It is important that you regularly check your Gatorlink account email for College and University wide information and the course E-Learning site for announcements and notifications.
Course websites are generally made available on the Friday before the first day of classes.
CLINICAL SCHEDULE
TBA
ATTENDANCE
Students are expected to be present for all classes, other learning experiences and examinations. Students who have extraordinary circumstances preventing attendance should explain these circumstances to the course instructor prior to the scheduled class or clinical lab, or as soon as possible thereafter. Instructors will make an effort to accommodate reasonable requests. A grade penalty may be assigned for late assignments or make-up exams. Make-up exams may not be available in all courses.
Students are expected to be present for all scheduled clinical practice experiences and seminars. Students who have extraordinary circumstances preventing attendance should explain these circumstances to the course instructor prior to the scheduled clinical practice experience or seminar. Instructors will make an effort to accommodate reasonable requests. A grade penalty may be assigned for unexcused seminar or clinical absences. The faculty member will advise the method of notification for absences to the clinical site e.g. phone, email, and notification of facility.
Graduate students are required to submit a written calendar of planned clinical practice dates and times to the course faculty member prior to beginning the clinical rotation. Any changes to the calendar (dates and times) must be submitted in writing to the course faculty member before the change is planned to occur. Clinical hours accrued without prior knowledge of the faculty member will not be counted toward the total number of clinical hours required for the course.
ACCOMMODATIONS DUE TO DISABILITY
Each semester, students are responsible for requesting a memorandum from the Disability
Resource Center to notify faculty of their requested individual accommodations. This should be done at the start of the semester.
STUDENT HANDBOOK
Students are to refer to the College of Nursing Student Handbook for information about
College of Nursing student policies, honor code, and professional behavior. Of particular importance for this course are the sections on appearance in clinical practice areas, personal liability insurance, and student safety.
TOPICAL OUTLINE
1.
Nurse-midwifery management of at-risk women and neonates
2.
Anatomy and physiology of fetal/neonatal complications and complications related to pregnancy
3.
Genetics and embryology
4.
Environmental and occupational hazards that affect pregnancy
5.
Indicators of at-risk and/or high risk-pregnancy and deviations from normal in neonates with appropriate interventions
6.
Diagnosis and management of antepartal complications: Rh incompatibility, anemias, hemoglobinopathies; hypertensive disorders and trophoblastic disease; preterm labor, premature rupture of membranes, dysmaturity, grandmultiparity, and multiple gestation; bleeding disorders; infectious diseases; gastrointestinal/genitourinary problems; endocrine disorders; and concurrent/preexisting medical problems
7.
Diagnosis and management of intrapartal complications: breech and malpresentations; prolapsed cord, depressed neonate, bleeding disorders, postpartum hemorrhage, shoulder dystocia, multiple gestation, dysfunctional labor and fetopelvic disproportion
8.
Diagnosis and management of postpartal complications: infections, hemorrhage, perinatal loss, and psychosis
9.
Diagnosis and management of neonatal complications, including risk factors associated with: malformations, cardiopulmonary adaptation and difficulties; asphyxia, thermoregulation, gastrointestinal and metabolic disorders, infections; hematologic problems and hyperbilirubinemia, fetal growth restriction, feeding, abuse and neglect
10.
Collaborative care of high-risk clients
11.
Special populations: adolescents, physically and/or mentally handicapped, advanced maternal age, substance abusers, sexual abuse and domestic violence
12.
Pharmacotherapeutics specific to nurse-midwifery care of the neonate
13.
Counseling, diagnosis, and management of perinatal infections: H1N1, Hepatitis,
Parvo, varicella, chorioamnionitis, pyelonephritis CMV, HSV, listeriosis, syphilis, toxoplasmosis
14.
Diagnosis and management of women’s health problems: abnormal breast findings, menstrual irregularities, osteoporosis.
LEARNING ACTIVITIES
Clinical simulations and laboratory, written exams, paper, discussion boards and oral presentations via Adobe Connect
CLINICAL EVALUATION
Clinical experience will be evaluated through faculty observation, verbal communication with the student, written work, and agency staff reports using a College of Nursing Clinical
Evaluation Form. Faculty reserve the right to alter clinical experiences, including removal from client care areas, of any student to maintain patient safety and to provide instructional experiences to support student learning.
Clinical evaluation will be based on achievement of course and program objectives using a
College of Nursing Clinical Evaluation Form. All areas are to be rated. A rating of Satisfactory represents satisfactory performance and a rating of Unsatisfactory represents unsatisfactory performance. The student must achieve a rating of Satisfactory in each area by completion of the semester in order to achieve a passing grade for the course. A rating of less than satisfactory in any of the areas at semester end will constitute a course grade of E. Satisfactory achievement of clinical competency is a requirement to receiving a course grade. Regardless of the classroom grade, a student receiving an Unsatisfactory evaluation in the clinical component of the course will be assigned a course grade of E.
The faculty member will hold evaluation conferences with the student and clinical preceptor at each site visit. The faculty will write a summary of each conference in an advisement note.
This summary will be signed by the faculty member and student. Final evaluation conferences with the faculty member are mandatory and will be held during the last week of each semester.
A student may request additional conferences at any time by contacting the clinical faculty member.
Students enrolled in advanced practice courses with a clinical component will use Clinical
Experience Form F to document clinical experience including hours, practice location and preceptor for their personal records. Students also assess their learning experience using Clinical
Site Assessment Form G. Completed Form G is collected by the faculty member and submitted to the Coordinator of Clinical Laboratories at the College. At the end of the clinical experience the student completes a self-evaluation and the faculty completes a student evaluation using the
College of Nursing Clinical Evaluation Form.
CLASSROOM EVALUATION
For students who achieve a satisfactory clinical grade, the letter grade for the course will be based upon the following:
GRADING SCALE
Course grades are determined by a variety of evaluative methods such as written exams, clinical performance, written papers, oral presentation, case studies, and class participation. The nursemidwifery specialty utilizes the following grading scale to compute grades:
A 95-100 (4.0)
A- 93-94 (3.67)
B+ 91-92 (3.33)
B 84-90 (3.0)
C 74-79* (2.0)
C- 72-73 (1.67)
D+ 70-71 (1.33)
D 64-69 (1.0)
B-
C+
82-83 (2.67)
80-81 (2.33)
D-
E
62-63 (0.67)
61 or below (0.0)
* 74 is the minimal passing grade
Examinations are presented remotely through Proctor U. Students should familiarize themselves with this software before taking an examination. There is an information section on Sakai regarding this.
Students’ tests will be maintained on file in the nurse-midwifery office. No copies of tests may be made by students. A student can review tests at any time but cannot remove them from the office. Downloading the exam from Sakai is prohibited, as is printing the exam.
Students must achieve an overall GPA of 3.0 or better in order to receive the Masters degree.
Exam I
Exam II
30% (Monday 06/11/12)
30% (Monday 07/30/12)
Paper
Case Studies/Discussion boards
Clinical Practice
25% (Monday 7/16/12 by 4 PM)
15% (varies/TBA)
Pass/Fail
Late Work Students are expected to turn in assignments when they are due. If advance arrangements are made with the faculty for due cause (e.g. extended illness, death in the family), an assignment may be turned in at a later date without penalty. Otherwise, assignments turned in late will be assessed a penalty of ten (10) percentage points the first 24 hours, plus five percentage point per day after the first 24 hours, including weekends. This is deducted from the final percentage grade.
REQUIRED
REQUIRED: All texts from previous MSN courses
American College of Nurse-Midwives (ACNM) http://www.acnm.org/
Core Competencies for Nurse-Midwifery Practice (2007)
The Standards for the Practice of Nurse-Midwifery (2003)
The ACNM Code of Ethics (2008)
REQUIRED TEXTS
Beckmann, C., Ling, F., Smith, R. & Barzansky, B. (2009) Obstetrics and Gynecology (6 th ed).
Philadelphia, PA: Lippincott Williams & Wilkins
Gabbe, S., Simpson, J. L., Niebyl, J. R., Galan, H., Goetzl, L., Jauniaux, E.R. & Landon, M (2007)
Obstetrics: Normal and Problem Pregnancies (5 th ed). Philadelphia, PA: Churchill Livingstone
Hatcher, R. A., Trussell, J., Nelson, A.L., Cates, W., Stewart, F., & Kowal, D. (2008). Contraceptive
technology (20 th ed.). New York, NY: Ardent Media.
Oxorn, H. (1986). Oxorn-Foote: Human labor and birth (5th sub ed.). Norwalk, CT: Appleton & Lange.
Schuiling, K.D., & Likis, F.E. (2012). Women’s gynecologic health . Sudbury ME: Jones & Bartlett.
Varney, H. (2004).
Varney’s midwifery
(4th ed.). Sudbury, ME: Jones and Bartlett.
RECOMMENDED TEXTS
Briggs, G.G, Freeman, R.K., & Yaffe, S.J. (2011). Drugs in pregnancy and lactation (9th ed.).
Philadelphia, PA: Lippincott Williams & Wilkins.
Cunningham, F. G., Leveno, K. J., Bloom, S.L., Hauth, J.C., Gilstrap, L. C., & Wenstrom, K.D. (2009).
Williams Obstetrics (23rd ed.). Columbus OH: McGraw-Hill.
Gordon, J. D., Rydfors, J., Druzin, M.L., Tadir, Y., El-Saved, Y., Chan, J., Lebovic, D., Langen, E. &
Fuh, K. (2007). Obstetrics, Gynecology and Infertility: Handbook for Clinicians; Pocket Edition.
Arlington, VA: Scrub Hill Press
Varney, H. (2009). Varney’s Pocket Midwife (2nd ed). Sudbury, ME: Jones and Bartlett.
Approved: Academic Affairs Committee: 2/01; 1/02
Faculty: 3/01; 2/02
UF Curriculum: 10/97; 11/01
5/14/12
9:00 – 10:00
10:00 - 12:00
12:00 –1:00
1:00 – 15:00
15:00-1700
5/15/12
8:00 – 9:00
9:00-noon
Noon-1:00
1:00 – 5:00
5/21/12
WEEKLY SCHEDULE
Monday
Course overview
Mirena IUS lab
Varney Chapter 19
Beckmann pp 231-233
Gabbe pp 578-579
LUNCH
Jane Houston CNM readings posted to Sakai
OB SIM LAB second floor
Elm Room
Suturing Lab (BRING YOUR KITS)
Nexplanon demonstration
Beckmann p 228
Tuesday
Videos and discussion
Shoulder dystocia, PPH
Beckmann p 111, 133-139
Oxorn chaper 22
Gabbe pp 466-481
Management of PPH and shoulder dystocia (use of Noelle simulator)
LUNCH
Breech delivery and malpresentations
Beckmann 110-111, Oxorn Chapters 15
– 18
Varney Chapter 30
Use of US for dating and cervical length
Gabbe pp 215-244
Infections in Pregnancy
Jane Houston CNM
Readings posted to Sakai
Jane Houston CNM
Brent Seibel MD
Students to present to each other via discussion board
Readings on Sakai
Beckmann pp 164-175
Handouts on Sakai
Brent Seibel MD
OB SIM LAB second floor
Kristin Stich Foerster CNM
OB SIM LAB second floor
OB SIM LAB second floor
OB SIM LAB second floor
OB SIM LAB second floor
5/29/12
5/28/12 is
Memorial Day
Gestational diabetes, GHTN, HELLP
Beckmann p 154-158, 175, 176-181
Varney pp 695-699
Gabbe pp 864-868, 874-881, Chapter 37
Readings
COURSE SYLLABUS NGR 6361C
Page 7
06/04/12
06/11/12
06/18/1
06/25/12
ACNM MEETING NO CLASSES
EXAM 1
Bleeding in the GYN patient
Beckmann 3,398-399 Varney 427-428,
Handouts on Sakai
Break week
07/02/12
7/4/12
HOLIDAY
Thyroid disease, growth restriction
Beckmann 158-159, 189-194
Gabbe 771-814, Chapter 38
7/09/12
7/16/12
Multiple gestation/Hepatitis
Beckmann 183-187, 168-169
Varney Chapter 8 & 30
Infertility
Beckmann 337-346
Handouts on Sakai
PAPER DUE
7/23/12
GI and Metabolic Problems in Pregnancy
GU Problems in Pregnancy
Beckmann 50
Varney pp 151-152, 551, 553, 739
07/30/128/06/12 EXAM II
FINAL EVALUATIONS DUE