Appendix 6 - European Heart Journal
advertisement

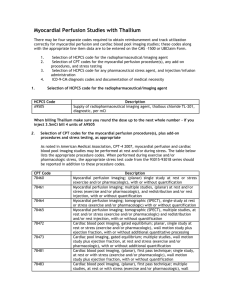
1 Online Exhibit B RWISE Cardiovascular Magnetic Resonance Imaging Core Laboratory: Manual of Operations (MOP) I. Background and Rationale Women with persistent signs and symptoms of myocardial ischemia are often likely to have no obstructive coronary artery disease (CAD) compared to obstructive CAD. We have described a high prevalence of limited coronary flow reserve (CFR) by direct left coronary artery Doppler catheter flow measurements and also limited subendocardial and mid-wall perfusion reserve by cardiac magnetic resonance imaging (CMRI) consistent with myocardial ischemia and coronary microvascular dysfunction (CMD) in these subjects. The NHLBI-sponsored Women’s Ischemia Syndrome Evaluation (WISE) documented that such subjects are at increased risk of adverse outcomes similar to those with obstructive CAD. However, it is unknown if limited subendocardial perfusion leading to ischemia is a mechanistic pathway for the signs, symptoms, morbidity and mortality in these subjects with no obstructive CAD. Prior data support that ranolazine improves angina and insulin resistance in CAD subjects and preliminary data suggests that it may improve myocardial perfusion in subjects with CMD who have no obstructive CAD. These data support the hypothesis that ranolazine may improve angina via an anti-ischemia mechanistic pathway. The major function of the cardiac magnetic resonance core laboratory (CMRC) is to systematically and objectively document the status of myocardial perfusion and left ventricular function in CMRI studies. II. Specific Aims and Purposes The principle purpose of the CMRC is to review and analyze CMRI data from all women enrolled who underwent CMRI. The CMRC will provide an interpretation of results by advanced imaging cardiologists and experienced CMRI analysts qualified to interpret these studies. Through this, we will reduce bias and inter-observer variability and increase accuracy/precision of study results. All interrogation of image data to be performed blinded to the patient identity or in the case of therapeutic trials, blind to therapy/group. The CMRI methods and acquisition are based on the NHLBI-sponsored Women’s Ischemic Syndrome Evaluation (WISE) CMRI protocol (9), modified for RWISE. Specifically, a) phasecontrast velocity mapping and b) late gadolinium enhancement were not included in RWISE to reduce magnet time and subject burden. WISE CMRI scans can be used to qualify subjects for RWISE. Specific aims (Based on the individual CMRI portions of the protocol, Figure 1): A. Left ventricular (LV) structure and function. a. Measure LV volumes (end-diastole, end-systole) and LV mass. b. Calculate diastolic filling curve (volume over time) from the whole heart cine imaging (stack of short axis cine images from the base to the apex) and from this, obtain variables of early and late peak filling rate (PFR) and time to PFR (tPFR). c. Documentation of patient size (body surface area) and heart rate are required. 2 B. Myocardial Perfusion. a. Calculate global, midventricular, subendocardial, and subepicardial myocardial perfusion reserve index (MPRI) for first pass perfusion performed at pharmacologic stress and cold pressor stress. b. Systematic approach to calculating the MPRI as detailed below. C. Late gadolinium enhancement. a. In subjects who had late gadolinium enhancement imaging performed 5 minutes post cold pressor testing (as part of the WISE study), determine the presence of scar and scar pattern as seen on late gadolinium enhancement. III. CMRI Methods A. Pre-CMRI Instructions The following instructions are provided to the subject in preparation for CMRI: a. Please fast before your appointment. Nothing to eat or drink for 12 hours prior to your appointment (except you may drink water.) No caffeine or smoking 24 hours prior to your appointment (i.e. tea, coffee, chocolate, soda, Anacin/Excedrin). b. Please discontinue your use of: Nicotine 4 hrs prior to your appointment. Long-acting nitrates, short-acting calcium channel blockers, alpha blockers and beta blockers, ACE/ARB inhibitors, Renin and Aldosterone Inhibitors for 24 hours prior to testing. Long-acting calcium channel blockers for 48 hours prior to your testing. Sublingual nitroglycerin up to 4 hours prior to testing. Bring your medications with you so that you can take them after the MRI. B. Supplies and materials required for perfusion imaging: a. Gadolinium perfusion: i. Infusion pump – CMRI compatible. ii. Gadolinium loaded with dose total 0.2 mmol/ kg – with additional top up of 5 ml to allow for tubing length dead space. b. Adenosine stress: i. Infusion pump. ii. Infusion syringe. iii. IV cannula x 2 (one each antecubital fossa ideally or separate on same arm with adenosine downstream to gadolinium) (minimum 20g iv for adenosine and 18g iv for gadolinium). iv. 5 piece tubing 38 inch long length (190 inches) that is primed with adenosine and not saline. v. Adenosine 140mcg/kg over 5 min (do not administer gad <3 min adenosine infused). vi. BP/HR monitor (attach to arm with adenosine cannula and NOT to arm with gadolinium cannula). OR 3 c. Regadenoson Stress (if did not tolerate prior Adenosine stress) i. Infusion syringe. ii. IV cannula x 2 (one each antecubital fossa ideally or separate on same arm with Regadenoson downstream to gadolinium) (minimum 20g iv for Regadenoson and 18g iv for gadolinium). iii. Regadenoson 0.4 mg/5 mL per syringe. iv. BP/HR monitor (attach to arm with adenosine cannula and NOT to arm with gadolinium cannula). d. Cold Pressor Stress: i. Ice hand wrap from freezer. ii. Low temperature thermometer to document 4 degrees C. iii. Towels. C. Sequence of Events: Adenosine Stress (See Figure 1a) 1. Adenosine dose 140mcg/kg/min for 5 min. 2. Sequence of events: adenosine stress, rest, cold pressor. 3. Gadolinium 0.05 mmol/kg for rest, adenosine stress and cold pressor doses. Regadenoson Stress (See Figure 1b) 1. Regadenoson 0.4 mg/5 mL per syringe. 2. Sequence of events: rest, cold pressor, and then regadenoson stress. 3. Gadolinium 0.05 mmol/kg for rest, regadenoson stress and cold pressor doses. LV function imaging (performed pre- contrast) Pre- Contrast TIME ZERO – 10 minutes 1. Scout imaging (anatomic three plane) to check the HEART is in the magnet ISOCENTER. 2. remove patient and re- center if needed. 3. Axial HASTE through chest. 4. Scout for LV axis. 5. SSFP cine left ventricle planned from 1 slice above the mitral valve to 1 slice below the apex. Parameters: a. 8mm slice thickness / skip 2mm, matrix = 256. b. Minimum 25 phases/ cycle, retrospective gating. c. FOV according to patient (decrease to maximize resolution). 6. SSFP 4 chamber, 2 chamber, and LVOT view cine imaging. Bolus first pass perfusion procedures (see Table 1 for CMRI sequence parameters): TIME 10- 20 minutes Adenosine stress 1. baseline imaging to set up pulse sequence and copy sequence ready for imaging: 4 a. Copy image parameters from representative basal, mid and distal short axis cine images. Be sure that the cine image at the base includes myocardium throughout the cardiac cycle on review of image data (ie does not partial volume atrium). b. Check for wrap and open FOV if required. 2. remove patient partially from magnet (do not lose isocenter position). 3. measure baseline HR and BP. 4. hook up adenosine and gadolinium infusion lines after first re- checking patency of iv catheters. 5. double check lines are securely attached. 6. start / check clock time and infuse adenosine. 7. note peak HR at 1.min 30 seconds. 8. patient placed back into magnet and close door at 1 min 45 seconds. 9. breathing instructions. 10. start pulse sequence at 2 minutes of adenosine infusion. 11. infuse 0.05 mmol/kg gadolinium bolus once pulse sequence is triggered. 12. recover patient part way out of magnet with adenosine turned off immediately on completion of imaging. 13. measure BP immediately post gadolinium / pulse sequence and stop IV adenosine. 14. record response on check sheet (note peak HR, flush, CP, SOB etc). WAIT minimum 10 minutes post gadolinium infusion and then proceed. TIME 30 – 35 minutes Rest perfusion 1. Copy same baseline imaging parameter above to set up pulse sequence. 2. Patient goes back into the magnet. 3. Measure baseline HR and BP. 4. Prime gadolinium infusion pump. 5. Double check line is securely attached. 6. Breathing instructions. 7. Infuse 0.05 mmol/kg gadolinium bolus once pulse sequence is triggered. WAIT minimum 10 minutes post gadolinium infusion and then proceed. TIME 45- 50 minutes: Cold pressor stress 1. Copy same baseline imaging parameter to set up pulse sequence. 2. Patient remains in the magnet. 3. Measure baseline HR and BP. 4. Prime gadolinium infusion pump. 5. Double check line is securely attached. 6. Start 2 minute timer and check clock time. 7. Apply ice hand wrap to hand and forearm. 8. Note peak HR at 1.min 45 seconds by starting BP cuff at 1 min (not same arm as gadolinium). 9. Breathing instructions. 10. Start pulse sequence at 2 minutes of cold stress. 11. Infuse 0.05 mmol/kg gadolinium bolus as soon as the pulse sequence is triggered. 5 12. Recover patient part way out of magnet with cold pack off immediately on completion of imaging. 13. Record response on check sheet (note peak HR and BP, CP, pain etc). CMRI with Regadenoson (Lexiscan) Lexiscan will be used for the CMRI for subjects who cannot take adenosine due to mildmoderate stable chronic asthma. The sequence of CMRI acquisition in this case will be rest perfusion as mentioned above, followed by cold presser followed by hyperemia with Lexiscan infusion. Upon completing of the CMRI with Lexiscan, patient will then be transported to PACU for continuous 12 Lead ECG monitoring for 90 minutes. IV. Transmission of Data to the Core Laboratory Once patients are enrolled, baseline and any follow-up CMRI data sets should be sent via fedex in DICOM format on a CD to the core laboratory. CMRI data sets should be sent to the core laboratory within one week of completing the CMRI. Acquisition forms (technician worksheet) to record procedural information such as contrast agent amount, injection rate, patient blood pressure, and heart rate information will be provided. V. Core Laboratory Storage, Filing, Retrieval and Transmission of Data All CMRI data sets submitted to the core laboratory will be logged into a computerized database and stored under appropriate conditions to preserve their integrity. Access to data will be restricted to CMRC personnel and electronic information stored on secure, password protected computer systems. Back-up copies of data, stored on CDs will be filed in locked fireproof cabinets on site. To transmit data electronically or via paper copy, participants will only be identified by a secure code, and no personal identifiers will be included in transmissions. Data will be handled in compliance with HIPAA regulations. Off-site data storage will be used to store data in CD format, as part of a disaster recovery plan. At the CMRI, database management including determination of the validity of data entry, security, and back-up will be performed. All forms developed for the study will undergo a monthly Form Control evaluation to ensure that the correct forms are in use. VI. Interpretation and Review of CMRI Data VI. 1. Introduction All CMRI datasets from patients enrolled will be reviewed by the core laboratory within one week of reception. Additional datasets may be reviewed (~10% re-reads). Computer records of the regions used in CMRI analysis will be stored at the CMRC so that analysis of the same myocardial segments using the same views can be performed at follow-up. V1. 2. Image Quality and RWISE Eligibility All datasets will be scored based on Image Quality (Excellent, Good, Fair, Poor, Uninterpretable). All patients with CMRI Image Quality scores of Excellent, Good, or Fair can qualify with either their visual score (≥10% reversible perfusion abnormality indicated by a visual read qualitative summed severity score) or MPRI value. Patients with a CMRI Image Quality Score of Poor can only qualify with their MPRI value. All patients with a CMRI Image Quality Score of uninterpretable are excluded from RWISE. In October 2011, a Protocol Amendment was approved to remove the visual score as an enrollment criteria and MPRI cutoff was set at <1.8 for eligibility. 6 In December 2013, a Protocol Amendment was approved to increase the MPRI eligibility to ≤2.0. VI. 3. Quality Assurance Interpretation of each CMRC dataset will begin with an assessment of study quality. Regular phone conference call discussions of quality will take place. VI. 4. Data Collection Collect and export the necessary variables into a corelab spreadsheet. VI. 5. Quality Control CMRC is a corelab for the CMRI part of the RWISE Study. The core lab will collect/receive raw CMRI CDs from both Florida and CSMC site. Edward Gill (CMRI technologist) will extract and back-up the CMRI data at two different locations (local hard drive and online server). He will process the data in three portions as follows: 1. Structure and Function. 2. Stress vs rest perfusion. 3. Cold pressor vs rest perfusion. 4. Diastolic filling. Processed data will be checked for quality control and transcribed by Dr. Louise Thomson, Dr. Daniel Berman, or appropriately experienced research fellow (under their supervision). An excel spreadsheet located on the server will be updated with the results. This includes MPRI analysis in all 16 segments in 3 layers (global MPRI, subendocardial, and subepicardial), rest first pass perfusion maximal up slope value, function analysis (ejection fraction and cardiac output, volumes, and diastolic filling parameters) and heart rate and blood pressure values obtained from CMRI forms. The CMRC is also the CMRI corelab for the NLHBI-sponsored WISE study and has previously published regarding reproducibility of MPRI (Goykhman P et al, 2012) as well as the sensitivity and specificity for MPRI to detect CMD defined by invasive coronary reactivity testing (Thomson LE et al, 2015). The core lab will communicate with the Florida and CSMC coordinators regarding receipt of the CMRI forms, clinical CMRI report and CMRI raw data CD and the coordinators will update core lab regarding enrollment spreadsheet and send the mentioned data to the core lab. This will be performed at least monthly. The details of study enrollment as well as analyzed and processed data will be discussed during monthly CMRI core lab call. VI. 6. CMRI Analysis 1). Left Ventricular Structure and Function Quantitative CMRI analysis will be performed with a computer based system (CAAS MRV 3.3.1 Netherlands). Epicardial contours will be manually traced at end-diastole and end-diastole. A reference point will be marked as the point of insertion of the right ventricle into the left ventricle on the inferoseptal surface. Endocardial contours are propagated and manually adjusted to include the papillary muscles in the left ventricular (LV) cavity, between the end-systolic frame to the end-diastolic frame, to provide endocardial contours during diastole. Based on the contour information, LV end-diastolic/end-systolic volumes, and ejection fraction (EF) % (stroke volume/end-diastolic volume) are derived. Papillary muscles were included in the measurement 7 of myocardial mass (calculated from the end-diastolic frames) and excluded in the measurement of volumes. Volumetric diastolic filling are plotted over time to calculate peak filling rate (PFR) and time to PFR (tPFR) in early and active phases of diastole. 3). Myocardial Perfusion (Table 1: CMRI perfusion parameters) 3a). Qualitative Analysis Myocardial perfusion will be based on 17-segment AHA model using 5 point scoring system: 0normal, 1-mildly reduced, 2-moderately reduced, 3-severely reduced, 4-absent uptake. The apical segment (17th segment) is not assessed since the first pass perfusion images are acquired in short axis and are not sliced all the way to the apex. Summed Stress Score is obtained by adding the scores of the 16 segments of the stress perfusion images. Perfusion defects are categorized depending on the percentage of involved myocardium, which is calculated by the sum of the severity scores divided by 64 [the product between the number of segments analyzed (16) and the worst possible uptake score (4)], then multiplied by 100. 3b). Quantitative analysis of the first pass perfusion images will be performed using CAAS MRV 3.3.1 software (Pie Medical Imaging B.V., Netherlands) (Figure 2). Observers in a systematic way, according to the software manufacturer’s specifications, will manually place the epicardial and endocardial contours of the left ventricular (LV) myocardium for three slices (basal, mid, and apical). STEP 1. The epicardial contours are manually adjusted to sample data from the LV myocardium alone and not to include any portion of the right ventricular cavity at the septal margin. The endocardial contours are placed to include the papillary muscles; care was taken to exclude blood pool activity and to exclude any linear dark rim artifact at the LV cavity/endocardial border. The LV cavity region of interest was manually adjusted to include the region of maximal signal intensity within the cavity and to exclude papillary muscle. The left-right ventricular (LRV) junction point is placed at the inferior portion of the interventricular septum. STEP 2. The intensity over time curves at rest and stress for an AHA 17-segments model are automatically generated using these adjusted contours. The apical segment, (17th segment) is not calculated since the first pass perfusion images are acquired in short axis and are not sliced all the way to the apex. The curves should be inspected for inconsistencies, with repeat adjustment of contours if needed. STEP 3. The starting point (T0 cycle) and the ending point (T end) of the upslope curve are then chosen in order to obtain the intensity over time curves. T0 is placed at the beginning of the upslope of the LV cavity curve and T end is placed at the end of the upslope of the segments. The intensity over time curves are then used to calculate the relative upslope (RU), defined as the ratio between the maximum upslope of the selected curve, which corresponds to the specific myocardial segment, divided by the maximum upslope of the left ventricular cavity curve. Myocardial perfusion reserve index (MPRI) for each segment is then calculated by RU at stress divided the RU at rest. The data is then entered into the spreadsheet for corresponding segments in global (transmural), subepicardial and subendocardial regions. Mid-ventricular MPRI is defined as the mean MPRI in AHA segments 7-12. In the case of 2-slice image data being acquired as a result of high stress heart rate, data were recorded for 12 segments, and mean MPRI was the average of 12 segments. 4) Late Gadolinium Enhancement Late gadolinium enhancement images from prior WISE CMRI scans of the subject were read by an experienced investigator to identify and describe areas of late enhancement. 8 VII. Resources The CMRC is located in the S. Mark Taper Foundation Imaging Center, a state-of-the-art, multimodality imaging facility that opened in late 2002. The 121,000 square-foot center extends from the north tower of Cedars-Sinai Medical Center on two levels. The nuclear imaging facilities, which include clinical nuclear medicine and nuclear cardiology, consist of approximately 16,000 square feet of clinical space extending on the street level of the Imaging Center. The facility includes 2,500 square feet of office space and working areas (secretarial, reading room, conference room, etc). The Cardiac Imaging and Nuclear Medicine research program staff are accommodated in 8,000 square feet in the lower level, north tower of the main building of the Medical Center. The CMRC is located within this facility. Taper Imaging as a whole performs 320,000 procedures per year; approximately 40% is film-less. Average daily volume on PACS is 18-22 GB per day. Cedars-Sinai Medical Center created an optical fiber "imaging backbone" which ties the Cardiology, Imaging (including Radiology, Magnetic Resonance, Nuclear Medicine, Computed Tomography, Computed Radiography, Ultrasound, Vascular Ultrasound, Fluoroscopy, Angiography, and Digital Mammography and Medical Physics) resources and scanners together to PACS using TCP/IP protocols across Ethernet. The Optical Fiber Backbone (OFB) supports a wide variety of technologies including imaging, graphics and text, voice, video and virtually any other data type. The OFB also provides critical gateways to strategic off campus business partners, such as UCLA's School of Medicine. Security measures have been built into the system to protect patient privacy and hospital security. All research computers are in the same intra-net directly connect to the Kodak PACS, MRI, CT and nuclear workstations. The Taper Imaging Center has 6 state-of-the-art 1.5 Tesla Siemens MRI scanners of which two are equipped with cardiac specifications (Siemens Sonata) and one is dedicated to cardiac MR (Siemens Magnetom Avanto). There are 5 Siemens Leonardo 3-D workstations. Post processing and image review is performed on Leonardo workstations utilizing Argus software. VIII. CMRC Investigators Daniel Berman, M.D., is the Director of Cardiac Imaging and Nuclear Cardiology at Cedars-Sinai Medical Center and a Professor of Medicine at the David Geffen School of Medicine at the University of California at Los Angeles, directing programs in Cardiac SPECT, PET, MRI and CT. He is also a fellow of the American College of Cardiology and the American Heart Association's Council on Clinical Cardiology. Dr. Berman has written more than 500 original manuscripts, chapters and books. He has been awarded numerous grants and continues to lead the specialty of cardiac imaging in generating outcome data for cost-effective analysis of cardiac status. Louise Thomson, M.B.Ch.B. is a physician with the Cedars-Sinai Imaging Group and director of the Cedars-Sinai Cardiovascular Imaging Fellowship program. She received her medical degree from the University of Otago, New Zealand and trained in internal medicine, cardiology (Auckland, NZ) and nuclear medicine (Sydney, Australia) before moving to the United States in 2002 to work as a research associate at the Duke Cardiovascular Magnetic Resonance Center. She joined the Cedars-Sinai Medical Center faculty in 2003. 9 References 1. Cerqueira MD, Weissman NJ, Dilsizian V, et al. Standardized myocardial segmentation and nomenclature for tomographic imaging of the heart: a statement for healthcare professionals from the Cardiac Imaging Committee of the Council on Clinical Cardiology of the American Heart Association. Circulation. 2002;105:539-542. 2. Doyle M, Fuisz A, Kortright E, et al, The impact of myocardial flow reserve on the detection of coronary artery disease by perfusion imaging methods: an NHLBI WISE study. J Cardiovasc Magn Reson. 2003;5(3):475-85. 3. Doyle M, Pohost GM, Kortright E, Shaw LJ, Johnson D, Rogers WJ, Fuisz A, Reism SE, Sharaf BL, Pepine CJ, Bairey Merz CN, Mankad S, Vido DA, Kelsey SF, Olson MB, Biederman RWW. In Women with Symptoms of Ischemic Heart Disease, Global and Regional Myocardial Perfusion Status by MRI Better Assigns Risk: Results from the NHLBIsponsored Women’s Ischemia Syndrome Evaluation (WISE). J Am Coll Cardiol. 2004;43[Suppl A]:266A. 4. Goykhman P, Mehta PK, Agarwal M, Shufelt C, Slomka PJ, Yang Y, Xu Y, Shaw LJ, Berman DS, Merz NB, Thomson LE. Reproducibility of myocardial perfusion reserve variations in measurements from post processing using commercially available software. Cardiovasc Diagn Ther. 2012 Dec;2(4):268-77. 5. Maceira AM, Prasad SK, Khan M, Pennell DJ. Normalized Left Ventricular Systolic and Diastolic Function by Steady State Free Precession Cardiovascular Magnetic Resonance. J. Cardiovasc Magn Reson. 2006;8(3):417-26. 6. Nelson MD, Szczepaniak LS, Wei J, Haftabaradaren A, Bharadwaj M, Sharif B, Mehta P, Zhang X, Thomson LE, Berman DS, Li D, Bairey Merz CN. Diastolic dysfunction in women with signs and symptoms of ischemia in the absence of obstructive coronary artery disease: a hypothesis-generating study. Circ Cardiovasc Imaging. 2014 May;7(3):510-6. 7. Shoucri RM. Performance of the left ventricle based on pressure-volume relation. J of Biomed Eng. 1990;12:482-488. 8. Shufelt CL, Thomson LE, Goykhman P, Agarwal M, Mehta PK, Sedlak T, Li N, Gill E, Samuels B, Azabal B, Kar S, Kothawade K, Minissian M, Slomka P, Berman DS,Bairey Merz CN. Cardiac magnetic resonance imaging myocardial perfusion reserve index assessment in women with microvascular coronary dysfunction and reference controls. Cardiovasc Diagn Ther. 2013 Sep;3(3):153-60. 9. Thomson LE, Wei J, Agarwal M, Haft-Baradaran A, Shufelt C, Mehta PK, Gill EB, Johnson BD, Kenkre T, Handberg EM, Li D, Sharif B, Berman DS, Petersen JW, Pepine CJ, Bairey Merz CN. Cardiac magnetic resonance myocardial perfusion reserve index is reduced in women with coronary microvascular dysfunction. A National Heart, Lung, and Blood Institute-sponsored study from the Women's Ischemia Syndrome Evaluation. Circ Cardiovasc Imaging. 2015 Apr;8(4):e002481. 10 Table 1: CMRI Pulse Sequence Sequence Gradient echo-EPI Hybrid TR per slice 148 ms TE 1.1 ms BW 1420 Hz/pixel Echo train length 4 Flip angle 20° Slice thickness 8 mm Image matrix 160 x 70 pixels In-plane resolution 2.7 x 2.2 mm2 Parallel imaging (GRAPPA) factor 2 # slices/heartbeat 3 11 Figure 1a. CMRI protocol with Adenosine Figure 1b. CMRI protocol with Regadenoson 12 Figure 2. Quantitative CMRI analysis using CAAS MRV 3.3.1 software A.1 A.2 RV LV B.1 B.2 RV LV First pass, rest (top)-stress (bottom) perfusion image through short axis two chamber views; showing mid slice right ventricle (RV) and left ventricle (LV). Normal myocardial enhancement at rest (A.1) and circumferential area of subendocardial hypoperfusion during stress (B.1). Epicardial (blue) and endocardial (red) contours at rest (A.1) and stress (B.1) used to obtain intensity over time curves at rest (A.2) and stress (B.2), respectively. Intensity over time curves are used to calculate the relative upslope (RU), defined as the ratio between the Maximum upslope of the selected curve divided by the Maximum upslope of the LV cavity curve. Myocardial perfusion reserve index (MPRI) = Relative Upslope (RU) at stress / RU at rest.