Shashidhar - journal of evidence based medicine and healthcare
advertisement

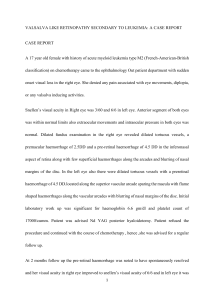
DOI: 10.18410/jebmh/2015/584 ORIGINAL ARTICLE ND YAG POSTERIOR HYALOIDOTOMY: A SAFE AND COSTEFFECTIVE APPROACH FOR THE MANAGEMENT OF PRE-MACULAR HAEMORRHAGE IN VALSALVA RETINOPATHY Shashidhar S1, Manasa Penumetcha2 HOW TO CITE THIS ARTICLE: Shashidhar S, Manasa Penumetcha. ”ND YAG Posterior Hyaloidotomy: A Safe and Cost-Effective Approach for the Management of Pre-Macular Haemorrhage in Valsalva Retinopathy”. Journal of Evidence based Medicine and Healthcare; Volume 2, Issue 28, July 13, 2015; Page: 4107-4113, DOI: 10.18410/jebmh/2015/584 ABSTRACT: AIM: To assess the safety and efficacy of Nd YAG posterior hyaloidotomy or membranotomy as a treatment modality for pre-macular haemorrhage in valsalva retinopathy. METHODS: This is a retrospective study of 10 eyes of 10 patients who underwent Nd YAG posterior hyaloidotomy for pre-macular haemorrhage in valsalva retinopathy from January 2006 to November 2014. Post procedure results were assessed in terms of clearance of pre macular haemorrhage, improvement in visual acuity, complications of procedure if any. RESULTS: 10 eyes of 10 patients with valsalva retinopathy were studied. These patients presented within 4 weeks of onset of symptoms. The pre-macular haemorrhage of more than 3DD seen in association with valsalva retinopathy were included and drained into the vitreous cavity using Nd YAG laser. It was observed that 9 out of 10 patients had a vision of 6/12 or better (90%) out of which 7 had 6/6 vision (70%). No patients had any complications. CONCLUSION: Nd YAG laser posterior hyaloidotomy or membranotomy can be considered to be a safe, inexpensive, nonsurgical treatment option for the management of pre macular haemorrhage valsalva retinopathy. KEYWORDS: Nd YAG-Neodimium yittrium aluminium garnett, ILM-Internal Limiting membrane, Valsalva retinopathy. INTRODUCTION: Valsalva retinopathy was first described by Thomas Duane in 1972 as “A particular form of retinopathy which was pre-retinal and hemorrhagic in nature, secondary to a sudden increase in intrathoracic pressure”.1 Following a valsalva manoeuvre, that is forcible exhalation effort against a closed glottis there is a sudden rise in intrathoracic pressure leading to a reduced venous return to the heart, decreasing the stroke volume subsequently increasing the venous system pressure. This is transmitted or transferred to the eye as a sudden increase in the intraocular venous pressure causing the retinal capillaries to spontaneously rupture.2,3,4,5,6 Individuals with history of vascular diseases such as diabetes, hypertension, sickle cell disease, anemia, idiopathic thrombocytopenic purpura and other blood dyscrasias and patients with history of ocular venous occlusion are at increased risk for retinopathy to occur following valsalva manoeuvre.7,8,9 Valsalva retinopathy is characterized by sudden painless loss of vision or central scotoma. Affected individuals are generally healthy with normal eyes and positive history of valsalva stress like strenuous exertion, emesis, violent coughing, sexual intercourse, labour, blowing musical instruments, compression injuries. The classical sign is a small, solitary, well-circumscribed preJ of Evidence Based Med & Hlthcare, pISSN- 2349-2562, eISSN- 2349-2570/ Vol. 2/Issue 28/July 13, 2015 Page 4107 DOI: 10.18410/jebmh/2015/584 ORIGINAL ARTICLE retinal haemorrhage at the macula which is not associated with retinal, choroidal or any systemic disease. In some instances, the solitary haemorrhage may be fairly large.10 The anatomical location of the pre-macular haemorrhage is described as sub internal limiting membrane, subhyaloid, or a combination of both. However it is usually not possible to distinguish clinically between a subhyaloid and sub-ILM haemorrhage.10,11,12 In majority of cases it resolves spontaneously without compromising visual acuity however, even a small pre-macular haemorrhage may take several months to clear.13 Various available modalities of management are: 1. Observation for small haemorrhage. 2. Posterior hyaloidotomy/Membranotomy using Nd YAG laser or double frequency YAG laser. 3. 3-Port pars plana vitrectomy. 4. Injection of tissue plasminogen activator with pneumatic displacement of subhyaloid haemorrhage. Nd YAG laser treatment is a non-invasive method which enables the drainage of extensive pre-macular haemorrhage into the vitreous cavity and facilitates the absorption of blood leading to a faster improvement in visual acuity by clearing the macular area. There are several reports presenting results of Nd YAG laser treatment in patients with pre macular haemorrhage for various aeitiologies like proliferative diabetic retinopathy, valsalva retinopathy, macroaneurysm, retinal vein occlusion and Tersons syndrome.14,15,16 In this study 10 patients of valsalva retinopathy with pre-macular haemorrhage more than 3 disc diameters in size and duration less than 4 weeks were included. MATERIALS AND METHODS: It is a retrospective study including 10 eyes of 10 patients from January 2006 to November 2014. Inclusion criteria were patients with pre-macular haemorrhage because of valsalva retinopathy with duration of presentation being less than 4 weeks. Exclusion criteria considered was premacular haemorrhage due to other causes, media opacities like cataract, vitreous haemorrhage etc. that would interfere with the procedure and any other causes which would have influence on the final visual outcome. Pre and post treatment evaluation was included in the form of best corrected visual acuity, detailed anterior and posterior segment evaluation. Horizontal and vertical diameter of pre-macular haemorrhage was measured in comparison with disc using calipers in digital imaging system. Nd YAG laser was applied through a slit lamp using the Goldmann three mirror. Laser settings used were single burst, Q switched mode started with 2mJ with increments of 1mJ. Maximum energy used was upto 7mJ and cumulative energy never exceeded 15-18mJ. Site of laser application was the most dependent part of the haemorrhage avoiding the fovea and major blood vessels. For larger haemorrhages 2 openings were made for complete clearance of the haemorrhage. 2 out of 10 eyes needed repeat procedure on day 3 in view of blockage of the opening. Follow up was done on day 3, 1st week, 2nd week, 1st month, 3rd month, 6th month and yearly thereafter for 2 years. J of Evidence Based Med & Hlthcare, pISSN- 2349-2562, eISSN- 2349-2570/ Vol. 2/Issue 28/July 13, 2015 Page 4108 DOI: 10.18410/jebmh/2015/584 ORIGINAL ARTICLE OUTCOME MEASURES: All patients were studied for decrease of pre-macular haemorrhage, improvement of visual symptoms and complications of the procedure if any. RESULTS: Sl. No. Age/Sex 1 2 3 4 5 6 7 8 9 10 25yrs/F 28yrs/M 28yrs/F 44yrs/M 30yrsF 20yrs/M 25yrs/M 25yrs/M 32yrs/M 45yrs/M Size of haemorrhage 3.75DD 3.25DD 6.5DD 5.25DD 4.75DD 3.5DD 3DD 3.5DD 4DD 3DD Duration of presentation 1 Week 3 Days 3 Days 5 Days 5 Days 2 Weeks 4 Weeks 10 Days 1 Week 2 Weeks Table 1 Pre laser vision Total Energy used Post laser vision HM+ HM+ HM+ HM+ HM+ HM+ CFCF CFCF CFCF CFCF 8mJ 6mJ 4mJ 5mJ 4.5mJ 8mJ 10mJ 8mJ 13mJ 14mJ 6/6. 6/6. 6/6p. 6/18. 6/6. 6/6. 6/12. 6/6p 6/6. 6/12. The study included 10 Eyes of 10 patients in the age group of 20-45yrs average age being 30.2yrs. 7 patients were males while 3 were females. Right eye was affected in 7 out of 10 patients. Size of pre-retinal haemorrhage was between 3.00DD to 6.5DD. Duration of visual symptoms was less than 1 week in 4 patients, 1-2 weeks in 3 patients and 2-4 weeks in 3 patients. Following the procedure entrapped blood was released into vitreous cavity and macular area was cleared by 1st week in most patients and in all patients by 3-4 weeks. Initial few days following the intervention patients complained of floaters which subsided in all except 1 patient. 2 out of 10 patients needed a repeat procedure on day 3 of follow up. Visual acuity at presentation ranged from hand movements to counting fingers at 1meter. Visual acuity improved to 6/6 in 7 patients 6/12 in 2 patients and 6/18 in one patient who had vitreous haze at 1month follow up. No complications like retinal or choroidal haemorrhage, retinal detachment, macular hole were seen in our study. Posterior hyaloidotmy or membranotomy was 100% successful in our study and no patient needed other additional procedures. DISCUSSION: The pre-macular haemorrhage is located at the vitreoretinal interface, the most common site being posterior pole at the pre-macular bursa. Sudden increase in intraocular venous pressure following valsalva manoeuvre results in a spontaneous rupture of retinal perifoveal capillaries resulting in a pre-macular haemorrhage. J of Evidence Based Med & Hlthcare, pISSN- 2349-2562, eISSN- 2349-2570/ Vol. 2/Issue 28/July 13, 2015 Page 4109 DOI: 10.18410/jebmh/2015/584 ORIGINAL ARTICLE Small haemorrhages tend to resolve spontaneously without leaving any visual disturbance. A slowly resolving large subhyaloid or sub internal limiting membrane haemorrhage would prolong the contact of retina with haemoglobin and iron which has the possibility of damaging the retina in the form of macular pigmentary changes and epiretinal membranes leading to reduction in visual function which may be irreversible.17,18 The exact location of the pre-macular haemorrhage is still unclear. It is difficult to determine the location of the pre-macular haemorrhage biomicroscopically, but presence of glistening light reflex and fine striae on the surface of haemorrhage seen clinically is indicative of sub ILM haemorrhage. Shukla et al19 reported the optical coherence tomography (OCT) results of two patients of valsalva retinopathy and the OCT demonstrated two distinct membranes: highly reflective being internal limiting membrane and overlying patchy membrane with low optical reflectivity consistant with posterior hyaloids. The study concluded that the plane of pre-macular haemorrhage in Valsalva retinopathy is probably under ILM. It also indicated that only when both ILM and the posterior hyaloid are visible on OCT can the location of blood be ascertained. In our study OCT was done in a few patients after the procedure which shows reflective membranes one in vitreous cavity and other on the retinal surface (Fig 3a, 3b). In 1988 Faulborn first described the application of Q-switched Nd YAG laser to subhyaloid haemorrhage.14 Ulbig et al20 studied 21 eyes with pre-macular subhyaloid haemorrhage of various causes. Visual acuity improved in 16 out of 21 eyes within 1 month, 7 patients required additional vitrectomy due to vitreous haemorrhage, macular hole was reported in one of the patients with size of subhyaloid haemorrhage being 1DD. There was failure in draining a clotted haemorrhage of 35 days duration into the vitreous cavity. Following this the author advocated laser therapy in patients with size of haemorrhage more than 3 DD and used energy level below 9mJ and a shorter duration of presentation. In our study minimum size of haemorrhage was 3 DD and the laser energy used was 2mJ at the start, with an increment of 1mJ and never exceeded beyond 7mJ. In our study laser procedure was 100% successful in releasing the trapped blood and the visual acuity was 6/12 or better, which is in 90% patients. CONCLUSION: In accordance with other studies the improvement in visual acuity was faster and safer in our study. The procedure should be considered in young and healthy patients as they belong to the working population for whom rapid restoration of visual acuity is important. Therefore Nd YAG laser Posterior hyaloidotomy or membranotomy can be considered as an ideal mode of management provided the size of haemorrhage is more than 3DD and of shorter duration. It is a safe, inexpensive, nonsurgical treatment option. J of Evidence Based Med & Hlthcare, pISSN- 2349-2562, eISSN- 2349-2570/ Vol. 2/Issue 28/July 13, 2015 Page 4110 DOI: 10.18410/jebmh/2015/584 ORIGINAL ARTICLE COLOR PLATES: Fig. 1: Pre-macular haemorrhage in Valsalva retinopathy in 30-yr old female patient managed with Nd- YAG laser hyaloidotomy Fig. 2a: Immediate post-laser fundus Fig. 2b: Day 3 follow-up of same patient Fig. 3a: Pre laser OCT Fig. 3b: Post laser OCT J of Evidence Based Med & Hlthcare, pISSN- 2349-2562, eISSN- 2349-2570/ Vol. 2/Issue 28/July 13, 2015 Page 4111 DOI: 10.18410/jebmh/2015/584 ORIGINAL ARTICLE BIBLIOGRAPHY: 1. Duane TD, Valsalva hemorrhagic retinopathy. Trans Am Ophthalmol Soc. 1972; 52: 298313. 2. Chandra P, Azad R, Pal N et al. Valsalva and Purtscher’s retinopathy with optic neuropathy in compressive thoracic injury. Eye Aug 2005; 19(8) 914-915. 3. Choi SW, Lee SJ, Rah SH. Valsalva retinopathy associated with fibreopticgastroenteroscopy. Can J Ophthalmol Aug 2006: 41(4): 491-493. 4. Lee VY, Liu DT, Chan WM. Valsalva retinopathy as a complication of colonoscopy. J. ClinGastroentrol, Aug 2005 39(7) 643. 5. Saricaoqlu MS, Kalayci D, Guven D et al. Decompression retinopathy and possible risk factors. ActaOphthalmol Feb 2009: 87(1) 94-95. 6. Abdullah S Al-Mujaini, Carolina C Montana. Valsalva retinopathy in pregnancy a case report J Med Care reports Apr 7. 2008. 7. Androudi S, Ahmed M, Brazitikas P. Valsalva retinopathy: Diagnostic challenge in a patient with pars planitis. Acta Ophthalmolscand. April 2005: 83(2) 256-257. 8. Karaqiannis D, Greqor Z. Valsalva retinopathy associated with idiopathic thrombocytopenic purpura and positive antiphospholipid antibodies. Eye (Lond). March 10 2006. 9. Mansour AM, Salti HI, Han DP et al. Ocular findings in aplastic anemia. Ophthalmologica 2000; 214(6); 399-402. 10. Guyer DR,Yannuzzi LA etalRetina:Macula-vitreous. Philadelphia: W.B.Sanders: 1999; 840 11. Williams DF, Mieler WF, Williams GA. Posterior segment manifestation of ocular trauma. Retina 1990: 10 Suppl 1: S 35-44. 12. Kwok AK, Lai TY, Chan NR. Epiretinal membrane formation with ILM wrinkling after Nd YAG laser membranotomy in valsalva retinopathy Am J Ophthalmol. 2003 October. 136(4) 763766. 13. Gass JDM. Stereoscopic atlas of macular disease: Diagnosis and treatment 3rd edition. Mosby st.Louis 1987. 14. Faulborn, J. Behandlungeinerdiabetischenpramakularen Blutungmitdem Q-switched Neodym: YAG laser. Spektrum Augenheilkd. 1988; 2: 33–35 15. Chau P, Riech JA. Use of the Neodymium – YAG laser to manage sub internal limiting membrane haemorrhage Aust NYJ Ophthalmol 1991; 19: 81-83. 16. Rennie CA, Newman DK. Nd YAG laser treatment for premacular sub hyaloidhaemorrhage. Eye (Lond) 2001; 15: 519-524. 17. O'Hanley, GP and Canny, CLB. Diabetic dense premacular hemorrhage. A possible indication for prompt vitrectomy. Ophthalmology. 1985; 92: 507–511 18. Clearly PE, Kohner EM, Hamilton AM, Bird AC. Retinal macroaneurysms. Br J Ophthalmol 1975; 59: 355–61. 19. Shukla D, Naresh K, Kim R. Optical coherence tomography findings in valsalva retinopathy. Am J Ophthalmol 2005 Jul; 140(1): 1346. 20. Ulbig MW, Mangouritsas G, Rothbacher HH, Hamilton AMP, McHugh JD. Long-term results after drainage of premacularsubhyaloid hemorrhage into the vitreous with a pulsed Nd: YAG laser. Arch Ophthalmol 1998; 116: 1465–1469. J of Evidence Based Med & Hlthcare, pISSN- 2349-2562, eISSN- 2349-2570/ Vol. 2/Issue 28/July 13, 2015 Page 4112 DOI: 10.18410/jebmh/2015/584 ORIGINAL ARTICLE AUTHORS: 1. Shashidhar S. 2. Manasa Penumetcha PARTICULARS OF CONTRIBUTORS: 1. Associate Professor, Department of Ophthalmology, Minto Ophthalmic Hospital & Regional Institute of Ophthalmology. 2. Resident, Department of Ophthalmology, Bangalore Medical College & Research Institute. NAME ADDRESS EMAIL ID OF THE CORRESPONDING AUTHOR: Dr. Shashidhar S, A. V. Road, Opposite Central Police Station, Chamarajpete, Bangalore-560002, Karnataka, India. E-mail: swamyshashidhar@gmail.com Date Date Date Date of of of of Submission: 06/07/2015. Peer Review: 07/07/2015. Acceptance: 11/07/2015. Publishing: 13/07/2015. J of Evidence Based Med & Hlthcare, pISSN- 2349-2562, eISSN- 2349-2570/ Vol. 2/Issue 28/July 13, 2015 Page 4113