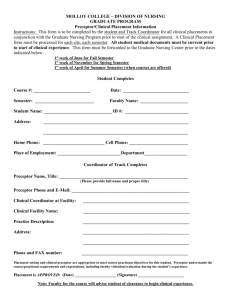
Preceptor - Lock Haven University
advertisement

Preceptorship Manual 2010-2011 Clinical Preceptor Manual *1 INTRODUCTION This manual is a resource and a guide for the second year Physician Assistant students at Lock Haven University of Pennsylvania and for their gracious preceptors. The program’s faculty would like to thank our preceptors for their generous support. Included in this manual are the following: a description of the PA student’s pre-clinical phase training. the role and responsibilities of the preceptor the goals and objectives of each clinical rotations / preceptorships the duties and responsibilities of the student. If you have suggestions regarding this manual, the program, or the clinical preparation of the students, please forward them to the program so they may be incorporated as appropriate. Also, feel free to contact the PA Program Clinical Coordinator at any time either by phone or e-mail: a) E-mail:lbower@lhup.edu b) Office number: 570-484-2199 Last Revised: June, 2011 Clinical Preceptor Manual *2 Table of Contents INTRODUCTION..................................................................................................................................... 2 Section One: PHYSICIAN ASSISTANT PROGRAM PRECEPTOR .................................................... 5 HISTORY .............................................................................................................................................. 6 MISSION............................................................................................................................................... 6 ACCREDITATION ............................................................................................................................... 6 PRE-PROFESSIONAL PROGRAM..................................................................................................... 7 Admission Requirements ........................................................................................................................ 7 PROFESSIONAL PROGRAM ............................................................................................................. 7 PA STUDENT PROFILE ...................................................................................................................... 7 DIDACTIC CURRICULUM ................................................................................................................ 8 YEAR 1: Summer Session ..................................................................................................................... 8 YEAR 1: Fall Semester .......................................................................................................................... 8 YEAR 1: Spring Semester ...................................................................................................................... 9 YEAR 2: Summer Session ..................................................................................................................... 9 YEAR 2: Fall Semester .......................................................................................................................... 9 YEAR 2: Spring Semester ...................................................................................................................... 9 COURSE DESCRIPTIONS .................................................................................................................10 PYAS600—Service Learning Module ..................................................................................................10 PYAS602—Introductory Module ..........................................................................................................10 PYAS604—Women’s Health Module ..................................................................................................10 PYAS606—Urology & Sexually Transmitted Diseases Module ..........................................................11 PYAS608—Human Sexuality Module ..................................................................................................11 PYAS610—Infectious Disease Module ................................................................................................11 PYAS612—Allergy & Immunology Module ........................................................................................11 PYAS614—Hematology Module ..........................................................................................................12 PYAS616—Oncology Module ..............................................................................................................12 PYAS618—Endocrinology Module ......................................................................................................12 PYAS620—Cardiology Module ............................................................................................................12 PYAS622—Pulmonary Module ............................................................................................................13 PYAS624—Nephrology Module ..........................................................................................................13 PYAS626—Psychiatry Module .............................................................................................................13 PYAS628—Ophthalmology Module.....................................................................................................13 PYAS630—Neurology Module ............................................................................................................14 PYAS632—Orthopedics Module ..........................................................................................................14 PYAS634—Rheumatology Module ......................................................................................................14 PYAS636—Dermatology Module.........................................................................................................14 PYAS638—Gastroenterology Module ..................................................................................................15 PYAS640—Obstetrics Module .............................................................................................................15 PYAS642—Otorhinolaryngology Module ............................................................................................15 PYAS644—Pediatrics Module ..............................................................................................................15 PYAS646—Geriatrics Module ..............................................................................................................16 PYAS648—Surgery Module .................................................................................................................16 PYAS650—Emergency Medicine Module ...........................................................................................16 PYAS652—Alternative Medicine Module ............................................................................................16 PYAS654—Occupational Medicine Module ........................................................................................17 PYAS603—Gross (Cadaver) Anatomy .................................................................................................17 PYAS659—Underserved Populations ...................................................................................................17 PYAS601—Medical Decisions .............................................................................................................17 PYAS661 – Evidence Based Medicine I ...............................................................................................17 PYAS662- Evidence Based Medicine II ...............................................................................................18 Clinical Preceptor Manual *3 PYAS 663 – Evidence Based Medicine III ...........................................................................................18 PYAS664 – Clinical Rotations I ...........................................................................................................18 PYAS665 – Clinical Rotations II .........................................................................................................18 PYAS 666 – Clinical Rotations III .......................................................................................................18 A NOTE TO OUR CLINICAL PRECEPTOR .....................................................................................19 PRECEPTORSHIPS ............................................................................................................................20 PROCEDURE FOR ESTABLISHING A LOCK HAVEN UNIVERSITY PHYSICIAN ASSISTANT PRECEPTORSHIP ..............................................................................................................................22 Section Two: POLICIES AND PROCEDURES ..........................................................................................23 POLICIES AND PROCEDURES: STUDENT ....................................................................................24 POLICIES AND PROCEDURES: PRECEPTOR ...............................................................................26 POLICIES AND PROCEDURES: PHYSICIAN ASSISTANT PROGRAM ......................................27 Section Three: GOALS AND OBJECTIVES ..............................................................................................28 PA STUDENT GENERAL CLINICAL GOALS AND OBJECTIVES...............................................30 ROTATION OBJECTIVES GENERAL INTERNAL MEDICINE ...............................................37 ROTATION OBJECTIVES OBSTETRICS AND GYNECOLOGY .............................................44 ROTATION OBJECTIVES GENERAL SURGERY ......................................................................49 ROTATION OBJECTIVES PEDIATRICS ......................................................................................55 ROTATION OBJECTIVES CARDIOLOGY ..................................................................................60 ROTATION OBJECTIVES ENT ......................................................................................................68 ROTATION OBJECTIVES ORTHOPEDICS .................................................................................71 ROTATION OBJECTIVES PSYCHIATRY ....................................................................................76 ROTATION OBJECTIVES EMERGENCY MEDICINE ..............................................................80 ROTATION OBJECTIVES CORRECTIONS MEDICINE ...........................................................84 TOPICS LIST - GERIATRICS..........................................................................................................88 TOPICS LIST - MENTAL HEALTH ...............................................................................................90 TOPICS LIST - OBSTETRICS & GYNECOLOGY .......................................................................91 TOPICS LIST - PEDIATRICS ..........................................................................................................92 Long Term Care Objectives ...............................................................................................................95 Section Four: GENERAL REQUIREMENTS FOR CLINICAL YEAR ...................................................101 Section Five: EVALUATION FORMS......................................................................................................115 STUDENT CRITIQUE FORM ..........................................................................................................116 Section Six: AGREEMENT FORMS .........................................................................................................120 AFFILIATION AGREEMENT ..........................................................................................................121 MEMORANDUM AGREEMENT ....................................................................................................128 PRECEPTORSHIP APPLICATION FORM......................................................................................129 Clinical Preceptor Manual *4 Section One: PHYSICIAN ASSISTANT PROGRAM PRECEPTOR Clinical Preceptor Manual *5 LHUP MASTER OF HEALTH SCIENCE--PHYSICIAN ASSISTANT PROGRAM HISTORY During the summer of 1994 Lock Haven University and its sister universities within the SSHE system were approached regarding the feasibility of starting a program to educate mid-level primary health care providers for medically underserved areas within the state. After initially seeking the support of the local medical community, the University developed an advisory committee to look into such an undertaking. This committee overwhelmingly felt that the existing resources of Lock Haven University could be augmented to provide both the prerequisite requirements and the graduate curriculum required to provide a high quality Master’s level program to educate and place Physician Assistants in rural communities. The support of the medical community has been overwhelming. In June, 1996 the Physician Assistant Program enrolled its first class of 24 students and became the first state-supported Physician Assistant program within the Commonwealth. Since its inception the PA Program has received National Recognition ranking 34th, out of the over 140 PA Programs nationally, in US News and World Report. The program has been successful in fulfilling its mission with over 60% of graduates remaining in Pennsylvania, and over 45% acquiring positions in primary care specialties. The program has expanded to four campus locations including Harrisburg, Clearfield, Coudersport, and main campus in Lock Haven PA enrolling 72 new students each year. MISSION The mission of the program is to educate and train highly-skilled physician assistants who: are capable of providing quality health care, have expertise in the health care needs of the medically underserved, are prepared to critically evaluate, and become leaders in bringing about improvement in, the medical and social systems that affect the health of underserved populations, will seek and retain employment as primary care physician assistants in medically underserved areas of the Commonwealth of Pennsylvania. ACCREDITATION The Lock Haven University Physician Assistant Program is fully accredited in accordance with the standards set forth by the Accreditation Review Committee for the Physician Assistant. The Physician Assistant Program resides within the Department of Physician Assistant Studies. Clinical Preceptor Manual *6 PRE-PROFESSIONAL PROGRAM Pre-professional requirements are designed to provide the student with a firm foundation in the basic sciences. The following are prerequisite courses for matriculation into the physician assistant program: Admission Requirements Baccalaureate degree from a regionally accredited institution with the following course requirements: Chemistry I & II Biology/Zoology (6 semester hours) Human Anatomy Human Physiology Microbiology Genetics Statistics Further requirements include: Computer literacy – demonstrated through course work or experience GRE scores – students must have completed the Graduate Record Examination. PROFESSIONAL PROGRAM The professional phase consists of a rigorous 24-month combination of didactic and clinical work. The first 12 months are devoted to the didactic (classroom) phase as outlined on the following pages. The second year is divided into five six-week clinical rotations in the disciplines of internal medicine, pediatrics, either obstetrics and gynecology or emergency medicine, surgery, and an elective of the student’s choice. Following these five rotations is a single eighteen-week or two nine-week clinical preceptorships in a primary care setting. The program’s masters level design is commensurate with current trends within the PA education. As part of that masters level design, students will be required to complete coursework in research design and complete an Evidence Based Medicine Project. PA STUDENT PROFILE 107 Currently enrolled Average age is 23 Undergrad GPA is 3.46 Clinical Preceptor Manual *7 DIDACTIC CURRICULUM YEAR 1: Summer Session Gross (Cadaver) Anatomy 4.0 sh Service Learning Module 1.0 sh Introductory Module 5.0 sh Women’s Health Module 1.5 sh Urology & Sexually Transmitted Diseases Module 0.5 sh Human Sexuality Module 0.5 sh Infectious Disease Module 2.0 sh Total 14.5 sh YEAR 1: Fall Semester Allergy & Immunology Module 1.0 sh Hematology Module 1.0 sh Dermatology Module 1.0 sh Endocrinology Module 1.5 sh Cardiology Module 3.0 sh Pulmonary Module 2.0 sh Nephrology Module 1.5 sh Ophthalmology Module 1.0 sh Neurology Module 2.0 sh Psychiatry Module 2.0 sh Underserved Populations 3.0 sh Total Clinical Preceptor Manual 19 sh *8 YEAR 1: Spring Semester Orthopedics Module 1.0 sh Rheumatology Module Oncology Module 1.5 sh Gastroenterology Module 1.5 sh Obstetrics Module 1.5 sh Otorhinolaryngology Module 1.0 sh Pediatrics Module 2.0 sh Geriatrics Module 1.0 sh Surgery Module 1.5 sh Emergency Medicine Module 1.5 sh Alternative Medicine Module 0.5 sh Occupational Medicine Module 1.0 sh Medical Decisions 3.0 sh Total First Year Total 18 sh 51.5 sh YEAR 2: Summer Session Clinical Rotations 1EBM 1Total 11.0 sh 1.0 sh 12.0 sh YEAR 2: Fall Semester Clinical Rotations 2EBM 2Total 17.0 sh 1.0 sh 18.0 sh YEAR 2: Spring Semester Clinical Rotations 3EBM 3Total 17.0 sh 1.0 sh 18.0 sh Second Year Total 48 sh Grand Total of Years 1 & 2 Clinical Preceptor Manual 99.5 sh *9 COURSE DESCRIPTIONS PYAS600—Service Learning Module Description: This module is one of the series of modules that comprises the didactic curriculum of the program. It prepares the student to participate in program service learning projects that focus on the health care needs of rural communities. Content areas in this module include: introduction to community health and preventive medicine, community health needs assessment, community screening and health promotion/disease prevention programs, diagnostic procedures used in health screening programs, and alternative therapies. Each student will participate in designing, implementing, and assessing community-based service learning projects in designated communities within proximity to the university. PYAS602—Introductory Module Description: This module is one of the series of modules that comprises the didactic curriculum of the program. It introduces the student to fundamental concepts essential to understanding subsequent components of the curriculum. Content areas in this module include: fundamentals of medical research and reasoning, an overview of pathophysiology, introductory patient assessment including the medical history and physical examination, pharmacokinetics and pharmacodynamics, health promotion and disease prevention, medical records, and rural and professional issues. PYAS604—Women’s Health Module Description: This module is one of the series of modules that comprises the didactic curriculum of the program. It provides a disease oriented and problemoriented approach to understanding the etiology, pathophysiology, manifestations, diagnosis and treatment of specific diseases encountered in gynecology and women’s health. Content areas in this module include: medical research and reasoning, anatomy, pathophysiology, patient assessment, diagnostic procedures, therapeutics, patient education, service learning, medical record keeping, and rural and professional issues. Clinical Preceptor Manual *10 PYAS606—Urology & Sexually Transmitted Diseases Module Description: This module is one of the series of modules that comprises the didactic curriculum of the program. It provides both a disease oriented and problemoriented approach to understanding the etiology, pathophysiology, manifestations, diagnosis and treatment of specific diseases encountered in urology, including sexually transmitted diseases. Content areas in this module include: medical research and reasoning, anatomy, pathophysiology, patient assessment, diagnostic procedures, therapeutics, patient education, service learning, medical record keeping, and rural and professional issues. PYAS608—Human Sexuality Module Description: This module is one of the series of modules that comprises the didactic curriculum of the program. Personal attitudes toward sexual issues are explored in order to prepare the student to discuss issues of sexuality with patients. Other topics include human sexual response, sexual diversity, and the diagnosis and treatment of disorders of human sexual response. PYAS610—Infectious Disease Module Description: This module is one of the series of modules that comprises the didactic curriculum of the program. It provides both a disease oriented and problemoriented approach to understanding the etiology, pathophysiology, manifestations, diagnosis and treatment of specific diseases encountered in infectious diseases. Content areas in this module include: medical research and reasoning, medical microbiology, pathophysiology, patient assessment, diagnostic procedures, therapeutics, patient education, service learning, medical record keeping, and rural and professional issues. PYAS612—Allergy & Immunology Module Description: This module is one of the series of modules that comprises the didactic curriculum of the program. It provides both a disease oriented and problemoriented approach to understanding the etiology, pathophysiology, manifestations, diagnosis and treatment of specific diseases encountered in allergy and immunology. Content areas in this module include: medical research and reasoning, anatomy, pathophysiology, patient assessment, diagnostic procedures, therapeutics, patient education, service learning, medical record keeping, and rural and professional issues. Clinical Preceptor Manual *11 PYAS614—Hematology Module Description: This module is one of the series of modules that comprises the didactic curriculum of the program. It provides both a disease oriented and problemoriented approach to understanding the etiology, pathophysiology, manifestations, diagnosis and treatment of specific diseases encountered in hematology. Content areas in this module include: medical research and reasoning, anatomy, pathophysiology, patient assessment, diagnostic procedures, therapeutics, patient education, service learning, medical record keeping, and rural and professional issues. PYAS616—Oncology Module Description: This module is one of the series of modules that comprises the didactic curriculum of the program. It provides a disease oriented and problemoriented approach to understanding the etiology, pathophysiology, manifestations, diagnosis and treatment of specific diseases encountered in oncology. Content areas in this module include: medical research and reasoning, anatomy, pathophysiology, patient assessment, diagnostic procedures, therapeutics, patient education, service learning, medical record keeping, and rural and professional issues. PYAS618—Endocrinology Module Description: This module is one of the series of modules that comprises the didactic curriculum of the program. It provides a disease oriented and problemoriented approach to understanding the etiology, pathophysiology, manifestations, diagnosis and treatment of specific diseases encountered in endocrinology. Content areas in this module include: medical research and reasoning, anatomy, pathophysiology, patient assessment, diagnostic procedures, therapeutics, patient education, service learning, medical record keeping, and rural and professional issues. PYAS620—Cardiology Module Description: This module is one of the series of modules that comprises the didactic curriculum of the program. It provides a disease oriented and problemoriented approach for understanding the etiology, pathophysiology, manifestations, diagnosis and treatment of specific diseases encountered in cardiology. Content areas in this module include: medical research and reasoning, anatomy, pathophysiology, patient assessment, diagnostic procedures, therapeutics, patient education, service learning, medical record keeping, and rural and professional issues. Clinical Preceptor Manual *12 PYAS622—Pulmonary Module Description: This module is one of the series of modules that comprises the didactic curriculum of the program. It provides a disease oriented and problemoriented approach to understanding the etiology, pathophysiology, manifestations, diagnosis and treatment of specific diseases encountered in pulmonary medicine. Content areas in this module include: medical research and reasoning, anatomy, pathophysiology, patient assessment, diagnostic procedures, therapeutics, patient education, service learning, medical record keeping, and rural and professional issues. PYAS624—Nephrology Module Description: This module is one of the series of modules that comprises the didactic curriculum of the program. It provides a disease oriented and problemoriented approach to understanding the etiology, pathophysiology, manifestations, diagnosis and treatment of specific diseases encountered in nephrology. Content areas in this module include: medical research and reasoning, anatomy, pathophysiology, patient assessment, diagnostic procedures, therapeutics, patient education, service learning, medical record keeping, and rural and professional issues. PYAS626—Psychiatry Module Description: This module is one of the series of modules that comprises the didactic curriculum of the program. It provides a disease oriented and problemoriented approach to understanding the etiology, pathophysiology, manifestations, diagnosis and treatment of specific diseases encountered in psychiatry. Content areas in this module include: medical research and reasoning, anatomy, pathophysiology, patient assessment, diagnostic procedures, therapeutics, patient education, service learning, medical record keeping, and rural and professional issues. PYAS628—Ophthalmology Module Description: This module is one of the series of modules that comprises the didactic curriculum of the program. It provides a disease oriented and problemoriented approach to understanding the etiology, pathophysiology, manifestations, diagnosis and treatment of specific diseases encountered in ophthalmology. Content areas in this module include: medical research and reasoning, anatomy, pathophysiology, patient assessment, diagnostic procedures, therapeutics, patient education, service learning, medical record keeping, and rural and professional issues. Clinical Preceptor Manual *13 PYAS630—Neurology Module Description: This module is one of the series of modules that comprises the didactic curriculum of the program. It provides a disease oriented and problemoriented approach to understanding the etiology, pathophysiology, manifestations, diagnosis and treatment of specific diseases encountered in neurology. Content areas in this module include: medical research and reasoning, anatomy, pathophysiology, patient assessment, diagnostic procedures, therapeutics, patient education, service learning, medical record keeping, and rural and professional issues. PYAS632—Orthopedics Module Description: This module is one of the series of modules that comprises the didactic curriculum of the program. It provides a disease oriented and problemoriented approach to understanding the etiology, pathophysiology, manifestations, diagnosis and treatment of specific diseases encountered in orthopedics. Content areas in this module include: medical research and reasoning, anatomy, pathophysiology, patient assessment, diagnostic procedures, therapeutics, patient education, service learning, medical record keeping, and rural and professional issues. PYAS634—Rheumatology Module Description: This module is one of the series of modules that comprises the didactic curriculum of the program. It provides a disease oriented and problemoriented approach to understanding the etiology, pathophysiology, manifestations, diagnosis and treatment of specific diseases encountered in rheumatology. Content areas in this module include: medical research and reasoning, anatomy, pathophysiology, patient assessment, diagnostic procedures, therapeutics, patient education, service learning, medical record keeping, and rural and professional issues. PYAS636—Dermatology Module Description: This module is one of the series of modules that comprises the didactic curriculum of the program. It provides a disease oriented and problemoriented approach to understanding the etiology, pathophysiology, manifestations, diagnosis and treatment of specific diseases encountered in dermatology. Content areas in this module include: medical research and reasoning, anatomy, pathophysiology, patient assessment, diagnostic procedures, therapeutics, patient education, service learning, medical record keeping, and rural and professional issues. Clinical Preceptor Manual *14 PYAS638—Gastroenterology Module Description: This module is one of the series of modules that comprises the didactic curriculum of the program. It provides a disease oriented and problemoriented approach to understanding the etiology, pathophysiology, manifestations, diagnosis and treatment of specific diseases encountered in gastroenterology. Content areas in this module include: medical research and reasoning, anatomy, pathophysiology, patient assessment, diagnostic procedures, therapeutics, patient education, service learning, medical record keeping, and rural and professional issues. PYAS640—Obstetrics Module Description: This module is one of the series of modules that comprises the didactic curriculum of the program. It provides a disease oriented and problemoriented approach to understanding the etiology, pathophysiology, manifestations, diagnosis and treatment of specific diseases encountered in obstetrics. Content areas in this module include: medical research and reasoning, anatomy, pathophysiology, patient assessment, diagnostic procedures, therapeutics, patient education, service learning, medical record keeping, and rural and professional issues. PYAS642—Otorhinolaryngology Module Description: This module is one of the series of modules that comprises the didactic curriculum of the program. It provides a disease oriented and problemoriented approach to understanding the etiology, pathophysiology, manifestations, diagnosis and treatment of specific diseases encountered in otorhinolaryngology. Content areas in this module include: medical research and reasoning, anatomy, pathophysiology, patient assessment, diagnostic procedures, therapeutics, patient education, service learning, medical record keeping, and rural and professional issues. PYAS644—Pediatrics Module Description: This module is one of the series of modules that comprises the didactic curriculum of the program. It provides a disease oriented and problemoriented approach to understanding the etiology, pathophysiology, manifestations, diagnosis and treatment of specific diseases encountered in pediatrics. Content areas in this module include: medical research and reasoning, anatomy, pathophysiology, patient assessment, diagnostic procedures, therapeutics, patient education, service learning, medical record keeping, and rural and professional issues. Clinical Preceptor Manual *15 PYAS646—Geriatrics Module Description: This module is one of the series of modules that comprises the didactic curriculum of the program. It provides a disease oriented and problemoriented approach to understanding the etiology, pathophysiology, manifestations, diagnosis and treatment of specific diseases encountered in geriatrics. Content areas in this module include: medical research and reasoning, anatomy, pathophysiology, patient assessment, diagnostic procedures, therapeutics, patient education, service learning, medical record keeping, and rural and professional issues. PYAS648—Surgery Module Description: This module is one of the series of modules that comprises the didactic curriculum of the program. It provides a disease oriented and problemoriented approach to understanding the etiology, pathophysiology, manifestations, diagnosis and treatment of specific diseases encountered in surgery. Content areas in this module include: medical research and reasoning, anatomy, pathophysiology, patient assessment, diagnostic procedures, therapeutics, patient education, service learning, medical record keeping, and rural and professional issues. PYAS650—Emergency Medicine Module Description: This module is one of the series of modules that comprises the didactic curriculum of the program. It provides a disease oriented and problemoriented approach to understanding the etiology, pathophysiology, manifestations, diagnosis and treatment of specific diseases encountered in emergency medicine. Content areas in this module include: medical research and reasoning, anatomy, pathophysiology, patient assessment, diagnostic procedures, therapeutics, patient education, service learning, medical record keeping, and rural and professional issues. PYAS652—Alternative Medicine Module Description: This module is one of the series of modules that comprises the didactic curriculum of the program. This module provides the student with an orientation to alternative methods of health care, including such fields as acupuncture, chiropractic, massage, naturopathy, and culturally based therapies. Content areas in this module include: medical research and reasoning, anatomy, pathophysiology, patient assessment, diagnostic procedures, therapeutics, patient education, service learning, medical record keeping, and rural and professional issues. Clinical Preceptor Manual *16 PYAS654—Occupational Medicine Module Description: This module is one of the series of modules that comprises the didactic curriculum of the program. It provides a disease oriented and problemoriented approach to understanding the etiology, pathophysiology, manifestations, diagnosis and treatment of specific diseases encountered in occupational medicine, with special emphasis on those occupations that predominate in rural areas. Content areas in this module include: medical research and reasoning, epidemiology, anatomy, pathophysiology, patient assessment, diagnostic procedures, therapeutics, patient education and prevention, service learning, medical record keeping, and rural and professional issues. PYAS603—Gross (Cadaver) Anatomy Description: Gross anatomy is studied regionally stressing relationships of major structures, organs, vessels and nerves. Human cadaver observation and dissection by students are included in the laboratory sessions. All major areas of the body are covered. References to the relationship of anatomical structures to pathology, traumatic injury and medicine are stressed. PYAS659—Underserved Populations Description: An exploration of factors, especially historical, racial, ethnic, socioeconomic, and geographic, determined to create disparities in healthcare access, delivery, and policy. The course will specifically encompass/consider barriers known to affect these disparities in rural and urban regions as well as various healthcare settings including correctional facilities. PYAS601—Medical Decisions Description: An exploration of the many influences in medical decisions made by providers, patients, communities and governments. Institutional and psychological constraints will be considered when looking at legal, ethical, moral and personal medical decisions. Medical decisions will also be viewed through various multicultural prisms. Throughout the course, we will examine the balance of pragmatism and compassion in the quickly changing medical arena. PYAS661 – Evidence Based Medicine I Description: The first of three complimentary courses that will develop skills in Evidence Based Medicine (EBM). Students will build upon skills acquired during the first year of the program and apply EBM skills to authentic patient cases. Students will explore the limitations and the ethical Clinical Preceptor Manual *17 implications of evidence based practice. The overall goal of this course will be to extrapolate (EBM) use into their future practice as clinicians. PYAS662- Evidence Based Medicine II Description: The second of three complimentary courses that will develop skills in Evidence Based Medicine (EBM). Students will build upon skills acquired during the first year of the program and EBM I. Students will apply EBM skills to authentic patient cases. Students will explore the limitations and ethical implications of Evidence Based Practice. The overall goal of this course will then be to extrapolate evidenced based medicine use into their future practice as clinicians. PYAS 663 – Evidence Based Medicine III Description: The third of three complimentary courses that will build upon skills acquired during EBM I & II. Students will further develop skills using the concepts of variability, validity, sensitivity, specificity and probability of testing. Students will apply EBM to their daily clinical practice. This course culminates in the written and oral presentation of the EBM capstone project. PYAS664 – Clinical Rotations I Description: The first in a series of three rotations, 12 weeks in duration, designed to allow students to develop the knowledge, skills, abilities and attitudes required to care for patients of all age groups seen in primary care. Students will be assigned to a minimum of two clinical rotation sites in any of the following disciplines; surgery, internal medicine, pediatrics, OB/GYN, emergency medicine, or any subspecialty discipline that will develop skills required for generalist/primary care practice. PYAS665 – Clinical Rotations II Description; An eighteen-week clinical experience, the second in a series of three courses, that allows students to develop the knowledge, skills, abilities and attitudes required to care for patients of all age groups seen in primary care. Students will be assigned to a minimum of three clinical rotation sites in any of the following disciplines; surgery, internal medicine, pediatrics, OB/GYN, emergency medicine, or any subspecialty discipline that will develop skills required for generalist/primary care practice. PYAS 666 – Clinical Rotations III An eighteen-week clinical experience, the third in a series of three courses, that allows students to develop the knowledge, skills, abilities and attitudes required to care for patients of all age groups seen in primary care. Students will develop an understanding of the health promotion, disease prevention needs of communities and refine skills that develop problemfocused and disease-oriented approach diseases commonly seen in the primary care setting. Clinical Preceptor Manual *18 A NOTE TO OUR CLINICAL PRECEPTOR Inherent in the role of the primary care provider is that of a teacher. You teach your patients, your staff, your colleagues, and perhaps the community at large. Teaching provides the opportunity to stay current by responding to the inquiries of bright young students. "To Teach is to Learn Twice”; the first time for your own benefit the second for the benefit of the student you mentor. The preceptor provides a central role in the clinical education of Physician Assistants. Since the emphasis of the PA's role is teamwork with his or her supervising physician, development of these characteristics starts here. Students look to the preceptor for answers to clinical questions and guidance in patient management problems. Specific guidelines for the clinical experience are outlined in the clinical education objectives section of this manual. The preceptor should provide the student an opportunity to accomplish those objectives that are applicable to their practice setting, and facilitate and encourage the student to find ways to accomplish the remaining objectives through other sources. The preceptor evaluates the clinical acumen, knowledge, skills and abilities of the student and documents it in the Clinical Evaluation Form included in this manual. Early conferencing with the student will assure that an open line of communication exists, expectations are not disparate, and that the student and the preceptor both have an enjoyable experience. This opportunity is facilitated by the rotations first written assignment due from every student to the program: “Individual Goal Assessment”. This assessment allows you the preceptor to sit down with the student and review your goals and expectations for the rotation. We thank you for your time in doing this with the student. The program further looks to the clinical preceptor for other areas of expertise. They play an important role in improving curriculum, clinical objectives, and other requirements of the clinical experience. Additional guidelines are provided in Section II, Policies and Procedures in this manual. Clinical Preceptor Manual *19 PRECEPTORSHIPS OBJECTIVES: The overall goal of clinical rotations and preceptorships is to provide both breadth and depth of experience in primary care, under the physician’s supervision, in clinical practice settings, with a significant portion of clinical experience taking place in rural areas. Specific goals and objectives are listed in Section III of this manual. LENGTH: The second year of the program consists of five, six-week rotations and two nine-week rotations (or one 18 week rotation) called preceptorships. The 6-week rotations are in pediatrics, internal medicine, surgery, emergency medicine or obstetrics, gynecology and an elective. The preceptorship rotations are recommended to be in rural primary care. PRECEPTORS: Preceptors are Physicians or Physician Assistants throughout the United States with the majority coming from primary care specialties and subspecialties. Preceptors are responsible for the organization and administration of local resources, including the provision of patients. The preceptors and their colleagues act as instructors and supervisors of the student while in the clinical environment. CLINICAL FACILITIES: The clinical facilities used in the instruction of students during rotations and preceptorships are those in which the physician preceptors have privileges. Most preceptors offer exposure not only in the clinic and the hospital but also, to a limited degree, in nursing homes and other clinical facilities in the community. The preceptor acts as a liaison with the health care facility administration and the Lock Haven University Physician Assistant Program. SUPERVISON AND EVALUATION: Students will return to campus at the completion of each rotation for comprehensive testing, clinical skills evaluation, patient management seminars, and lectures on professional and medical topics. Prior to the preceptorship experience, new preceptors will be oriented to their role as a preceptor. A report of the student’s academic performance, didactic and clinical strengths and weaknesses, and a personal profile will be provided to each preceptor prior to the beginning of each clinical assignment. This will help to individualize instruction. During the clinical assignment the preceptor will become more familiar with each student’s strengths, and can provide individualized teaching, supervision, and clinical experience accordingly. Clinical Preceptor Manual *20 The preceptor must complete an evaluation of the student. To this end, a “Clinical Evaluation Form” appears in Section V of this manual. The preceptor’s evaluation will form a portion of the student’s grade. Students are asked to evaluate their clinical experiences to assist the preceptor and program in evaluating the preceptorship experience. A “Student Critique Form” can be found in Section V. Preceptors will periodically be asked to evaluate the overall program and its success in providing well-trained Physician Assistants geared toward service in primary care. APPOINTMENT: Participating Physicians and Physician Assistants will receive an appointment as a Preceptor in the Physician Assistant Program. This appointment, without compensation, is granted in official recognition of your involvement in the education and professional development of students. Preceptors are provided with guest e-mail accounts to facilitate ongoing communication. This, along with electronic access to the University’s Expanded Academic Index and the Internet, will provide current medical resources for the preceptor and student in remote locations. Preceptors are also entitled to utilize the University’s facilities to help in their own personal and professional development. HOUSING: Many preceptors are able to provide or arrange for housing at their site. Accommodations range from a room in the community hospital, to a spare room in someone’s home, to an apartment or room that is leased for the period involved. Since the cost of the preceptor year is very burdensome for many students, any arrangements made for housing and/or meals are very much appreciated. Being unable to provide for housing does not eliminate you from consideration as a preceptor. LIABILITY: The student is required to maintain liability coverage throughout the two years of the program. Arrangements have been made through Chicago Insurance Company, a contracted carrier for medical malpractice insurance through the American Academy of Physician Assistants, to provide low cost coverage for physician assistant students. Limits of liability will be furnished upon request. AGREEMENTS: Agreements will be completed prior to commencement of the clinical rotation. Memorandum agreements will be completed by the supervising preceptor (M.D., PA, NP, etc.) and affiliation agreements will be completed as necessary. Clinical Preceptor Manual *21 PROCEDURE FOR ESTABLISHING A LOCK HAVEN UNIVERSITY PHYSICIAN ASSISTANT PRECEPTORSHIP The physician or PA interested in serving as a preceptor to a PA student completes the application form contained in Section VI of this manual and returns it along with a current curriculum vitae to the Department of Physician Assistant Studies. 1. The Clinical Coordinator and Program or Medical Director review this data and mail a Memorandum Agreement to prospective preceptors. A Memorandum Agreement is included in Section VI. 2. In the interim, the Clinical Coordinator generally corresponds with, or schedules a preceptorship site visit to meet with the prospective preceptor and answer any additional questions. 3. Each site will be evaluated as to its appropriateness for student rotations prior to, or at the signing of the Memorandum Agreement. 4. The prospective preceptor signs the Memorandum Agreement, or similar agreement, and returns it to the program for final approval of either the Program Director or Medical Director. 5. The Clinical Coordinator adds the physician’s name to the list of preceptors and assigns students depending on the availability of the preceptor and the needs of the program and students. 6. Current licensure information is verified by the PA Program administrative staff 7. Contact is made with, and appropriate agreements established, ancillary sites where the PA student may be working with the preceptor. Clinical Preceptor Manual *22 Section Two: POLICIES AND PROCEDURES Clinical Preceptor Manual *23 POLICIES AND PROCEDURES: STUDENT The physician assistant student will be required to adhere to the regulations and policies as set forth in the Lock Haven University Handbook as well as the Physician Assistant Student Handbook. In addition the student will: 1. Be responsible to the preceptor for reporting at the assigned times, on call responsibilities of the site, and satisfactory performance on each learning rotation. The student will also be responsible for any other stipulations set forth by the preceptor. 2. Request permission for absences from clinical sites from the preceptor. Program authorization is required for any absence exceeding one day. Failure to notify the Clinical Coordinator of absences greater than one day will result in grade reduction. 3. Wear an identification tag that identifies the student by first and last names as well as the words "Physician Assistant Student" in 16 point lettering while carrying out any responsibilities entailed in his/her clinical training. 4. Comply with preceptorship dress requirements and/or those found in the Physician Assistant Student Handbook. 5. Sign all notes documented in patient records with "PA Student" or PA-S following their name. All entries shall be legible. 6. Conduct him/herself in a professional manner at all times. Students should consider themselves as ambassadors of Lock Haven University, the Department of Physician Assistant and Graduate Studies in Education and the physician assistant profession. This includes behavior toward patients, faculty, peers, and other members of the community. Ethical behavior should adhere to the code of ethics set forth by the American Academy of Physician Assistants. Students shall also be required to abide by all applicable state laws pertaining to physician assistant practice. 7. Write prescriptions only when directed by the supervising preceptor to do so. The preceptor must sign all such prescriptions. 8. Respect patient confidentiality at all times. Exclude all identifying information when discussing cases in and outside the clinical setting. Remove all identifying information from assignments forwarded to the PA Program. Clinical Preceptor Manual *24 9. Confer immediately with the preceptor and the program if he or she becomes aware of any potential medical liability incident regarding his or her activities. 10. Be certain that all personal and financial obligations with individuals or institutions are satisfied prior to leaving. 11. Be responsible to his or her preceptor, follow the rules and regulations of the hospital or other institutions in which he or she works. 12. Successfully complete the requirements of the rotation/preceptorship as outlined in this manual including timely submission of journals and patient logs. 13. Notify the precepting physician and the program director immediately of any sharps, injuries or other biohazard contamination. 14. If upon receipt of grades from the preceptor, should the student feel that the grades assigned were inconsistent with their perceived level of competency, the student shall notify his/her faculty supervisor. Under no circumstances will a student directly contact the preceptor to argue his/her point for a higher grade. Failure to comply with this policy will result in disciplinary action being taken. 15. Dismissal from a clinical rotation site due to behavioral or other reasons of professional misconduct will result in failure of the course that the student is enrolled in. 16. Any absence from the clinical year of greater than 30 days will require the student to undergo testing, both written and practical, prior to resuming clinical training. Failure to comply with the above policies and procedures may jeopardize the student’s standing in the program. Non compliance will result initially in grade reduction, including the possibility of course failure, and may ultimately result in dismissal from the program. Clinical Preceptor Manual *25 POLICIES AND PROCEDURES: PRECEPTOR The policies and procedures listed below are intended to assist in the overall administrative process of the clinical preceptorship experience. The preceptor: * Holds an appointment as “Clinical Faculty” within the Physician Assistant Program, within the Department of Physician Assistant and Graduate Studies in Education, College of Health and Human Services. This appointment is effective with the date of appointment and continues until the appointment is terminated. The preceptor will: * Be the individual at the clinical site who is designated to provide supervision and related assessments of the student’s progress in achieving program requirements. * Be responsible for the organization and administration of local resources to meet the goals and objectives of the Physician Assistant Program. This includes: * The provision of patients (both ambulatory and in the hospital) and associate preceptors to share and assist in the teaching program, and other resources available in the community that might strengthen the clinical educational experiences for the student. * Assigning students to various learning situations during the clinical experience. * Assist with arrangements for housing when possible. * Complete and return to the program a Clinical Evaluation Form for each student’s performance. * Countersign the student’s notes and work-ups on the patient's records within a reasonable time and consistent with the guidelines of the institution. * Countersign all prescriptions and/or orders originated by the student. * In the event of any potential medical liability in which the student may be involved, confer immediately with the Physician Assistant Program. * Participate in program accreditation reviews as able. * Participate in program educational conferences and/or programs to enhance clinical educational experiences. * Directly supervise all student activities related to diagnostic/therapeutic care Clinical Preceptor Manual *26 POLICIES AND PROCEDURES: PHYSICIAN ASSISTANT PROGRAM The Clinical Coordinator of the Physician Assistant Program is responsible to the Director of the Physician Assistant Program, and the Chair of the Department of Physician Assistant and Graduate Studies in Education and the Dean of the College of Education and Human Services. The policies set forth by the program and the university will be followed. In addition, the Physician Assistant Program will: * Maintain all department and academic files on each student. * Be responsible for the assignment of students to preceptors. * Be responsible for maintaining open lines of communication with students who are on preceptorships. * Provide academic information about the student to the preceptor and/or cooperating medical facility, including a biographical sketch, prior to the beginning of each preceptorship. * Be responsible to excuse student absences of more than one day from the preceptor sites and, after consultation with the preceptor, determine remedial action and progress criteria for each student. * Communicate with the preceptor at appropriate intervals regarding student progress, as well as present status of the preceptorship site. * Along with the faculty supervisor, will determine final grades for students in their clinical course. * Accept feedback from preceptors on ways to improve student preparation during the didactic and clinical phases of training. * Provide feedback to preceptors from the Student Critique Form and other information gathered in the clinical year. * Provide assistance and instruction to the preceptor regarding methods and techniques for facilitating clinical instruction. * Assure students receive training in areas that are mandated for all healthcare workers including HIPPA, Universal Precautions and other areas that assure patient safety and confidentiality. Clinical Preceptor Manual *27 Section Three: GOALS AND OBJECTIVES Clinical Preceptor Manual *28 PHYSICIAN ASSISTANT PROGRAM—Competencies Consistent with the mission of the LHU PA Program to prepare highly skilled physician assistants with expertise related to medically underserved regions of the Commonwealth the program has adopted the Competencies for the Physician Assistant Profession as promulgated by the major professional organizations. Each student will demonstrate minimal competency n each of the following areas: MEDICAL KNOWLEDGE Medical knowledge includes an understanding of pathophysiology, patient presentation, differential diagnosis, patient management, surgical principles, health promotion and disease prevention. Physician assistants must demonstrate core knowledge about established and evolving biomedical and clinical sciences and the application of this knowledge to patient care in their area of practice. In addition, physician assistants are expected to demonstrate an investigatory and analytic thinking approach to clinical situations. Physician assistants are expected to: 1. understand etiologies, risk factors, underlying pathologic process, and epidemiology for medical conditions 2. identify signs and symptoms of medical conditions 3. select and interpret appropriate diagnostic or lab studies 4. manage general medical and surgical conditions to include understanding the indications, contraindications, side effects, interactions and adverse reactions of pharmacologic agents and other relevant treatment modalities 5. identify the appropriate site of care for presenting conditions, including identifying emergent cases and those requiring referral or admission 6. identify appropriate interventions for prevention of conditions 7. identify the appropriate methods to detect conditions in an asymptomatic individual 8. differentiate between the normal and the abnormal in anatomic, physiological, laboratory findings and other diagnostic data 9. appropriately use history and physical findings and diagnostic studies to formulate a differential diagnosis 10. provide appropriate care to patients with chronic conditions INTERPERSONAL & COMMUNICATION SKILLS Interpersonal and communication skills encompass verbal, nonverbal and written exchange of information. Physician assistants must demonstrate interpersonal and communication skills that result in effective information exchange with patients, their patients’ families, physicians, professional associates, and the health care system. Physician assistants are expected to: 1. create and sustain a therapeutic and ethically sound relationship with patients 2. use effective listening, nonverbal, explanatory, questioning, and writing skills to elicit and provide information 3. appropriately adapt communication style and messages to the context of the individual patient interaction 4. work effectively with physicians and other health care professionals as a member or leader of a health care team or other professional group 5. apply an understanding of human behavior Clinical Preceptor Manual *29 6. • demonstrate emotional resilience and stability, adaptability, flexibility and tolerance of ambiguity and anxiety 7. • accurately and adequately document and record information regarding the care process for medical, legal, quality and financial purposes PA STUDENT GENERAL CLINICAL GOALS AND OBJECTIVES While emphasizing the health care needs of medically underserved populations, the following general objectives will be achieved: 1. HISTORY: Elicit an appropriate complete, interval or acute history from patients of any age and either sex in any setting. A. Obtain a clear, concise chief complaint and history of the present illness. B. Obtain a complete past medical history including illnesses, hospitalizations, surgeries, trauma, and childhood illnesses. C. Obtain a history of allergies, transfusion reactions, and reactions to medications. D. Obtain a pertinent social history including occupation, current life situation, nutrition, uses of tobacco, alcohol and other drugs. E. Obtain a list of current medications along with details as to use, dose and schedules, including the use of over-the-counter medications. F. Obtain a family history pertaining to exposure to illness, familial predisposition to disease, or genetic transmission. G. Obtain a pertinent review of body systems. H. Obtain an interval history pertaining to progression, regression or stability of chronic illness. I. Obtain a brief outpatient history pertaining to an acute illness. J. Record all pertinent historical data on the defined database in a clear, concise and relevant manner. 2. PHYSICAL EXAMINATION: Perform, as appropriate, a complete or partial physical examination of a patient of any age, sex or condition in any setting. A. Demonstrate ability to gain the patient’s confidence and provide reassurance about the examination. B. Demonstrate appropriate use of the instruments for the physical examination. C. Perform a complete, logical and sequential physical examination. While emphasizing the health care needs of underserved populations, the following general objectives will be achieved: A. Demonstrate the ability to alter the sequence and content of the examination according to the special need of the individual patient. B. Perform an appropriate limited examination pertaining to progression, regression or stability of chronic illness. C. Perform an appropriate physical examination on an acute illness. D. Recognize the physical examination findings that are normal and Clinical Preceptor Manual *30 E. abnormal for the patient’s age and gender. Record all normal and abnormal findings on the defined database. Clinical Preceptor Manual *31 3. DIAGNOSTIC STUDIES: Identify, perform, order and/or interpret appropriate, cost-effective, routine diagnostic procedures, based on history and physical examination findings, and be able to assist the physician with other diagnostic procedures as directed. A. Identify the appropriate and available diagnostic tests for a particular problem based on the history and physical examination findings. B. Identify and discuss indications and contraindications of the various diagnostic tests. C. Identify and describe the risks, costs and patient inconvenience of various diagnostic tests. D. Demonstrate skills required to collect routine specimens. 1. bacteriologic samples 2. bloods, venous and arterial 3. gastric contents 4. sputum 5. stool 6. tissues 7. urine E. Demonstrate skills necessary to perform and/or interpret basic laboratory tests. 1. CBC 2. gram stain 3. stool, O&P 4. stool, guaiac 5. urinalysis, dipstick 6. wet prep/KOH 7. pregnancy test 8. alcohol screening F. Demonstrate skills necessary to perform and interpret a 12 lead EKG and rhythm strip. G. Administer, interpret and record results of intradermal skin test. H. Demonstrate skills necessary to perform and interpret screening tonometry and audiometry tests. I. Identify, order and/or perform and/or interpret other selected diagnostic tests. J. Order and make preliminary assessment of routine radiologic studies, including PA and lateral chests, KUB, GI, GB and extremity films. K. Know routine preparation for common X-ray studies. L. Be familiar with techniques of anoscopy, proctoscopy, sigmoidoscopy, bronchoscopy, gastroscopy and endoscopy and colonoscopy. M. Be familiar with techniques of thoracentesis, paracentesis, arthrocentesis, pericardiocentesis and lumbar puncture. N. Be familiar with routine nuclear medicine studies/reports. O. Be familiar with the technique of excisional biopsy. P. Recognize the signs and symptoms of complications of diagnostic procedures performed or ordered. Clinical Preceptor Manual *32 4. DIFFERENTIAL DIAGNOSIS: Develop a differential diagnosis and diagnostic impression considering the database. A. Develop a differential diagnosis and diagnostic impression at each stage of data collection. B. Demonstrate ability to organize and integrate data from the medical history, physical examination and diagnostic studies. C. Demonstrate sound medical judgment in formulating a differential diagnosis and reaching a diagnostic impression. D. Be familiar with the common medical problems seen in rural primary care and their modes of presentation. 5. THERAPEUTICS: Identify, perform and/or order appropriate, costeffective, routine therapeutic procedures and be able to assist the physician with other therapeutic procedures. A. Administer intravenous infusions utilizing appropriate equipment including scalp vein needle, butterfly needle, intravenous catheter, heparin lock and infusion pumps. B. Calculate infusion rate. C. Administer injections by a variety of routes including intradermal, subcutaneous, intramuscular and intravenous. D. Be familiar with normal nutritional requirements. E. Be familiar with dietary treatment of health problems including weight reduction, diabetic, low fat, low cholesterol and low sodium diets. F. Be familiar with the drugs used most frequently in treatment or health problems including basic modes of action, indications, contraindications and complications. G. Be familiar with the management of common medical problems. 6. HEALTH PROMOTION/DISEASE PREVENTION: Recognize, develop and implement effective strategies for incorporating health promotion/disease prevention into rural primary care practice. A. Know the appropriate, recommended health screening services for each gender through the lifespan. B. Know the risk factors for preventable diseases. C. Know the personal health behaviors that can predispose to illness. D. Know the recommended immunizations for each gender throughout the lifespan. E. Know the various chemoprophylactic regimens that can be offered to patients before they develop clinical evidence of disease. F. Instruct the female patient in self-breast examination technique and its importance. G. Recognize the importance of patient education in effecting change in the health status of both individuals and groups. 7. EMERGENCY SKILLS: Be able to recognize and manage lifethreatening emergencies jointly with, and in the absence of, the physician. A. Recognize signs and symptoms of common emergencies and take Clinical Preceptor Manual *33 B. C. D. E. F. G. H. I. J. K. L. M. N. O. appropriate action to sustain life. Apply basic techniques of CPR. 1. establish an airway 2. initiate or sustain effective ventilation 3. perform external cardiac massage Assist with or perform other techniques frequently indicated in lifethreatening situations. 1. endotracheal/nasogastric intubation 2. cricothyrotomy 3. defibrillation/cardioversion 4. central line insertion 5. central venous pressure monitoring Initiate hemostasis in patients with hemorrhage. Assess and treat hemorrhagic shock. Support and treat patients with anaphylactic reaction. Communicate with the physician regarding the patient’s emergency status as soon as possible. Administer and/or advise regarding the first aid indicated in the overdose, accidental ingestion or attempted suicide with drugs and other chemical agents. Know the reference sources regarding toxic materials. Recognize potentially lethal cardiac dysrhythmias and know the current treatment for each. Recognize altered mental status and its common causes and treatment. Understand the use of and indications for standard emergency medications and administer if appropriate. Be familiar with triage procedures in mass casualty situations. Respect the decision of the patient and/or family for no advanced life support procedures. Assess patients with multiple trauma, skull and/or spinal injuries. 8. COMMUNICATION: Be able to communicate in a medically professional manner, both orally and in writing, to the patient, the family and with health care professionals. A. Present to the physician a brief synopsis of the patient’s present illness, pertinent positive and negative findings and the diagnostic and therapeutic regimen instituted. B. Communicate effectively with both patient and family by using a vocabulary familiar to all concerned. C. Counsel patient and family regarding the health problem including an explanation of the disease process, therapy and its rationale, therapeutic options, prognosis and health care services available. D. Write routine and all other admission orders by the problem number. E. Write in a SOAP format, clear concise and relevant progress notes including diagnostic, therapeutic and patient education plans. F. Fill out routine laboratory test and diagnostic procedure request forms accurately and with pertinent data. Clinical Preceptor Manual *34 G. H. I. J. K. L. Maintain a complete up-to-date problem list. Initiate requests for patient services including public health and home nursing, school testing and evaluation and release of medical records. Report communicable diseases utilizing appropriate forms and follow-up. Write interval notes. Perform discharge summaries. Give empathetic support to both patient and family in all communications. 9. RESEARCH: Demonstrate knowledge of medical research methodologies and their application to rural primary care medicine. 10. ATTITUDE: Be able to appreciate the perceptions and reactions to health problems of the individual patient as well as those of culturally diverse population groups and approach each with sensitivity and an attitude of professional concern. A. Appreciate the physical, psychic, social and economic distress created by the health problem. B. Maintain the objectivity necessary to permit logical perspective, assessment and solution of the health problem. C. Appreciate the difficulty frequently encountered by patients in their attempts to comply with therapeutic regimens and the health care delivery system. D. Respect the right of the patient to be informed regarding his/her physical status, therapy, costs, therapeutic alternatives, prognosis and services available. E. Respect the patient’s rights to individuality and privacy, and treat confidential information with professional discretion. 11. ETHICS: Act consistently and responsibly for the patient’s welfare and best interests, showing respect for persons and their autonomy. A. Be committed to providing competent medical care, assuming as a primary responsibility the health, safety, welfare and dignity of all humans. B. Extend the full measure of ability as a dedicated, empathetic health care provider and assume responsibility for the skillful and proficient transaction of professional duties. C. Deliver needed health care services to health consumers without regard to sex, age, race, creed, sexual orientation, socio-economic and political status. D. Adhere to all state and federal laws governing informed consent concerning the patient’s health care. E. Seek consultation with their supervising physician, other health providers, or qualified professionals having special skills, knowledge or experience whenever the welfare of the patient will be safeguarded or advanced by such consultation. F. Take personal responsibility for being familiar with and adhering to all federal/state laws applicable to the practice of their profession. G. Provide only those services for which qualified via education and/or experiences and by pertinent legal regulatory process. H. Not misrepresent on any manner, either directly or indirectly, their skills, training, professional credentials, identity or services. Clinical Preceptor Manual *35 I. J. K. L. M. N. O. Uphold the doctrine of confidentiality regarding privileged patient information, unless required to release such information by law or such information becomes necessary to protect the welfare of the patient or the community. Strive to maintain and increase the quality of individual health care service through individual study and continuing education. Accept the duty to respect the law, uphold the dignity of the physician assistant profession and to accept its ethical principles. Not participate in or conceal any activity that will bring discredit or dishonor to the physician assistant profession and shall expose, without fear or favor, any illegal or unethical conduct in the medical profession. Use the knowledge and experience acquired as professionals to contribute to an improved community. Place service before material gain and carefully guard against conflicts of professional interest. Strive to maintain a spirit of cooperation with professional organizations and the general public. 12. SOCIAL/HISTORICAL: A. Rural Primary Care 1. Describe the historical processes that have created the contemporary health care system in the United States and in Appalachia particularly. 2. Interpret the unique historical forces that have shaped the Appalachian region. 3. Identify the exceptional health care needs of rural Appalachian citizens and evaluate the difficulties of health care delivery in rural communities. 4. Explain the historical development of the medical profession and evaluate the consequences of the elevation of physicians above other health care workers. 5. Define the relationships among various categories of health care professionals and analyze the historical role of each of these groups on the delivery of medical services to rural Appalachia. 6. Critique the current status of health care in Appalachia. 7. Become familiar with the sociologic concepts, theories and research methods in rural sociology. 8. Understand the structure and development of urban-rural patterns in the United States. 9. Become familiar with some of the major issues of rural sociology. B. Corrections Medicine 1. Describe the historical processes that have lead to the increased demand for providers to care for the incarcerated patient. 2. Identify the specific health care needs that are unique to patients within correctional facilities. 3. Identify the unique sociologic environment present within correctional facilities. 4. Critique the current status of health care within correctional settings. 5. Describe current sociologic concepts, theories, and research methods in the corrections environment. 6. Define the reporting relationships of personnel working within correctional settings. 7. Describe a plan that could serve to improve care to the incarcerated patient. Clinical Preceptor Manual *36 ROTATION OBJECTIVES GENERAL INTERNAL MEDICINE During the six-week general internal medicine rotation the PA student will develop appreciation for the care of the adult and geriatric patient with particular emphasis being placed on the uniqueness of such care in a rural setting. In addition to the requirements set forth in the segment “General Clinical Goals and Objectives” the student will: HISTORY 1. Be able to elicit an appropriate history from the adult or geriatric patient. a. Elicit detailed history regarding dietary habits, sleep patterns behavior changes use of medications (prescription or OTC), drugs or alcohol. b. Elicit history of hearing or visual disturbances c. Elicit information regarding patient’s home environment, support network and financial status. d. Elicit a careful comprehensive history through several interview sessions. e. Appropriately utilize a second party to augment information obtained from a patient. f. Be aware that the process of aging alters both the historical and physical manifestations of certain diseases. g. Be aware that geriatric patients may underreport illness. PHYSICAL EXAMINATION 1. Perform a physical examination on the adult or geriatric patient allowing for: a. Variations in physical findings among the elderly population. b. Common normal physical findings in the geriatric population. c. Abnormal physical findings that are found with increased frequency in this population. DIAGNOSTIC STUDIES 1. Identify, perform, order and/or interpret appropriate, cost-effective, routine diagnostic procedures, based on history and physical examination findings, and be able to assist the physician with other diagnostic procedures as directed. a. Identify the appropriate and available diagnostic tests for a particular problem based on the history and physical examination findings. b. Identify and discuss indications and contraindications of the various diagnostic tests. c. Identify and describe the risks, costs and patient inconvenience of various diagnostic tests. Clinical Preceptor Manual *37 d. Demonstrate skills required to collect routine specimens. 1. bacteriologic samples 2. bloods, venous and arterial 3. gastric contents 4. sputum 5. stool 6. tissues 7. urine e. Demonstrate skills necessary to perform and/or interpret basic laboratory tests. 1. CBC 2. gram stain 3. stool, O&P 4. stool, guaiac 5. urinalysis, dipstick 6. wet prep/KOH 7. pregnancy test 8. alcohol screening f. Demonstrate skills necessary to perform and interpret a 12 lead EKG and rhythm strip. g. Administer, interpret and record results of intradermal skin test. h. Demonstrate skills necessary to perform and interpret screening tonometry and audiometry tests. i. Identify, order and/or perform and/or interpret other selected diagnostic tests. j. Order and make preliminary assessment of routine radiologic studies, including PA and lateral chests, KUB, GI, GB and extremity films. k. Know routine preparation for common X-ray studies. l. Be familiar with techniques of anoscopy, proctoscopy, sigmoidoscopy, bronchoscopy, gastroscopy and endoscopy and colonoscopy. m.Be familiar with techniques of thoracentesis, paracentesis, arthrocentesis, pericardiocentesis and lumbar puncture. n. Be familiar with routine nuclear medicine studies/reports. o. Be familiar with the technique of excisional biopsy. p. Recognize the signs and symptoms of complications of diagnostic procedures performed or ordered. DIFFERENTIAL DIAGNOSIS 1. Develop a differential diagnosis and diagnostic impression considering the database a. Develop a differential diagnosis and diagnostic impression at each stage of data collection. b. Demonstrate the ability to organize and integrate data from the medical history, physical examination, and diagnostic studies. c. Demonstrate sound medical judgment in formulating a differential diagnosis. d. Demonstrate skills necessary to accurately record and present data in a manner appropriate to the setting. e. Be familiar with the common medical problems and their modes of presentation, including: Clinical Preceptor Manual *38 CARDIOLOGY Cardiac Risk Factors Coronary Artery Disease Angina/Myocardial Infarction Pericarditis Congestive Heart Failure Arrhythmias Arterial Disease Aneurysm/Occlusion Venous thrombosis/Insufficiency Valvular Heart Disease Endocarditis Hypertension Cardiac Rehabilitation PULMONARY MEDICINE Chronic Obstructive Pulmonary Disease Asthma Bronchitis/Acute & Chronic Emphysema Infections-pneumonia Cancers of the lung and pleura Pulmonary Function Testing/Arterial Blood Gases Pulmonary Embolism/Pneumothorax/Hemothorax Inhalational and Environmental Injury Silo-Fillers Disease(Hypersensitivity Pneumonitis) Farmer’s Lung Black Lung-Coal worker’s Pneumoconiosis Tobacco abuse/cessation Pulmonary Edema/Hypertension NEPHROLOGY/UROLOGY Acid Base Balance and Electrolyte Disturbances Urinary Tract Infections /Pyelonephritis Glomerulonephritis/Nephrotic Syndrome Acute Renal Failure Chronic Renal Failure/Dialysis Nephrolithiasis Prostatitis Sexually Transmitted Diseases Nephrotoxins NEUROLOGY Seizure Disorder Headaches Meningitis/Encephalitis Cerebrovascular Disease:TIA/CVA Multiple Sclerosis Tremors/Parkinson’s Neuropathies: Cranial/Peripheral Spinal Disc Disease Coma/CNS Trauma GASTROENTEROLOGY GERD/Spasm, Stricture, Dysmotility PUD/Gastritis Pancreatitis Malabsorption Ulcerative Colitis Crohn’s Disease Diverticular Disease Hemorrhoids/Fissures/Fistulas Neoplasms of the GI Tract Hepatitis: Infectious/Non-Infectious Jaundice Alcoholic Liver Disease Cholecystitis/Cholelithiasis Cholangitis Diarrhea/Constipation Infections: Viral, Bacterial, Parasitic Irritable Bowel Syndrome RHEUMATOLOGY Osteoarthritis Infectious Arthritis: Viral/Bacterial/Lyme Clinical Preceptor Manual *39 Rheumatoid Arthritis Gout/Psuedogout Spondyloarthropathies Collagen Vascular Disease ENDOCRINOLOGY Diabetes Mellitus Hypoglycemia Diabetes Insipidus Thyroid Disease Hyperlipidemia Adrenal Cortical Insufficiency DERMATOLOGY Allergic/Contact Dermatitis Acne Skin Tumors Infection: Viral, Bacterial Fungal, Parasitic Psoriasis/Eczema Dermatologic Manifestations of Systemic Disease IMMUNOLOGY/HEMATOLOGY Anemias Bleeding Disorders Leukemias Lymphomas/Hodgkin’s/ Non-Hodgkin’s Immune Deficiencies ALLERGY Anaphylaxis Hypersensitivity OPHTHAMOLOGY Conjunctivitis/Uveitis/Iritis-The Red Eye Cataracts Glaucoma Corneal Abrasion Retinal Changes Secondary to Systemic Disease ENT Hearing Loss Vertigo Infections: Viral/Bacterial Allergic Rhinitis/Sinusitis MENTAL HEALTH Neurotic Disorders Psychiatric Emergencies Depression Sleep Disorders Bipolar Disorder Post Traumatic Stress Syndrome Schizophrenic Disorders Anxiety Paranoid Disorders Somatoform Disorders Affective Disorders Personality Disorders Dementia Substance Abuse and Dependence Clinical Preceptor Manual *40 THERAPEUTICS 1. Identify, perform and/or order appropriate, cost-effective, routine therapeutic procedures and be able to assist the physician with other therapeutic procedures. a. Administer intravenous infusions utilizing appropriate equipment including butterfly needle, intravenous catheter, heparin lock and infusion pumps. b. Calculate infusion rate. c. Administer injections by a variety of routes including intradermal, subcutaneous, intramuscular and intravenous. d. Be familiar with normal nutritional requirements. e. Be familiar with dietary treatment of health problems including weight reduction, diabetic, low fat, low cholesterol and low sodium diets. f. Be familiar with the drugs used most frequently in treatment or health problems including basic modes of action, indications, contraindications and complications. g. Be familiar with the management of common medical problems. HEALTH PROMOTION/DISEASE PREVENTION 1. Recognize, develop and implement effective strategies for incorporating health promotion/disease prevention into rural primary care practice. a. Know the appropriate, recommended health screening services for each gender through the lifespan. b. Know the risk factors for preventable diseases. c. Know the personal health behaviors that can predispose to illness. d. Know the recommended immunizations for each gender throughout the lifespan. e. Know the various chemoprophylactic regimens that can be offered to patients before they develop clinical evidence of disease. f. Instruct the female patient in self-breast examination technique and its importance. g. Recognize the importance of patient education in effecting change in the health status of both individuals and groups. EMERGENCY SKILLS 1. Be able to recognize and manage life-threatening emergencies jointly with, and in the absence of, the physician. a. Recognize signs and symptoms of common emergencies and take appropriate action to sustain life. b. Apply basic techniques of CPR. 1. establish an airway 2. initiate or sustain effective ventilation 3. perform external cardiac massage c. Assist with or perform other techniques frequently indicated in lifethreatening situations. 1. endotracheal/nasogastric intubation 2. cricothyrotomy Clinical Preceptor Manual *41 d. e. f. g. h. i. j. k. l. m. n. o. 3. defibrillation/cardioversion 4. central line insertion 5. central venous pressure monitoring Initiate hemostasis in patients with hemorrhage. Assess and treat hemorrhagic shock. Support and treat patients with anaphylactic reaction. Communicate with the physician regarding the patient’s emergency status as soon as possible. Administer and/or advise regarding the first aid indicated in the overdose, accidental ingestion or attempted suicide with drugs and other chemical agents. Know the reference sources regarding toxic materials. Recognize potentially lethal cardiac dysrhythmias and know the current treatment for each. Recognize altered mental status and its common causes and treatment. Understand the use of and indications for standard emergency medications and administer if appropriate. Be familiar with triage procedures in mass casualty situations. Respect the decision of the patient and/or family for no advanced life support procedures. Assess patients with multiple trauma, skull and/or spinal injuries. COMMUNICATION 1. Be able to communicate in a medically professional manner, both orally and in writing, to the patient, the family and with health care professionals. a. Present to the physician a brief synopsis of the patient’s present illness, pertinent positive and negative findings and the diagnostic and therapeutic regimen instituted. b. Communicate effectively with both patient and family by using a vocabulary familiar to all concerned. c. Counsel patient and family regarding the health problem including an explanation of the disease process, therapy and its rationale, therapeutic options, prognosis and health care services available. d. Write routine and all other admission orders by the problem number. e. Write in a SOAP format, clear concise and relevant progress notes including diagnostic, therapeutic and patient education plans. f. Fill out routine laboratory test and diagnostic procedure request forms accurately and with pertinent data. g. Maintain a complete up-to-date problem list. h. Initiate requests for patient services including public health and home nursing, school testing and evaluation and release of medical records. i. Report communicable diseases utilizing appropriate forms and follow-up. j. Write interval notes. k. Perform discharge summaries. l. Give empathetic support to both patient and family in all communications. Clinical Preceptor Manual *42 RESEARCH 1. Demonstrate an awareness of the recognized internal medicine literature, current issues and controversies in the literature and methods of accessing current literature while in rural sites. ATTITUDE 1. Demonstrate an understanding of the effects of illness on the patient, family and the community. 2. Demonstrate an understanding of the difference between minor problems and those that require intense therapy and treatment. 3. Demonstrate awareness that drug and alcohol abuse is a common problem. 4. Demonstrate an understanding of the medical/legal aspects of dealing with health problems. 5. Demonstrate an appreciation for the need to refer patients to community agencies and therapists. 6. Demonstrate an appreciation for awareness of age dependent mental health problems. 7. Demonstrate awareness for the scope of the health care system and understand how it affects scope and access to patient care services. 8. Demonstrate awareness for the respect of the legal rights of patients, including confidentiality. Clinical Preceptor Manual *43 ROTATION OBJECTIVES OBSTETRICS AND GYNECOLOGY During the six-week obstetrics and gynecology rotation exposure to some or all of the following subject matter will be provided. In addition to the general objectives, the student on the Obstetrics and Gynecology rotation should achieve the following objectives: HISTORY 1. Elicit an appropriate complete obstetrical and gynecologic history. a. Elicit a pertinent review of symptoms of pregnancy. b. Elicit a comprehensive obstetrical history c. Elicit a history of untoward reaction to anesthesia d. Elicit a history pertaining to sexuality, STD, menstrual cycles, and contraceptive use. 2. Calculate the EDC PHYSICAL EXAMINATION 1. Demonstrate the appropriate use of the fetoscope 2. Perform a pelvic examination a. Prenatal b. Postpartum c. Gynecologic d. Under anesthesia 3. Perform thorough examination of the prenatal abdomen. a. Measure uterine height b. Auscultate the fetal heart and note discrepancies from gestational dates c. Determine fetal lie 4. Perform Pelvimetry. 5. Assess and document membrane rupture. 6. Determine cervical dilation, effacement and station. 7. Examine the placenta for abnormalities 8. Examine the postpartum abdomen for uterine size DIAGNOSTIC STUDIES 1. 2. 3. 4. 5. 6. 7. 8. 9. Formulate a high-risk pregnancy problem list Apply fetal monitoring system electrodes Interpret fetal monitoring tracings Assist in performing amniocentesis Assist/observe obstetric ultrasound Assist in performing contraction stress and nonstress testing Assess contractions, vital signs, and reflexes during labor. Obtain Pap smears as indicated. Obtain various cultures as indicated: a. Gonorrhea Clinical Preceptor Manual *44 b. Chlamydia c. Herpes simplex d. Group B beta strep 10. Demonstrate skills necessary to perform and/or interpret basic laboratory tests. a. CBC b. stool, guaiac c. urinalysis, dipstick d. wet prep/KOH e. pregnancy test f. hormonal assays: LH, FSH, Prolactin, Testosterone, DHEAS, Thyroid Function Tests 11. Assist/perform biopsies: a. Vulvar b. Cervical c. Endocervical d. Endometrial 12. Be familiar with the techniques of: a. Post-coital test b. Basal body temperature charting and interpretation c. Artificial insemination d. Hysterosalpingogram e. Pelvic ultrasound 13. Participate in diagnostic laparoscopy, colposcopy DIFFERENTIAL DIAGNOSIS 1. Demonstrate and discuss the common obstetric and gynecologic conditions and problems and their typical presentations including: OBSTETRICS Fetal Development Prenatal Care Normal Labor and Delivery High Risk Pregnancy Toxemia of Pregnancy/PIH Medical Complications of Pregnancy Obstetrical Anesthesia Postpartum Care Abruptio Placenta Placenta Previa Ectopic Pregnancy Abortion Intrauterine Death Cesarean Section Genetic Counseling Amniocentesis Ultrasonography/Fetal Monitoring Fetal Activity Testing Clinical Preceptor Manual *45 GYNECOLOGY Menstruation/normal and altered throughout the life cycle Osteoporosis and prevention Dysfunctional Uterine Bleeding Menopause Contraception Premenstrual Syndrome Infertility PID Endometriosis Breast Disease Benign/Malignant Lesion of the Reproductive Tract Vaginitis Sexual Dysfunction Amenorrhea Common Gynecologic Surgeries THERAPEUTICS 1. Know the accepted treatment for the above conditions. 2. Describe and discuss the dietary treatment of obstetrical problems and special dietary needs of the obstetrical patient. 3. Give support to the patient in labor. 4. Employ proper delivery room protocol. 5. Manage a normal delivery. 6. Recognize the indication for episiotomies. 7. Know which drugs are safe to use during pregnancy and lactation and which should not be used and why. 8. Insert/Remove IUD’s and manage side effects or complications related to them. 9. Fit diaphragms and cervical caps. 10. Insert/remove Norplant and manage side effects or complications related to them. 11. Prescribe oral contraceptives and Depo-Provera and manage side effects or complications related to them. HEALTH PROMOTION/DISEASE PREVENTION 1. Know, and counsel the obstetric patient about, the current recommendations regarding: a. Screening for HIV b. Screening for chlamydial infections c. Screening for genital herpes d. Screening for asymptomatic bacteriuria e. Screening for rubella f. Screening ultrasonography g. Screening for preeclampsia h. Screening for RH incompatibility i. Screening for neural tube defects j. Screening for hemoglobinopathies k. Screening for PKU l. Screening for congenital hypothyroidism m.Intrapartum electronic fetal monitoring Clinical Preceptor Manual *46 2. Know, and counsel the gynecologic patient about, the current recommendations regarding: a. Screening for breast cancer, including self-breast exam and mammography b. Screening for cervical cancer c. Screening for ovarian cancer d. Screening for osteoporosis e. Prevention of osteoporosis f. Hormone replacement therapy in the postmenopausal patient g. Screening for sexually transmitted diseases EMERGENCY SKILLS 1. Recognize and institute the initial management of emergency gynecologic and obstetric emergencies in the absence of the physician, such as: a. ectopic pregnancy b. obstetrical hemorrhage c. preeclampsia/eclampsia/PIH d. preterm labor e. intrapartum fetal distress f. postpartum hemorrhage/infection g. sepsis h. embolic phenomena i. dysfunctional uterine bleeding j. pelvic inflammatory disease k. torsion of ovarian cyst l. know the protocol for medical evaluation of rape/domestic abuse COMMUNICATION 1. Counsel patients and their family regarding pregnancy and childbirth, explaining the normal processes, complications and instruct regarding the importance of adequate nutrition and prenatal and postpartum care. 2. Counsel patients regarding breastfeeding vs. bottle feeding. 3. Maintain a complete prenatal and L&D record. 4. Counsel patients regarding birth control and sexual concerns. 5. Counsel patients regarding premenstrual syndrome. 6. Counsel patients regarding menopausal symptoms, osteoporosis, and hormone replacement therapy. 7. Counsel patients regarding sexually transmitted diseases. 8. Counsel patients regarding infertility. 9. Counsel patients regarding keeping a basal body temperature chart and in the use of ovulation predictor kits. 10. Counsel patients regarding the normal menstrual cycle and expected changes over the lifespan. 11. Counsel patients regarding rape and domestic abuse. Clinical Preceptor Manual *47 RESEARCH 1. Demonstrate an awareness of the recognized obstetric and gynecologic medical literature, current issues and controversies in the literature and methods of accessing current literature while in rural sites. ATTITUDE 1. Demonstrate an understanding of the role and range of female sexuality, showing sensitivity to its variable expression among individuals and different social and cultural groups. 2. Demonstrate an understanding of, and show sensitivity to, the emotional and physical changes experienced by women throughout the lifespan. Clinical Preceptor Manual *48 ROTATION OBJECTIVES GENERAL SURGERY During the six-week general surgical rotation, exposure to some or all of the following subject matter will be provided. In addition to the general objectives previously listed the student will accomplish the following: HISTORY 1. Elicit a history of untoward reactions to anesthesia. 2. Elicit a history of diseases that affect the advisability of surgery. 3. Elicit a history of recurrent or progressive surgical problems. 4. Elicit a history pertaining to prior surgical complications. 5. Elicit a post-operative history. PHYSICAL EXAMINATION Perform an appropriate physical examination for the surgical patient DIAGNOSTIC STUDIES 1. Identify, perform, order and/or interpret appropriate, cost-effective, routine diagnostic procedures, based on history and physical examination findings, and be able to assist the physician with other diagnostic procedures as directed. a. Identify the appropriate and available diagnostic tests for a particular problem based on the history and physical examination findings. b. Identify and discuss indications and contraindications of the various diagnostic tests. c. Identify and describe the risks, costs and patient inconvenience of various diagnostic tests. d. Demonstrate skills required to collect routine specimens. 1. bacteriologic samples 2. blood, venous and arterial 3. gastric contents 4. sputum 5. stool 6. tissues 7. urine e. Demonstrate skills necessary to perform and/or interpret basic laboratory tests. 1. CBC 2. gram stain 3. stool, O&P 4. stool, guaiac 5. urinalysis, dipstick 6. wet prep/KOH 7. pregnancy test Clinical Preceptor Manual *49 8. alcohol screening f. Demonstrate skills necessary to perform and interpret a 12 lead EKG and rhythm strip. g. Administer, interpret and record results of intradermal skin test. h. Demonstrate skills necessary to perform and interpret screening tonometry and audiometry tests. i. Identify, order and/or perform and/or interpret other selected diagnostic tests. j. Order and make preliminary assessment of routine radiologic studies, including PA and lateral chests, KUB, GI, GB and extremity films. k. Know routine preparation for common X-ray studies. l. Be familiar with techniques of anoscopy, proctoscopy, sigmoidoscopy, bronchoscopy, gastroscopy and endoscopy and colonoscopy. m.Be familiar with techniques of thoracentesis, paracentesis, arthrocentesis, pericardiocentesis and lumbar puncture. n. Be familiar with routine nuclear medicine studies/reports. o. Be familiar with the technique of excisional biopsy. p. Recognize the signs and symptoms of complications of diagnostic procedures performed or ordered. DIFFERENTIAL DIAGNOSIS 1. Describe and discuss common surgical problems, concerns and their modes of presentation, including: GENERAL pre/post operative care wound care and infections Anesthesia aseptic technique principles of suturing fluid and electrolyte balance and acid base surgical nutrition/hyperalimentation shock trauma care burns organ transplantation SYSTEMS Breasts-Tumors/reconstruction CARDIOVASCULAR Arterial by-pass grafting Aneurysms Venous ligation Arterial reconstruction THORAX Lung biopsy/resection Clinical Preceptor Manual *50 ABDOMEN Acute surgical abdomen Appendectomy Bowel resection Laparscopic procedures Cholecystectomy Liver Bx Herniorrhaphy Gastric Procedures-fundoplication/V&P/ UROLOGY Prostatectomy Nephrolithiasis Prostatic/Testicular tumors TURP Vasectomy ORTHOPEDICS Common Knee Injuries Common Shoulder Injuries Arthroscopy/Arthroplasty Hand Injuries ORIF Fractures NEUROSURGERY Cervical/lumbar disc disease Common cranial tumors VP Shunts for hydrocephalus Management of increased intercranial pressure Repair AVM THERAPEUTIC SKILLS The PA student will demonstrate the following knowledge, skills and abilities during their surgical rotation. 1. Discuss the composition of fluids that are frequently lost from the body including urine, gastric secretions, diarrhea, third space fluids, and hemorrhage. 2. Discuss the relationships between serum electrolytes and IV therapy and the need to adjust therapy based on lab results and physical signs. 3. Recognize the problems associated with hypo and hypervolemia. 4. Describe blood and blood products utilized in IV therapy and the indications, precautions, contraindications, and complications of their use. 5. Recognize the drugs most frequently used in treatment of surgical problems, including basic modes of actions, indication, contraindications, and complications. 6. Describe pre-op and post-op management of surgical patients. 7. Discuss anesthetics, their indications, modes of action, contraindications, complications, and combinations in: a. General anesthesia b. Spinal and regional anesthesia c. Regional anesthesia/field blocks Clinical Preceptor Manual *51 8. Utilize infiltration anesthesia. 9. Apply casts, splints, or wraps to immobilize the injured structure. 10. Assemble surgical instruments necessary for wound closure and use these instruments appropriately. 11. Set up a sterile field and prep the injured area. 12. Employ proper techniques for closing wounds. a. Aseptic technique b. Hemostasis c. Closure of dead space d. Approximation of like tissues e. Know various techniques for dermal closure 1. Simple stitch 2. Vertical/horizontal mattress 3. Running stitch 4. Running subcuticular 5. Specialty closure techniques 13. Discuss the different types of suture materials and their uses including silk, gut, chromic, nylon, dacron, vicryl, and PDS. 14. Demonstrate I&D of an abscess. 15. Instruct the patient in proper wound care. 16. Assess wound healing. 17. Remove sutures/staples. 18. Describe fluid therapy in burn patients. 19. Demonstrate proper use of topical antibiotics. 20. Demonstrate how to dress wounds including burn dressings. 21. Demonstrate management of burn patients, including nutrition and burn complications. 22. Demonstrate/Discuss the management of common surgical problems as listed above. HEALTH PROMOTION/DISEASE PREVENTION 1. Recognize, develop and implement effective strategies for incorporating health promotion/disease prevention into rural primary care practice. a. Know the appropriate, recommended health screening services for each gender through the lifespan. b. Know the risk factors for preventable diseases. c. Know the personal health behaviors that can predispose to illness. d. Know the recommended immunizations for each gender throughout the lifespan. e. Know the various chemoprophylactic regimens that can be offered to patients before they develop clinical evidence of disease. f. Instruct the female patient in self-breast examination technique and its importance. g. Recognize the importance of patient education in effecting change in the health status of both individuals and groups. Clinical Preceptor Manual *52 EMERGENCY SKILLS 1. Be able to recognize and manage life-threatening emergencies jointly with, and in the absence of, the physician. a. Recognize signs and symptoms of common emergencies and take appropriate action to sustain life. b. Apply basic techniques of CPR. 1. establish an airway 2. initiate or sustain effective ventilation 3. perform external cardiac massage c. Assist with or perform other techniques frequently indicated in lifethreatening situations. 1. endotracheal/nasogastric intubation 2. cricothyrotomy 3. defibrillation/cardioversion 4. central line insertion 5. central venous pressure monitoring d. Initiate hemostasis in patients with hemorrhage. e. Assess and treat hemorrhagic shock. f. Support and treat patients with anaphylactic reaction. g. Communicate with the physician regarding the patient’s emergency status as soon as possible. h. Administer and/or advise regarding the first aid indicated in the overdose, accidental ingestion or attempted suicide with drugs and other chemical agents. i. Know the reference sources regarding toxic materials. j. Recognize potentially lethal cardiac dysrhythmias and know the current treatment for each. k. Recognize altered mental status and its common causes and treatment. l. Understand the use of and indications for standard emergency medications and administer if appropriate. m. Be familiar with triage procedures in mass casualty situations. n. Respect the decision of the patient and/or family for no advanced life support procedures. o. Assess patients with multiple trauma, skull and/or spinal injuries. COMMUNICATION 1. Be able to communicate in a medically professional manner, both orally and in writing, to the patient, the family and with health care professionals. a. Present to the physician a brief synopsis of the patient’s present illness, pertinent positive and negative findings and the diagnostic and therapeutic regimen instituted. b. Communicate effectively with both patient and family by using a vocabulary familiar to all concerned. c. Counsel patient and family regarding the health problem including an explanation of the disease process, therapy and its rationale, therapeutic Clinical Preceptor Manual *53 d. e. f. g. h. i. j. k. l. options, prognosis and health care services available. Write routine and all other admission orders by the problem number. Write in a SOAP format, clear concise and relevant progress notes including diagnostic, therapeutic and patient education plans. Fill out routine laboratory test and diagnostic procedure request forms accurately and with pertinent data. Maintain a complete up-to-date problem list. Initiate requests for patient services including public health and home nursing, school testing and evaluation and release of medical records. Report communicable diseases utilizing appropriate forms and follow-up. Write interval notes. Perform discharge summaries. Give empathetic support to both patient and family in all communications. RESEARCH 1. Demonstrate knowledge of medical research methodologies and their application to rural primary care medicine. 2. Demonstrate the ability to obtain current surgical literature when located in remote areas. ATTITUDE 1. Demonstrate an understanding for the anxiety produced by the prospect of surgery and/or anesthesia for the patient and the family. 2. Demonstrate an understanding for the patient’s concern over body disfigurement. 3. Demonstrate an understanding for the emotional sequelae experienced by the victim of acute trauma. Clinical Preceptor Manual *54 ROTATION OBJECTIVES PEDIATRICS During the six-week pediatric rotation exposure to some, or all of, the following subject matter will be provided. In addition to the objectives previously listed the student will be responsible for the following: HISTORY 1. Obtain a complete or partial history from or regarding pediatric patients of any age. 2. Elicit a well baby history including physical growth, mental and emotional development, immunizations, and the historical components of Denver Developmental Screening Exam. 3. Elicit dietary history including formula used, amount taken, feeding per twentyfour hours, dates starting new foods, food intolerance, and history of pica. 4. Utilize techniques required to obtain an adolescent history including school performance, peer interactions, substance abuse, sexual activity, and tobacco use. PHYSICAL EXAMINATION 1. Be able to perform a complete and partial physical examination on pediatric patients. 2. Develop skills that assist in the examination of the uncooperative child. 3. Perform examination of the newborn 4. Demonstrate APGAR Scoring 5. Determine gestational age by examination. 6. Measure, record and chart height, weight, and head circumference on standard nomograms. 7. Utilize screening exams to augment the basic physical examination. DIAGNOSTIC STUDIES 1. Identify, perform, order and/or interpret appropriate, cost-effective, routine diagnostic procedures, based on history and physical examination findings, and be able to assist the physician with other diagnostic procedures as directed. a. Identify the appropriate and available diagnostic tests for a particular problem based on the history and physical examination findings. b. Identify and discuss indications and contraindications of the various diagnostic tests. c. Identify and describe the risks, costs and patient inconvenience of various diagnostic tests. d. Demonstrate skills required to collect routine specimens. 1. bacteriologic samples 2. blood, venous and arterial 3. gastric contents 4. sputum Clinical Preceptor Manual *55 5. stool 6. tissues 7. urine e. Demonstrate skills necessary to perform and/or interpret basic laboratory tests. 1. CBC 2. gram stain 3. stool, O&P 4. stool, guaiac 5. urinalysis, dipstick 6. wet prep/KOH 7. pregnancy test 8. alcohol screening f. Demonstrate skills necessary to perform and interpret a 12 lead EKG and rhythm strip. g. Administer, interpret and record results of intradermal skin test. h. Demonstrate skills necessary to perform and interpret screening audiometric testing. i. Identify, order and/or perform and/or interpret other selected diagnostic tests. j. Order and make preliminary assessment of routine radiologic studies, including PA and lateral chests, KUB, GI, and extremity films. k. Know routine preparation for common X-ray studies. l. Be familiar with techniques of anoscopy, proctoscopy, sigmoidoscopy, bronchoscopy, gastroscopy and endoscopy and colonoscopy. m.Be familiar with techniques of thoracentesis, paracentesis, arthrocentesis, pericardiocentesis and lumbar puncture. n. Be familiar with routine nuclear medicine studies/reports. o. Be familiar with the technique of excisional biopsy. p. Recognize the signs and symptoms of complications of diagnostic procedures performed or ordered. DIFFERENTIAL DIAGNOSIS 1. Describe and discuss common pediatric problems and concerns and their modes of presentation including: GENERAL Newborn Exam Problems in the neonate Fluids and Electrolytes Poisonings Mental Retardation Child Abuse Failure to Thrive Well Baby/Child Exams Acid Base Balance Growth and Development Genetic Disorders/Counseling Fever of unknown origin Communicable Disease Immunizations Learning Disabilities Adolescent Medicine Depression/Suicide Clinical Preceptor Manual *56 CARDIOLOGY Congenital Heart Disease RESPIRATORY URI Pharyngitis Pneumonia Respiratory Distress Syndrome Cystic Fibrosis Otitis Media/Otitis Externa Croup/Epiglottitis Bronchitis/Bronchiolitis Asthma GASTROINTESTINAL Infection: bacterial, viral, parasitic Hyperbilirubinemia Congenital anomalies Diarrhea/Dehydration Constipation GENITOURINARY Urinary Tract infections Vaginitis Vesicoureteral reflux Hematuria Tumors ORTHOPAEDICS Common Fractures Congenital abnormalities Dislocations/Subluxations ENDOCRINE Diabetes Thyroid Disease Congenital Endocrinopathies NEUROLOGY Meningitis Seizure Disorder Encephalitis Pediatric Headaches DERMATOLOGY Viral exanthems Parasitic Infections Acne Contact Dermatitis Impetigo Miliaria Eczema Tinea/Monilial Infections Allergic Dermatitis Clinical Preceptor Manual *57 THERAPEUTICS 1. 2. 3. 4. 5. Monitor serum drug levels in patients on long term treatment. Remove cerumen from the external auditory canal using various techniques. Perform and or interpret audiometry and/or tympanometry. Administer immunizations using the recommended schedule. Demonstrate techniques that are unique to the pediatric patient in advanced life support. 6. Obtain IV access on the pediatric patient. 7. Perform urethral catheterization on the pediatric patient. 8. Demonstrate appropriate treatment of the above conditions. HEALTH PROMOTION/DISEASE PREVENTION 1. Recognize, develop and implement effective strategies for incorporating health promotion/disease prevention into rural primary care practice. a. Know the appropriate, recommended health screening services for each gender through the lifespan. b. Know the risk factors for preventable diseases. c. Know the personal health behaviors that can predispose to illness. d. Know the recommended immunizations for each gender throughout the lifespan. e. Know the various chemoprophylactic regimens that can be offered to patients before they develop clinical evidence of disease. f. Instruct the female patient in self-breast examination technique and its importance. g. Recognize the importance of patient education in effecting change in the health status of both individuals and groups. EMERGENCY SKILLS 1. Be able to recognize and manage life-threatening emergencies jointly with, and in the absence of, the physician. a. Recognize signs and symptoms of common emergencies and take appropriate action to sustain life. b. Apply basic techniques of CPR and Pediatric Advanced Life Support. 1. establish an airway 2. initiate or sustain effective ventilation 3. perform external cardiac massage c. Assist with or perform other techniques frequently indicated in lifethreatening situations. 1. endotracheal/nasogastric intubation 2. defibrillation/cardioversion 3. central line insertion d. Initiate hemostasis in patients with hemorrhage. e. Assess and treat hemorrhagic shock. f. Support and treat patients with anaphylactic reaction. Clinical Preceptor Manual *58 g. h. i. j. k. l. m. n. o. Communicate with the physician regarding the patient’s emergency status as soon as possible. Administer and/or advise regarding the first aid indicated in the overdose, accidental ingestion or attempted suicide with drugs and other chemical agents. Know the reference sources regarding toxic materials. Recognize potentially lethal cardiac dysrhythmias and know the current treatment for each. Recognize altered mental status and its common causes and treatment. Understand the use of and indications for standard emergency medications and administer if appropriate. Be familiar with triage procedures in mass casualty situations. Respect the decision of the patient and/or family for no advanced life support procedures. Assess patients with multiple trauma, skull and/or spinal injuries. COMMUNICATION 1. Counsel the patient and parents on a variety of subjects including, but not limited to, growth and development, nutrition, childhood fears, accident prevention, preparation for school, obesity, immunizations, and discipline. 2. Counsel the adolescent regarding common adolescent concerns a. Explain the process of physical and emotional maturing. b. Reassure the patient about sexually related matters including development, menstruation, masturbation, sexual intercourse, birth control, and abortion. c. Explain disease processes as they relate to the adolescent’s medical problems. d. Counsel the adolescent in problems related to smoking, drugs and alcohol use. RESEARCH 1. Demonstrate an awareness of the recognized pediatric medical literature, current issues and controversies in the literature and methods of accessing current literature while in rural sites. ATTITUDE 1. Demonstrate an understanding of the parents’ concern for the child, and their anxiety over any pediatric problems. 2. Demonstrate an understanding of the emotional trauma suffered by the battered/abused child as well as the psychiatric problems of the adult inflicting the injury. 3. Demonstrate an understanding of the increasing incidence of adolescent suicide. Clinical Preceptor Manual *59 ROTATION OBJECTIVES CARDIOLOGY During the students rotation in cardiology exposure to some or all of the following subject matter will be provided. The student will gain experience and proficiency working as a member of an organized health care team. Emphasis shall be placed on developing skills and cognitive knowledge that will help the student perform well in a primary care setting. Additional objectives to be attained by the student are as follows: BASIC SCIENCE 1. Describe the anatomy of the cardiovascular system 2. Describe the physiologic function of the cardiovascular system 3. Describe pathophysiologic mechanisms involved in the following a. Ischemic Heart Disease and Acute MI b. Congestive Heart Failure c. Cardiomyopathies and Myocarditis d. Pericardial Disease e. Hypertension f. Arteriosclerosis g. Cardiac Arrhythmias h. Cardiogenic Shock HISTORY 1. Elicit and record an appropriate cardiovascular history including: a. Cardiovascular review of systems b. Past medical history pertinent to the cardiovascular system c. Social history pertinent to the cardiovascular system d. Family history pertinent to the cardiovascular system e. Current medications f. Drug allergies g. Cardiovascular disease risk factors 2. Recognize the classic historical presentation of the following etiologies of chest pain and shortness of breath a. Angina Pectoris b. Acute Myocardial Infarction c. Congestive Heart Failure d. Pericarditis e. COPD f. Musculoskeletal including muscle strain and costochondritis g. Neurogenic including Herpes Zoster and radiculopathies h. Pulmonary Embolus i. Pneumonia j. Pleuritis k. Pneumothorax/hemothorax Clinical Preceptor Manual *60 PHYSICAL EXAMINATION 1. Given a patient or historical, and laboratory data perform a comprehensive cardiovascular examination 2. Describe various normal and abnormal findings on the cardiovascular examination and further describe their etiology including: a. Normal heart sounds (S1, S2, physiologic splitting, Physiologic S3) b. Abnormal heart sounds(S3, S4, murmurs, rubs, valvular opening sounds, etc) c. Lifts, heaves and thrills d. Diminished or absent pulses e. Bruits f. Venous hums g. JVD and Hepatojugular reflux h. Skin changes consistent with various types of cardiovascular disease(cyanosis etc) DIFFERENTIAL DIAGNOSIS 1. Given a patient or historical, physical and laboratory findings differentiate between the following: a. Stable and unstable angina b. Acute myocardial infarction c. Variant angina d. Pericarditis e. Cardiomyopathy f. Pulmonary embolus g. Pneumonia h. Pneumothorax i. Herpes Zoster or other chest pain of neurogenic etiology j. Atypical chest pain k. Musculoskeletal chest pain l. Psychogenic chest pain DIAGNOSTIC STUDIES 1. Given a rhythm strip differentiate between the following arrhythmias/conditions: a. Tachy-arrhythmias 1. Atria Fib Flutter 2. PSVT 3. Sinus tachycardia 4. Ventricular tachycardia/fibrillation 5. WPW syndrome b. Brady-arrhythmias c. Sinus bradycardia 1. 1st, 2nd, and 3rd degree heart block Clinical Preceptor Manual *61 2. Asystole d. Premature contractions from various locations (APC’s VPC’s, JPC’s, etc) 3. Given a 12 lead EKG be able to identify the following conditions: a. Myocardial infarct patterns b. Pericarditis c. Bundle branch blocks d. LVH e. RVH 4. Describe the possible etiologies of abnormal cardiac enzymes including a. CPK/Fractions b. SGOT c. LDH 5. Classify various lipid abnormalities (hyper and dyslipidemias), describe secondary etiologies and prescribe treatment based on NCEP guidelines THERAPEUTIC 1. Describe an approach to management, following JNC guidelines, of hypertension 2. Describe an approach to management of the patient with ischemic heart disease including acute MI and angina pectoris 3. Describe an approach to management of asystole, tachy & brady arrhythmias 4. Describe and approach to managing the patient with CHF HEALTH PROMOTION AND DISEASE PREVENTION 1. List the risk factors for atherosclerotic cardiovascular disease 2. Given a patient database prescribe preventive measures to be taken to overcome reversible risk factors 3. Counsel patients on the advantages of exercise, smoking cessation, and prudent diet COMMUNICATION 1. Be able to communicate in a medically professional manner, both orally and in writing, to the patient, the family and with health care professionals. a. Present to the physician a brief synopsis of the patient’s present illness, pertinent positive and negative findings and the diagnostic and therapeutic regimen instituted. b. Communicate effectively with both patient and family by using a vocabulary familiar to all concerned. c. Counsel patient and family regarding the health problem including an explanation of the disease process, therapy and its rationale, therapeutic options, prognosis and health care services available. d. Write routine and all other admission orders by the problem number. e. Write in a SOAP format, clear concise and relevant progress notes including diagnostic, therapeutic and patient education plans. f. Fill out routine laboratory test and diagnostic procedure request forms Clinical Preceptor Manual *62 accurately and with pertinent data. g. Maintain a complete up-to-date problem list. h. Initiate requests for patient services including public health and home nursing, school testing and evaluation and release of medical records. i. Report communicable diseases utilizing appropriate forms and follow-up. j. Write interval notes. k. Perform discharge summaries. l. Give empathetic support to both patient and family in all communications. 2. Understand the roles of the various health care providers in performing primary screening for cardiovascular disease. 3. Communicate effectively the breadth and scope of services needed when consulting and/or referring a patient for cardiac consultation. Clinical Preceptor Manual *63 ROTATION OBJECTIVES DERMATOLOGY During the student’s rotation in dermatology exposure to some or all of the following subject matter will be provided. The student will gain experience and proficiency working as a member of an organized health care team. Emphasis should be placed on developing skills and cognitive knowledge that will help the student perform well in a primary care setting. Additional objectives to be attained by the student are as follows: BASIC SCIENCE 1. Describe the anatomy and components of the integumentary system 2. Describe the physiologic function of the integumentary system 3. Describe the physiologic and pathophysiological affects of UV radiation on the skin HISTORY 1. Elicit an appropriate complete dermatologic history a. elicit an appropriate dermatologic review of systems and medical review of systems that may lead the clinician to discover dermatologic manifestations of systemic disease b. elicit an appropriate dermatologic and systemic past medical history c. elicit an appropriate social and occupational history pertinent to dermatologic disease d. record the database acquired on the office or hospital record using the traditional or problem oriented format 2. Recognize classic historical presentations of primary dermatologic diseases and develop the ability to expand the database by exploring the following: a. risk factors b. exacerbating factors/conditions c. results of personal or medical attempts to treat the condition d. exposure to vocational or avocational skin irritants or common allergens e. use of personal hygiene products f. current or previous UV exposure PHYSICAL EXAMINATION 1. Describe a technique used for and the environment most conducive to performing an examination of the skin 2. Demonstrate the technique used for palpating the skin, hair and nails and list characteristics to be noted during this examination 3. Describe the normal and abnormal color characteristics of the skin and list common causes for abnormal findings 4. List commonly found nevi and describe characteristics that will help identify them 5. Describe various vascular lesions and list their etiology Clinical Preceptor Manual *64 6. List characteristics to observe when examining the skin including the following characteristics of skin, rashes, and/or lesions: a. color b. distribution c. type d. grouping or configuration e. edema f. temperature g. texture h. thickness i. mobility & turgor 7. List the most common types of primary skin lesions and describe their appearance 8. Describe the characteristics to be noted when inspecting and palpating the hair 9. Describe the common characteristics to be noted when inspecting and palpating the nails 10. List common normal and abnormal variations in the skin examination found in the newborn and children 11. List common normal and abnormal variations in the skin examination found in the elderly 12. List common non malignant skin abnormalities and be able to describe and recognize them 13. List common cutaneous malignancies and be able to recognize and describe them 14. List risk factors for Malignant Melanoma and other cutaneous neoplasms 15. List common nail pathologies and be able to identify them 16. List common hair pathologies and be able to identify them DIFFERENTIAL DIAGNOSIS 1. Differentiate between the following common dermatologic conditions: a. intradermal, junctional, hairy, halo, compound, and dysplastic nevi b. purpura, petechiae, spider angioma, and venous stars c. primary lesions such as macule, papule, patch, plaque, wheel, nodule, tumor, vesicle, bullae, & pustule d. secondary lesions such as scale, crust, lichenification, scar, keloid, excoriation, fissure, ulcer, erosion, atrophy 2. When presented with the following conditions develop a differential diagnosis, describe a diagnostic and therapeutic approach a. contact dermatitis b. dermatophyte, viral and bacterial infections of the skin, hair and nails c. infestations d. Lichen Planus e. urticaria f. verrucae g. molluscum contagiosum Clinical Preceptor Manual *65 h. sebaceous cysts i. seborrheic keratosis j. xerosis 3. When presented with a dermatitis differentiate between primary skin conditions and manifestations of systemic disease such as: a. xanthomas b. malar rash of systemic lupus erythematosus c. scarlatina d. erythema infectiosum e. Kaposi’s sarcoma f. septicemia(petechiae, etc) g. nail changes such as clubbing, spooning, Beau’s lines, splinter hemorrhages, etc DIAGNOSTIC 1. Describe the indications for, complications of, and technique to perform the following procedures a. punch biopsy b. excisional biopsy c. incisional biopsy d. skin scraping 2. Describe the indications for and perform the following diagnostic tests a. KOH prep b. Wood’s light examination c. Transillumination THERAPEUTIC 1. Describe a therapeutic approach to the conditions listed above 2. Describe the indications, contraindications and adverse reactions for prescribing common topical dermatologic agents 3. Describe the indications, contraindications, and adverse reactions to common oral agents used to treat dermatologic conditions including, but not limited to, antipruritics, corticosteroids, and antifungal agents HEALTH PROMOTION AND DISEASE PREVENTION 1. Counsel patients on the importance of protection from UV radiation exposure 2. Counsel patients on the importance of routine self skin examinations and indications for self referral for dermatologic care 3. Counsel patients regarding the risk factors and warning signs for skin cancer Clinical Preceptor Manual *66 COMMUNICATION 1. Be able to communicate in a medically professional manner, both orally and in writing, to the patient, the family and with health care professionals. a. Present to the physician a brief synopsis of the patient’s present illness, pertinent positive and negative findings and the diagnostic and therapeutic regimen instituted. b. Communicate effectively with both patient and family by using a vocabulary familiar to all concerned. c. Counsel patient and family regarding the health problem including an explanation of the disease process, therapy and its rationale, therapeutic options, prognosis and health care services available. d. Write routine and all other admission orders by the problem number. e. Write in a SOAP format, clear concise and relevant progress notes including diagnostic, therapeutic and patient education plans. f. Fill out routine laboratory test and diagnostic procedure request forms accurately and with pertinent data. g. Maintain a complete up-to-date problem list. h. Initiate requests for patient services including public health and home nursing, school testing and evaluation and release of medical records. i. Report communicable diseases utilizing appropriate forms and follow-up. j. Write interval notes. k. Perform discharge summaries. l. Give empathetic support to both patient and family in all communications. 2. Understand the roles of the various health care providers in performing primary screening for dermatologic disease. 3. Communicate effectively the breadth and scope of services needed when consulting and/or referring a patient for dermatologic consultation RESEARCH 1. Demonstrate an awareness of the recognized dermatologic literature, current issues and controversies in the literature and methods for accessing current medical literature while in rural sites Clinical Preceptor Manual *67 ROTATION OBJECTIVES ENT During the students rotation in ENT exposure to some or all of the following subject matter will be provided. The student will gain experience and proficiency working as a member of an organized health care team. Emphasis should be placed on developing skills and cognitive knowledge that will help the student perform well in a primary care setting. Additional objectives to be attained by the student are as follows: BASIC SCIENCE 1. Describe the anatomic components of the ear, nose, and throat 2. Describe the physiologic function of the ear, nose and throat 3. Describe common pathophysiological mechanisms involved in otolaryngology HISTORY 1. Elicit an appropriate complete history relative to common ENT problems 2. Record the database acquired on the office or hospital record using a traditional or problem oriented format 3. Recognize the classic historic presentations of disorders of the ear, nose or throat and further develop the database by exploring risk factors, vocational and avocational factors, and noise exposure PHYSICAL HISTORY 1. Perform and appropriate physical examination of the ear, nose, and throat 2. Recognize the multiple organ systems that may be responsible for common ENT complaints 3. Identify common normal and abnormal findings on physical examination of the ear nose and throat DIAGNOSTIC 1. Given a patient or historical, physical, and laboratory data, be able to diagnose and initiate treatment or appropriate referral for the following common problems: a. hearing loss b. sinusitis c. foreign body: (ear, nose, and throat) d. otitis externa e. otitis media f. perforated tympanic membrane g. pharyngitis/tonsillitis h. Meniere’s disease i. labyrinthitis j. epistaxis Clinical Preceptor Manual *68 k. rhinitis l. septal deviation m. nasal polyps 2. Know the indications, contraindications, and technique for performing the following: a. audiometry b. tympanograms c. radiologic evaluation including plain films and CT scans THERAPEUTIC 1. Perform, or assist the physician in performing, the following therapeutic procedures: a. cerumen removal b. sinus lavage c. otic wick insertion 2. Perform or assist in the following procedures developing an awareness of their indications, complications, appropriate equipment, and technique: a. surgical scrub b. donning of gown, gloves and mask c. proper draping of the patient d. proper application of wound dressings e. surgical closure 3. Participate in postoperative care by: a. ordering appropriate IV fluids b. maintaining appropriate IV fluids c. maintaining patient on appropriate diet d. administering wound care with special attention to drains and tubes e. monitoring patients with nasogastric catheters in place f. progressing patient’s ambulation at the appropriate times g. demonstrate measures to prevent post-operative thrombophlebitis/pulmonary emboli 4. List common complications of ENT surgeries and treatments for each complication 5. Describe the indications and contraindications as well as possible complications for the following surgical cases: a. tonsillectomy and/or adenoidectomy b. myringotomy with or without insertion tubes c. tympanoplasty HEALTH PROMOTION AND DISEASE PREVENTION 1. Counsel patients regarding the following primary preventive measures: a. appropriate use of hearing protection b. smoking cessation as a mechanism to decrease the incidence of respiratory disease and promote healthy living Clinical Preceptor Manual *69 COMMUNICATION 1. Be able to demonstrate both orally in writing a complete database in a concise, orderly fashion. 2. Develop an appreciation for the contribution of all health care providers in performing primary screening services for ENT disease and communicate effectively the breadth and scope of services needed when consulting and/or referring a patient for ENT problems. RESEARCH Demonstrate an awareness of the recognized ENT literature, current issues and controversies in the literature and methods for accessing current medical literature while in rural sites. Clinical Preceptor Manual *70 ROTATION OBJECTIVES ORTHOPEDICS During the student’s six-week elective rotation in orthopedics the PA student will develop an appreciation for the care of musculoskeletal diseases and trauma unique to the discipline. Emphasis shall be placed on the elements of this discipline essential to the practice of primary care. In addition to the requirements set forth in the segment general clinical goals and objectives the student will: HISTORY 1. Be able to elicit a first or second party history pertinent to care of the orthopedic patient developing skills in data base gathering and competence in common diagnosis. 2. Recognize that musculoskeletal problems rank sixth as a cause for all patient complaints and that 70% of musculoskeletal problems will be cared for by primary care providers and not orthopedists 3. Recognize the importance of discovering abuse or neglect as the etiology of musculoskeletal injuries during all ages of the lifespan. 4. Discover underlying risk factors for recurrent orthopedic injuries. PHYSICAL EXAMINATION 1. Demonstrate knowledge of musculoskeletal anatomy, pathology, and physiology applicable to the diagnosis, treatment, and prevention of musculoskeletal disease. 2. Develop proficiency in performing a musculoskeletal examination 3. Identify abnormal findings on the musculoskeletal examination 4. Record and/or present orally the data base in a concise, orderly, and accurate fashion. DIAGNOSTIC STUDIES 1. Identify, perform, or and/or interpret appropriate cost effective routine diagnostic procedures based on history and physical examination 2. Identify the appropriate and available diagnostic studies for a particular problem based on the history and physical examination. 3. Identify and describe the risks, costs, and patient inconvenience of various diagnostic studies DIFFERENTIAL DIAGNOSIS 1. Based on a given patient’s history, physical examination, or diagnostic studies develop a comprehensive differential diagnosis 2. When presented with the following symptoms develop a differential diagnosis and diagnostic impression consistent with the data base: a. Back Pain b. Oligo-articular joint pain Clinical Preceptor Manual *71 c. Polyarticular joint pain 3. When presented with a patient exhibiting symptoms consistent with the following disorders develop the ability to differentiate them from conditions that mimic their presentation: a. skeletal fractures/dislocations b. bursitis/tendonitis c. carpal tunnel syndrome d. sprains/strains e. low back pain/sciatica f. osteoarthritis g. crystalline arthropathies h. meniscal injuries i. rotator cuff injuries j. Reiter’s syndrome k. Chondromalacia l. Osgood-Slachter’s disease m. Legg-Cathe Perthe’s disease n. multiple myeloma o. scoliosis p. TMJ syndrome q. AC joint separation/dislocation r. Duputyren’s contracture 4. Given an x-ray film with good exposure and patient positioning identify the following: a. Normal anatomic landmarks b. Fractures c. Dislocations d. Osteoblastic/lytic lesions e. Abnormal calcifications f. Growth deformities g. Osteoarthritic changes THERAPEUTICS 1. Identify and initiate treatment for the following classifications of emergent conditions: a. Orthopedic Emergencies 1. infection 2. osteomyelitis 3. septic joints 4. slipped epiphysis 5. acute neurologic deficit b. Urgencies 1. congenital dislocated hip 2. club feet 3. tumors 4. acute bursitis Clinical Preceptor Manual *72 c. Trauma-life saving 1. cardiac and/or respiratory resuscitation 2. bladder trauma 3. bleeding 4. traumatic amputations d. Limb saving 1. spine injuries 2. open fractures 3. open dislocations 4. vascular occlusions 5. supracondylar fracture of the humerus in children 6. dislocated knee 7. neurovascular injuries 8. fractures 9. dislocations 2. Develop familiarity with the following techniques, common surgical procedures to include anatomic landmarks and common post-operative care and complications: a. Closed reductions b. Open reductions c. Skeletal traction d. Joint replacements e. Carpal tunnel release/neurolysis f. amputations including AK and BK g. Back surgery procedures to include microsurgery h. bracing i. prosthetic devices j. arthroscopic procedures 3. Perform or assist the following procedures knowing their indications, contraindications, complications, and appropriate equipment and techniques: a. Incision and drainage b. Wound débridement c. Joint aspiration/injection d. Closed management of simple fractures to including casting/splinting e. OR Protocol 1. surgical scrub 2. gowning and gloving 3. prepping the patient 4. proper draping of the patient 5. proper application of wound dressings f. Lacerations/surgical closure 1. cleansing and débridement of the wound 2. administration of local infiltrative anesthetics including hematoma and regional blocks 3. determine neurovascular involvement 4. suture lacerations 5. administer appropriate tetanus therapy Clinical Preceptor Manual *73 g. Participate in post operative care by: 1. ordering appropriate laboratory and diagnostic tests 2. ordering appropriate IV fluids 3. maintaining patient on correct diet 4. administering wound care with special attention being paid to drains and tubes 5. monitoring patients postoperatively for complications 6. progressing the patient’s activity at appropriate times 7. develop knowledge of the appropriate use of anticoagulant therapy 8. implement measures to reduce the risks of post operative embolic phenomena HEALTH PROMOTION AND DISEASE PREVENTION 1. Recognize, develop and implement effective strategies for incorporating health promotion and disease prevention as it relates to the discipline of orthopedics in primary care including: a. Prevention of osteoporosis b. Reducing risk of falls in the geriatric patient c. Prevention of sports related injury COMMUNICATION 1. Be able to communicate in a medically professional manner, both orally and in writing, to the patient, the family, and with health care professionals a. Communicate to the physician a brief synopsis of the patient’s present illness/condition b. Communicate effectively with both the patient and family using a vocabulary familiar to all concerned c. Counsel the patient and family regarding the health problem including an explanation of the disease process, therapy and its rationale, therapeutic options, prognosis, and health care services available d. Write routine and all other admission orders e. Write in a SOAP format, clear concise and relevant progress notes f. Maintain a complete and up to date progress list g. Write interval notes h. Perform discharge summaries i. Give empathetic support to both patient and family in all communications Clinical Preceptor Manual *74 RESEARCH 1. Demonstrate an awareness of the recognized Orthopedic literature, current issues and controversies in the literature and methods of accessing current literature while in rural sites. ATTITUDE 1. Demonstrate an understanding of the effects of illness and injury on the patient, family and community 2. Demonstrate an understanding of minor problems and those which require intense therapy and treatment 3. Demonstrate an awareness of the implication of drug and alcohol use/abuse in the orthopedic patient 4. Demonstrate an awareness for the respect of legal rights of patients including confidentiality Clinical Preceptor Manual *75 ROTATION OBJECTIVES PSYCHIATRY During the student’s six-week rotation in psychiatry exposure to some or all of the following subject matter will be provided. The student will gain experience and proficiency working as a member of an organized health care team working in psychiatry. Emphasis should be placed on developing those skills and cognitive knowledge that will help the student perform well in a primary care setting. Additional objectives to be attained by the student are as follows: HISTORY 1. Elicit an appropriate complete psychiatric a. history and medical review of systems that may present as psychiatric disease b. past medical history c. risk factors profile d. database stressing the cognitive and affective information and develop skills which will enable recognition of normal and deviation from normal 2. Record the database acquired on the office or hospital record using the traditional or problem oriented medical record system PHYSICAL EXAMINATION 1. 2. 3. 4. Perform a directed physical examination on the patient with suspected psychiatric disease. Perform and interpret the results of a complete mental status examination including: a. appearance and behavior b. thought process and perceptions 1. coherency and relevance 2. thought content 3. perception c. cognitive factors 1. orientation 2. attention and concentration 3. memory 4. information and vocabulary 5. abstract reasoning 6. judgment 7. perception and coordination d. evaluation of suicidal risks Identify abnormal findings on the physical examination that may lead the clinician to consider a secondary cause for the psychiatric manifestation of the patient. Record the physical examination on the office or hospital record using the traditional or problem oriented medical record. Clinical Preceptor Manual *76 DIAGNOSTIC 1. Given the database collected: a. develop a problem list and tentative diagnosis b. develop a plan of investigation and order appropriate laboratory and diagnostic tests c. understand and apply the current method of diagnostic criteria for psychiatric disorders 2. Identify and be able to discuss the indication for performing standardized psychiatric screening, and other examinations: a. EEG b. Brain Scan c. Cat Scan d. intelligence tests (Wechsler Adult Intelligence scale) e. tests of perceptual and motor function (Bender Gestalts) f. personality inventories (MMPI) g. projective tests (Rorschach, Thematic Apperception Test) h. Denver Developmental Screening Test DIFFERENTIAL DIAGNOSIS 1. List the criteria, clinical features, differential diagnosis, and treatment of the following psychiatric and associated disorders. a. affective disorders 1. bipolar disorder 2. cyclothymic disorder 3. dysthymic disorder b. anxiety disorders 1. phobic disorders 2. anxiety states 3. post traumatic stress disorder c. somatoform disorders 1. somatization disorder 2. conversion disorder 3. psychogenic pain disorder 4. hypochondriasis d. psychosexual dysfunction e. adjustment disorders f. pediatric disorders 1. mental retardation 2. attention deficit disorder 3. conduct disorder 4. anxiety disorder 5. eating disorders: anorexia nervosa/bulimia g. organic mental disorder h. substance abuse disorders Clinical Preceptor Manual *77 i. j. k. l. schizophrenic disorders paranoid disorders brief reactive psychosis personality disorders 1. paranoid 2. schizoid 3. schizotypal 4. histrionic 5. narcissistic 6. antisocial 7. borderline 8. avoidant 9. dependent 10. compulsive 11. passive-aggressive m. other conditions 1. malingering 2. uncomplicated bereavement 3. marital problems 4. parent child problems n. autism o. stress related medical disorders THERAPEUTICS 1. Understand the treatment modalities listed including indications, contraindications, and side effects of: a. psychotherapy b. electroconvulsive therapy c. neurosurgical approaches d. hospitalizations e. social approaches f. common psychiatric pharmacologic agents including: 1. minor tranquilizers 2. major tranquilizers 3. sedative hypnotics 4. phenothiazine derivatives 5. antidepressants Clinical Preceptor Manual *78 HEALTH PROMOTION AND DISEASE PREVENTION 1. Know and counsel the psychiatric patient about the current recommendations regarding: a. importance of medication compliance to maintain disease control b. importance of non pharmacologic mechanisms in prevention of stress mediated psychiatric disease c. availability of community based psychiatric services EMERGENCY SKILLS 1. List the indications for immediate psychiatric referral and evaluation by a psychiatrist 2. List the indications for involuntary commitment of the psychiatric patient 3. List the indications, contraindications, and adverse reactions of commonly used psychotropic drugs in an emergency setting COMMUNICATION 1. Be able to present both orally and in writing a complete database in a concise and orderly fashion 2. Develop an appreciation for the contribution of other health care providers in evaluating, managing and treating psychiatric disease and communicate effectively the breadth and scope of services needed when referring a psychiatric patient RESEARCH 1. Demonstrate an awareness of the recognized psychiatric literature, current issues and controversies in the literature and methods of accessing current literature while in rural sites. ATTITUDE 1. Demonstrate an understanding of the range of psychiatric disease showing sensitivity to its variable expression among individuals and various cultural and social groups. Clinical Preceptor Manual *79 ROTATION OBJECTIVES EMERGENCY MEDICINE 1. Develop an awareness of: a. The need for methodical, rapid, and accurate assessment of the acutely ill or injured patient is the primary concern of the emergency department. b. Patient anxiety and apprehension during times of crisis and the need for empathy, confidence, and appropriate reassurance that should be exhibited by the student c. The need to inform and educate the patient’s family regarding the current emergent condition and progress. 2. General Objectives: a. Elicit an appropriate complete or partial history from the patient or “third” party should the patient be unconscious or a child. b. Perform a methodical, rapid, comprehensive, and accurate immediate assessment of patients presenting to the emergency department with life threatening emergencies. c. Perform a methodical, rapid, comprehensive, and accurate secondary assessment of patients presenting to the emergency department, being careful to examine for the following: 1. Vital signs, facial and extremity coloration 2. Head 3. Chest 4. Abdomen 5. Extremities 6. Pelvis 7. Perineum 8. Back and Buttocks d. Given a patient presentation either historical, physical, or laboratory based: 1. Develop a problem list and tentative diagnosis 2. Develop a plan of investigation and order the appropriate laboratory and diagnostic tests 3. Develop a plan of therapy appropriate for the patients condition e. Record the data base on the emergency room record using both traditional and problem oriented medical record approach. f. Present orally the complete database in a concise and orderly fashion 3. Specific Objectives a. Given a patient or appropriate historical, physical or laboratory data, be able to diagnose and initiate treatment for the following common conditions seen in the emergency department 1. Fractures and dislocations 2. Deteriorating or changing mental status 3. Penetrating ocular injuries Clinical Preceptor Manual *80 4. Acute endocrine emergencies(diabetic coma, adrenal insufficiency, thyroid storm, etc) 5. Chest Pain (Angina/MI) 6. Abdominal Pain, (Appendicitis, Cholecystitis, Bowel Obstruction, Perforated Ulcer, Renal Colic, etc) 7. Ingestion of Poisons etc 8. Drug Overdose/Abuse 9. First, Second, or Third degree thermal, chemical, or electrical burns 10. Hypertensive Emergency/Urgency 11. Acute arterial occlusion 12. Intrapartum Hemorrhage 13. Threatened/Spontaneous AB 14. Precipitous delivery 15. Seizures 16. Severe Dehydration 17. Shock 18. Arrhythmias/Cardiac Arrest 19. Congestive Heart Failure/Pulmonary Edema 20. Acute Respiratory Distress Syndrome/ Respiratory Arrest b. Identify indications and complications of ACLS and perform Advanced Life support on 1. Newborn 2. Young Child 3. Adult c. Identify the presentation of and describe appropriate therapy for harmful bites from: 1. Humans 2. Snakes (Hemotoxic and Neurotoxic Venom) 3. Spiders 4. Animals 5. Insects d. Identify and initiate treatment for the following common conditions seen in the emergency room 1. Allergic 12. Glomerulonephritis Reactions/Anaphylaxis 13. Otitis Media 2. Lacerations/abrasions 14. Tonsillitis 3. Puncture/Stab wounds 15. Epistaxis/emoptysis 4. Cellulitis 16. Conjunctivitis 5. Rashes 17. URIs 6. Hematoma 18. Pneumonia 7. Herpes Zoster 19. Otitis Externa 8. Pharyngitis 20. Exac COPD 9. Headache 21. CVA 10. Sinusitis 22. Gastroenteritis 11. Pyelonephritis 23. Gastritis Clinical Preceptor Manual *81 24. Hepatitis 33. Back Pain 25. Hiatal Hernia/GERD 34. Muscle Spasm 26. Peptic Ulcer Disease 35. Costal Chondritis 27. UTI 36. Acute Anxiety 28. STDs 37. Depression 29. Kidney Stones 38. Alcohol Abuse 30. Vaginitis 39. Gunshot wounds 31. PID 40. Syncope 32. Sprains/Strains e. Perform the following procedures 1. Initiate IV Therapy using Intracath, Jelco, or butterfly 2. Insert and remove a central line under supervision 3. Insert and remove a nasogastric tube 4. Perform gastric lavage 5. Insert and remove a urinary bladder catheter 6. Obtain bacteriologic, viral, fungal cultures f. Perform and or interpret the following laboratory procedures 1. Venipuncture for CBC, Lytes, SMA-12, and Blood Cultures 2. Arteriopuncture for ABG’s 3. Micro-hematocrit 4. Urinalysis including microscopic examination 5. feces, urine, sputum, gastric contents for occult blood 6. 12 lead EKG g. For each of the following procedures identify 1. Indications, contraindications, and complications 2. Appropriate equipment to be used 3. Appropriate technique to be used 4. Perform, or assist in performing, under appropriate supervision a. defibrillation b. chest tube insertion c. venous cutdown d. thoracentesis e. paracentesis f. lumbar puncture g. joint aspiration h. tracheostomy i. cast application j. endotracheal intubation h. Perform the following clinical procedures for lacerations under responsible physician supervision. 1. cleansing and débridement of wounds 2. administration of local infiltrative anesthesia, or digital blocks as appropriate 3. determination of major vessel, nerve, or tendon involvement 4. suturing of the laceration in the absence of the above conditions Clinical Preceptor Manual *82 5. assisting the physician in repair of the above conditions 6. administer appropriate tetanus therapy i. Given a patient or simulated model demonstrate the following principles of splinting including the use of 1. Rigid Splints 2. Air Splints 3. Traction Splints 4. Apply Slings 5. Proper application of ACE wrap j. Given AP/Lateral View of any bone in the skeleton identify the following 1. Fractures 2. Dislocations 3. Osteolytic and Osteoblastic Lesions 4. Osteoporosis 5. Degenerative changes k. Given a flat plate and upright of the abdomen x-ray with good exposure and patient positioning, identify the following: 1. Free intraperitoneal air 2. Air/Fluid levels within the bowel 3. Intra-abdominal calcification 4. Hepatic and splenic margins 5. Psoas shadows 6. Non specific Abdomen 7. Dilated Intestine l. Given a PA and Lateral Chest x-ray with good exposure and patient positioning, identify the following 1. Pulmonary Infiltrates 2. Pulmonary Nodules 3. Atelectasis 4. Cardiomegaly 5. Rib Fractures 6. Widened Mediastinum 7. Pleural Effusions 8. Normal Chest X-ray Clinical Preceptor Manual *83 ROTATION OBJECTIVES CORRECTIONS MEDICINE 1. Be able to identify and define the following relationships and concepts inherent to the corrections setting. a. Care, custody and control of the inmates b. Medical and correction staff interaction c. Medical staff and inmates relationship d. Medical staff and Psychiatric/Psychological staff interdependence e. Staff/inmate abuse issues f. Deliberate indifference g. Malpractice issues h. Civil rights issues 2. Approach a patient of any age in the corrections setting and: a. Acquire partial or complete historical data pertinent to the patient’s presenting complaint b. Perform a partial or complete physical examination appropriate to the patients presenting complaint c. Synthesize the data obtained into a current problem list d. Address and prioritize the following: 1. the patient’s purpose for presenting to their primary care provider 2. significant findings identified at the time of their visit 3. maintenance of chronic disease states, and health promotion and disease prevention issues. 3. Develop a differential diagnosis of acute presenting complaints based on historical and physical findings. 4. Order appropriate laboratory and/or diagnostic tests to confirm, or rule out preliminary diagnostic impressions. 5. Present data gathered to the supervising physician in an organized and logical manner. 6. Develop a patient management plan based on data gathered. 7. Provide necessary patient education to assure understanding and compliance with treatment regimen. 8. Arrange timely and appropriate patient follow up or referral. 9. Develop an approach, based on location and nature of a given encounter to the following: a. Initial Workups - encounter characterized by initial assessment and management of clinical problems b. Continued Care - encounter characterized by management of a previously diagnosed condition or health maintenance visit c. Emergency Care - encounter characterized by prompt assessment and management of life threatening conditions d. Perform the following evaluative tasks: Clinical Preceptor Manual *84 1. 2. 3. 4. History taking and performance of physical examinations Perform and /or order appropriate laboratory and diagnostic studies Formulation of differential diagnosis Evaluation of the patient’s presenting problem 10. Management of the patient including health maintenance and disease prevention, appropriate clinical intervention, employment of appropriate clinical therapeutics, and awareness of legal and ethical considerations. 11. Apply scientific concepts focusing on physiologic or disease processes 12. Describe presentations and management of the most common diseases encountered in correctional settings, with particular emphasis placed on epidemiology, natural history, historical and physical manifestations, management, and prevention, within the following categories: a. b. c. d. e. f. g. h. i. j. k. l. m. n. o. Disease /Disorders of the Central Nervous System Disease/Disorders of the Sensory Organs Disease/Disorders of the Respiratory System Disease/Disorders of the Circulatory System Disease/Disorders of the Digestive System Behavioral/Emotional disorders Disease/Disorders of the Musculoskeletal System Disease/Disorders of the Skin/Subcutaneous Tissue Disease/Disorders of the Endocrine/Nutrition/Metabolism/Immune System Disease/Disorders of the Kidneys/Urinary Tract Diseases/Disorder of the Male/Female Reproductive System Disease/Disorders of the Blood/Blood-Forming Organs Infectious/Parasitic Diseases Injuries/Wounds/Toxic Effects/Burns Health Maintenance 13. Presentations of Ill Defined Symptom Complexes Clinical Preceptor Manual *85 TOPICS LIST - ADULT MEDICINE CARDIOLOGY Cardiac Risk Factors Coronary Artery Disease Angina/Myocardial Infarction Arterial Disease - Aneurysm/Occlusion Venous Disease - Thrombosis/Insufficiency Valvular Heart Disease Murmurs/Endocarditis Hypertension Cardiac Rehabilitation Pericarditis Congestive Heart Failure Arrhythmias PULMONARY MEDICINE Chronic Obstructive Pulmonary Disease: Asthma, Chronic Bronchitis, Emphysema Infection: Pneumonia/AcuteBronchitis/Pleuritis Adult Respiratory Distress Syndrome (ARDS) Neoplasms Pulmonary Function Testing/Arterial Blood Gasses Pulmonary Embolism/Pneumothorax/Hemothorax Pulmonary Rehabilitation Pulmonary Edema/Hypertension NEPHROLOGY/UROLOGY Acid Base and Electrolyte Balance Urinary Tract Infection/Pyelonephritis Glomerulonephritis/Nephrotic Syndrome Acute Renal Failure Chronic Renal Failure/Dialysis Nephrolithiasis Prostatitis/Epididymitis/Male STD’s Nephrotoxins GASTROENTEROLOGY Esophageal Reflux, Spasm, Stricture Peptic Ulcer Disease/Gastritis Pancreatitis Malabsorption Ulcerative Colitis Crohn’s Disease - Regional Enteritis Diverticular Disease Hemorrhoids/Fissures/Fistulas Neoplasms of GI System Hepatitis: Infectious/Non-Infectious Jaundice Alcoholic Liver Disease Cholecystitis/Cholelithiasis/Cholangitis Diarrhea/Constipation Infections: Viral, Bacteria, Parasitic Spastic/Irritable Colon-Irritable Bowel Syndrome NEUROLOGY - Seizure Disorders Headaches Infection: Meningitis, Encephalitis Cerebrovascular disease: TIA, CVA Multiple Sclerosis Tremors/Parkinsonisms Neuropathies: Cranial Nerves, Peripheral Disc Disease: Trauma, Osteoporosis Coma/Trauma of CNS Clinical Preceptor Manual *86 RHEUMATOLOGY Osteoarthritis Rheumatoid Arthritis Gout/Pseudogout Infectious Arthritis Spondyloarthropathies Collagen Vascular Diseases ENDOCRINOLOGY Diabetes Mellitus/IDDM-NIDDM Hypoglycemia Hyperlipidemia Adrenal Suppression Secondary to Steroid Use Thyroid Disease: Hyperthyroidism, Hypothyroidism, Thyroiditis, Nodules DERMATOLOGY Allergic/Contact Dermatitis Acne Skin Tumors Infection: Viral, Bacteria, Parasitic, Fungal Psoriasis Eczema IMMUNOLOGY Anemias Bleeding Disorders Leukemias Lymphomas/Hodgkins Immune Deficiencies ALLERGY Anaphylaxis Hypersensitivity OPHTHALMOLOGY Conjunctivitis/Red Eye Cataracts Glaucoma Corneal Abrasion Retinal Changes Secondary to Systemic Disease (Hypertension, Diabetes Mellitus) ENT Vertigo Infections: Viral, Bacterial Allergic Rhinitis/Sinusitis Clinical Preceptor Manual *87 TOPICS LIST - GERIATRICS GENERAL Biological Process of Aging Infectious Disease of Elderly Alcoholism Dementia/Depression/Suicide Pharmacology in the Elderly Human Sexuality Death and Dying Problems of Institutionalization Elder Abuse Home Health Care Nutrition Community Senior Citizen Resources SYSTEMS HEENT Glaucoma/Cataracts/Presbyopia Loss of Hearing/Sense of Taste Dental Problems Cardiovascular Hypertension CAD-ASCVD Arrhythmias Syncope Thrombophlebitis Arterial Occlusion Respiratory COPD: Asthma/Chronic Bronchitis/ Emphysema Pneumonia/Bronchitis Cancer Gastrointestinal Constipation Hiatal Hernia/Reflux PUD/Gastritis Cancer: Esophagus, Stomach, Colon Malabsorption Diverticular Disease Appendicitis Cholelithiasis Intestinal Obstruction Genitourinary Incontinence Urinary Tract Infections Acute/Chronic Renal Failure (Male) Prostatic/Testicular Tumors/Impotence/Hernias (Female) Atrophic Vaginitis/Uterine Prolapse/Tumors: Breast Uterus, Vulva Musculoskeletal Osteoarthritis Osteoporosis Paget’s Disease Stress Fractures/Hip Fractures Clinical Preceptor Manual *88 Endocrine Diabetes/Hypoglycemia Thyroid Disorders Obesity Hematology Anemia Leukemia Neoplasms Prostate Breast Lung Colon Skin Keratoses Skin Cancers Dermatitis: Contact, Seborrheic, Dry Skin Fungal Infections Pigmentary Changes Decubitus Ulcers Neurology Cerebrovascular Disease Falls/TIA’s Tremors/Parkinsonism Dementia/Alzheimer’s Disease Clinical Preceptor Manual *89 TOPICS LIST - MENTAL HEALTH Neurotic Disorders Psychiatric Emergencies Depression Sleep Disorders Bipolar Disorder Post-Traumatic Stress Syndrome Schizophrenic Disorders Anxiety Paranoid Disorders Somatoform Disorders Affective Disorders Personality Disorders Dementia Child Psychiatry Childhood Developmental Disorders Substance Abuse and Dependence Mental Retardation Clinical Preceptor Manual *90 TOPICS LIST - OBSTETRICS & GYNECOLOGY GYNECOLOGY Menstruation Menopause/Osteoporosis Contraception Dysfunctional Uterine Bleeding Premenstrual Syndrome High Risk Pregnancy Infertility Vaginitis/STD’s/PID Endometriosis Breast Disease Benign/Malignant Lesions of the Reproductive Tract Sexual Dysfunction/Counseling Gynecological Surgery/Laparoscopy Ultrasonography/Colposcopy Amenorrhea Genetic Counseling OBSTETRICS Fetal Development/Fetal Prenatal Exam/care Labor and Delivery High Risk Pregnancy Toxemia of Pregnancy Medical Complications of Pregnancy Obstetrical Anesthesia Post-Partum Care Abruptio Placenta/Placenta Previa Ectopic Pregnancy Abortion Intrauterine Death Cesarean Section Genetic Counseling/Amniocentesis Ultrasonography/Fetal Monitoring/Fetal Activity Testing Clinical Preceptor Manual *91 TOPICS LIST - PEDIATRICS GENERAL Newborn Exam Problems in the Neonate Well Baby/Well Child Exams Immunizations Growth and Development Failure to Thrive Fever of Unknown Origin Fluids and Electrolytes/Acid-Base Communicable Diseases Poisonings Learning Disabilities/Mental Retardation Genetic Disorders/Counseling Adolescent Medicine Child Abuse Depression/Suicide in Teenagers SYSTEMS Cardiology Congenital Heart Disorders Respiratory URI including Otitis Media, Otitis Externa, Pharyngitis, Croup Epiglottis Bronchitis/Bronchiolitis Respiratory Distress Syndrome Pneumonia Asthma Cystic Fibrosis Gastrointestinal Infection: Bacterial, Viral, Parasitic Diarrhea/Dehydration Constipation Hyperbilirubinemia Congenital Malformations Genitourinary Urinary Tract Infections Vaginitis Orthopedics Common Fractures Congenital Abnormalities Hematology Anemia Childhood Leukemias Endocrinology Diabetes Clinical Preceptor Manual *92 Neurology Meningitis Encephalitis Seizure Disorders Skin Viral Exanthems Contact Dermatitis Eczema Parasitic Infections Impetigo Tinea/Monilial Infections Acne Miliaria Allergic Dermatitis Clinical Preceptor Manual *93 TOPICS LIST - SURGERY GENERAL Pre/Post Operative Care Wound Care and Infections Anesthesia Aseptic Techniques Principals of Suturing Fluid and Electrolytes/Acid-base Surgical Nutrition/Hyperalimentation Shock Trauma Care Burns Organ Transplantation SYSTEMS Breast Tumors/Reconstruction Cardiovascular By-Pass Grafting Aneurysms Valve Replacements Venous Ligation Arterial Reconstruction Thorax Lung Biopsy/Resection Abdomen Acute Surgical Abdomen Appendectomy Bowel Resection Cholecystectomy Liver Biopsy Clinical Preceptor Manual *94 Urology Herniorrhaphy Prostatic/Testicular Tumors/Testicular Torsion Nephrolithiasis TURP-BPH Orthopedics Arthroscopy/Arthroplasty Common Knee Injuries Common Shoulder Injuries Hand Injuries Sprains/Strains Neurosurgery Lower Back Problems Cervical Disc Disease Long Term Care Objectives All LHUP PA students will obtain clinical experiences in long term care settings. These experiences begin during the first year of the program whereby students spend on day during the didactic year completing an assessment of a long term care patient, including: Attain a history and comprehensive physical examination Review and make suggested changes to a long term care plan based on current standards of care Assessing polypharmacy issues and other common areas whereby medical errors occur and making recommended changes Develop a health maintenance and disease prevention plan Students are also required to obtain exposure to long term care facilities throughout the clinical year. All experiences in long term care must be logged into the LHUP PA Program web portal. Clinical Preceptor Manual *95 BASIC SCIENCE 1. Upon written, oral, or practical examination the PA student will: a. Describe normal human aging, age-related changes in tissues, organs and physiologic function, and homeostasis. b. Describe age-related changes in epidemiology of diseases, presentation of illnesses, response to therapy, pharmacokinetics and pharmacodynamics. c. Discuss Principles of biomedical ethics, including an understanding of decision-making capacity, competence, and autonomy. d. Describe nutritional needs of older persons, including recognition and treatment of malnutrition. e. List age specific health promotion, disease prevention screening assessments that should be completed HISTORY 1. Be able to elicit and record an appropriate first or second person history from a geriatric patient and further: a. Make appropriate adjustments necessary in history taking and physical examination. b. Describe the elements and conduct of Comprehensive Geriatric Assessment. c. Elicit detailed history regarding dietary habits, sleep patterns behavior changes use of medications (prescription or OTC), drugs or alcohol. d. Elicit history of hearing or visual disturbances e. Elicit information regarding patient’s home environment, support network and financial status. f. Appropriately utilize a second party to augment information obtained from a patient. g. Demonstrate awareness that the process of aging alters both the historical and physical manifestations of certain diseases. h. Demonstrate awareness that geriatric patients may underreport illness. Clinical Preceptor Manual *96 PHYSICAL EXAMINATION 1. Perform a physical examination on the adult or geriatric patient allowing for: a. Variations in physical findings among the elderly population. b. Common normal physical findings in the geriatric population. c. Abnormal physical findings that are found with increased frequency in this population. DIAGNOSTIC STUDIES Order and interpret cost effective, appropriate diagnostic testing in the geriatric patient considering: 1. Age related changes in lab values 2. Changes in the range of normal that may occur as a result of the aging process DIFFERENTIAL DIAGNOSIS 1. Develop a differential diagnosis and diagnostic impression for the following diseases commonly seen in geriatric patients in long term care facilities: a. Cognitive impairment/dementia b. Depression c. Incontinence (urinary and fecal) d. Gait and balance disorders e. Immobility f. Pressure ulcers g. Sensory impairment h. Pain i. Falls j. Delirium 2. Compare and contrast the difference in incidence, natural history, presentation management, and outcomes of medical problems when they occur in elderly persons. Clinical Preceptor Manual *97 THERAPEUTICS 1. Identify, perform and/or order appropriate, cost-effective, routine therapeutic procedures and be able to assist the physician with other therapeutic procedures. a. administer intravenous infusions utilizing appropriate equipment including butterfly needle, intravenous catheter, heparin lock and infusion pumps. b. calculate infusion rate. c. administer injections by a variety of routes including intradermal, subcutaneous, intramuscular and intravenous. d. be familiar with normal nutritional requirements of the elderly. e. be familiar with dietary treatment of health problems including hypertensive, diabetic, low fat, low cholesterol and low sodium diets. f. be familiar with the drugs used most frequently in treatment or health problems including basic modes of action, indications, contraindications and complications as well as the role of polypharmacy as it relates to the elderly.. g. be familiar with the management of common medical problems. HEALTH PROMOTION/DISEASE PREVENTION 1. Describe the nutritional needs of older persons, including recognition and treatment of malnutrition. 2. Describe age specific health promotion and disease prevention strategies. 3. Describe risks and benefits of surgical interventions, pre-operative evaluations and post-operative care in the geriatric population. 4. Compare and contrast the organization and financing of health care for older persons. 5. Discuss the principles of fitness, exercise and rehabilitation as applied to older people. EMERGENCY SKILLS 1. Demonstrate the ability to recognize and manage life-threatening emergencies jointly with, and in the absence of, the physician. a. Recognize signs and symptoms of common emergencies in geriatric patients and take appropriate action to sustain life when appropriate. b. Recognize common causes of altered mental status in the geriatric population and treatment. Clinical Preceptor Manual *98 c. Describe the use of and indications for standard emergency medications and administer if appropriate to geriatric patients d. Respect the decision of the patient and/or family for no advanced life support procedures COMMUNICATION 1. Be able to communicate in a medically professional manner, both orally and in writing, to the patient, the family and with health care professionals. a. Present to the physician a brief synopsis of the patient’s present illness, pertinent positive and negative findings and the diagnostic and therapeutic regimen instituted. b. Communicate effectively with both patient and family by using a vocabulary familiar to all concerned. c. Counsel patient and family regarding the health problem including an explanation of the disease process, therapy and its rationale, therapeutic options, prognosis and health care services available. d. Write routine and all other admission orders by the problem number. e. Write in a SOAP format, clear concise and relevant progress notes including diagnostic, therapeutic and patient education plans. f. Maintain a complete up-to-date problem list. g. Give empathetic support to both patient and family in all communications including end of life issues and decisions. RESEARCH 2. Demonstrate an awareness of the recognized geriatric literature, current issues and controversies in the literature and methods of accessing current literature while in rural sites. ATTITUDE A. Demonstrate an awareness of the various myths and stereotypes related to older people. B Discuss how ageism, like racism, affects all levels and aspects of society including health professions and can adversely affect optimal care of elderly patients. C. Describe the heterogeneity of older persons--a diverse group with different personalities, different values, different functional levels, and different medical illnesses. The need for PA students to view geriatric patients as individuals regardless of chronological age and to be cared for in a unique fashion. D. Demonstrate Openness, willingness and necessity to work with other disciplines in caring for older patients. Clinical Preceptor Manual *99 E. Demonstrate self-awareness of the students’ personal attitudes towards their own aging, disability, and death. F. Demonstrate compassion and understanding attitude on the part of the PA student for care givers of the frail elderly and the difficulties they face. G. Demonstrate an appreciation of the need for improving and optimizing function for older people, rather than just focusing on diseases. H. Describe how maintenance of function and quality of life are more often goals of care than cures of disease Clinical Preceptor Manual *100 Section Four: GENERAL REQUIREMENTS FOR CLINICAL YEAR Clinical Preceptor Manual *101 GENERAL REQUIREMENTS FOR THE CLINICAL YEAR 1. Communication A. General It is important that students maintain contact with the program throughout their clinical rotations. B. E-mail Students are required to maintain a current Lock Haven University email address and internet access while on all clinical rotations at all times. At a minimum, students will check email at least every other day and it is recommended that email be reviewed daily. Remember, local libraries and sister PASSHE System Universities can provide computer/internet access when not available at your site. Failure to maintain a current LHUP email account may prevent students from acquiring critical information during the clinical year. Students will be responsible for all correspondence sent to their LHUP account. Failure to maintain email communication on a regular basis may result in failure of the rotation. Students are advised to maintain copies of all email correspondence to their faculty advisor and other program correspondence to assist them in settling disputes over grades. Failure to produce copies of emails that were allegedly sent will diminish chances for the student to be successful in resolving grade disputes. C. Phone Calls If you wish to contact the Physician Assistant Program, the telephone number is 570-484-2929. You may call this number 24 hours a day and leave voice mail messages so that your call can be returned. Be sure to leave your name and a time that will be most appropriate to return your call. You may also call your faculty advisor at their contact number and leave a message any time. D. Conference Phone Calls Conference calls may be scheduled with each student periodically and at the direction of the Clinical Coordinator. E. Student Site Visitations A PA program faculty member will visit at least twice during your clinical year. Additional site visits will be scheduled on an as-needed basis. Faculty Advisors Students will be assigned a faculty advisor during the clinical year. The assignments of faculty advisors are made by the PA program. If a student has concerns regarding their assigned faculty advisor, they should first attempt to Clinical Preceptor Manual *102 resolve the issue with the faculty member. If the issue cannot be resolved directly with the faculty member, the student may petition the PA Program Director for a change of faculty advisor. Students will maintain communication with their faculty advisor by regularly turning in scheduled assignments, journals, e-mail or by phone if they feel they are having urgent issues on their rotation. 2. Work Hours, Meetings & Attendance A. Rotation Work Hours Students are expected to exhibit an exemplary work ethic by maximizing their time at the clinical site in which they are assigned. This includes after hours clinic assignments, on call time, rotating shifts, hospital rounds as required, and any other clinical opportunities that may present themselves during the course of the clinical experience. Students are required to log a minimum of 40 clinical hours per week during the clinical experience. Not maximizing clinical opportunities may result in grade reduction at the discretion of the faculty advisor. These hours need to be accurately listed on the schedule you will turn in on your first assignment of a “post card” (explained below). Likewise, your journal will also reflect the hours you work each day. B. Work Settings Students are required to obtain experiences in emergency, ambulatory, long term care, and inpatient settings during their educational experience. These experiences can be obtained in a variety of ways including making rounds in hospitals or nursing homes, seeing patients in an emergency room or caring for emergencies in clinics equipped to do so. These settings are listed on your student log page on the web. Be sure to indicate all settings in which you have had experiences during your clinical training. Long term care, prenatal care and emergency medicine experiences must include the dates and locations of these experiences in the appropriate fields in the student log page and documented in the student’s weekly journal. Failure to provide this information will preclude the student from meeting the minimum requirements for graduation. Falsification of log information represents grounds for immediate dismissal from the program. We will monitor your logs closely and if you have not attained these experiences we will be required to adjust your future clinical experiences accordingly to assure you have experienced a wide variety of clinical settings. If you are uncertain as to how to classify settings contact your faculty advisor. Clinical Preceptor Manual *103 C. PA Days Students are required to attend all PA day activities at the end of each clinical experience. PA days start at 7:45 AM and end at 4 PM each day. At the end of Clinical Rotations II you will be on the LHU Main campus for one week for a Board Review Course. Students are required to be on campus for a week during the preceptorship experience for summative testing. Do not make any travel plans during these times. Upon returning to campus for PA days you are required to provide the following paperwork: 1. Original preceptor evaluation. 2. Preceptor grading sheet and attached write-ups for that clinical experience. 3. Students are required to hand carry, or make arrangements for the preceptor evaluations to be sent to the PA Program by PA days. Ultimately, it is the student’s responsibility to insure that their preceptor evaluation is received by the program Prior to taking your end of clinical experience exam you will be required to fill out your student critique for the clinical experience you just completed. You will not be able to take your exam if you haven’t completed this critique. D. Attendance & Punctuality Students must report to their clinical experience site as per the agreed weekly schedule sent via your first week “post card” assignment. Any absence from your clinical site due to illness must be reported to your faculty advisor and the clinical coordinator. Absence of two or more days will require a physician’s excuse. Any absence for personal reasons, including job interviews, must be approved in advance by your faculty advisor and the clinical coordinator. Punctuality is expected for all meetings, work days, and PA day activities. E. Professional Behavior Students are required to uphold the highest level of professional demeanor at all times. Failure to abide by the PA Program policies set forth in the student manual, or the PA Profession Code of Ethics, recurrent unexcused absences, failure to submit assignments in a timely fashion, dishonesty, failure to respond to emails, or unprofessional behavior will result in a reduction of your overall grade for the rotation at the discretion of the faculty advisor. Repeated violations after a verbal warning and written contract will result in dismissal from the program. Clinical Preceptor Manual *104 CLINICAL ROTATIONS I, II, III ASSIGNMENTS & GRADING Following are tables showing assignments & grading for Clinical Rotations I through III. All assignments are mandatory and failure to produce them will result in failing that rotation. All assignments must be uploaded into the PA Program Portal by midnight Sunday of the fourth week for each clinical experience. A detailed explanation of each type of assignment follows at the end of this section. Students are required to complete an online evaluation of all their clinical sites. Failure to complete the evaluation will result in a grade of incomplete for the rotation. Incomplete grades convert to failing grades at the midpoint of the following semester per University policy. Clinical Rotations I and II Assignments for each clinical experience. Due by Week 1 Week 2 Week 3 4 Week Week 5 Week 6 Journal 1 Journal 2 Journal 3 Journal 4 Journal 5 Journal 6 Quiz 1 Quiz 2 Quiz 3 Quiz 4 Quiz 5 1. Post All writeCard ups due 2. Indiv. Goals. Clinical Rotation III Assignments for each clinical experience (first 9 weeks) Due by Week 1 Week 2 Week 3 4 Week Week 5 Week 6 Week 7 Journal 1 Journal 2 Journal 3 Journal 4 Journal Journal Journal 5 6 7 EBM EBM EBM EBM EBM EBM EBM 1. Post All writeCard ups are 2. Indiv. due Goals. Week 8 Journal 8 EBM Clinical Rotation III Assignments for each clinical experience (second 9 weeks) Due by Week 1 Week 2 Week 3 4 Week Week 5 Week 6 Week 7 Week 8 Journal 1 Journal 2 Journal 3 Journal 4 Journal Journal Journal Journal 5 6 7 8 Bates Bates Bates Bates Bates Bates Bates Bates Quiz 1 Quiz 2 Quiz 3 Quiz 4 Quiz 5 Quiz 6 Quiz 7 Quiz 8 1. Post All writeCard ups are 2. Indiv. due Goals. Clinical Preceptor Manual *105 Week 9 Journal 9 EBM Week 9 Journal 9 Bates Quiz 9 Clinical Experience Grading Points for Clinical Rotations I and II Faculty Assigned Post Card, Individual Goals Assessment, Prompt Assignments, Journals, Quality & Professionalism Write-ups/Case Reports (30 points each) Quizzes Preceptor Assigned Clinical Experience Exam 70 90 50 150 100 *minimum score of 70% is required on each exam. Re-takes of exams will not improve score for grade Total 460 Clinical Rotations III Faculty Assigned 75 points Post Card, Individual Goals Assessment , Prompt Assignments, Journals, Quality & Professionalism, These items must be completed for all clinical experiences that occur during course H&P H&P, SOAP NOTE, Procedure Note (25 points each) Exit Interview with Advisor Preceptor Assigned Grade Rotation Exams 25 75 This grade will be derived from the following examinations: 1) P1- post preceptorship psychiatry exam (15%) 2) P2-PD Online Quizzes (15%) 3) Comprehensive written final exam (70%) 35 150 100 *minimum score of 70% is required on each clinical experience exam – retakes of exams will not improve score for grade Total 460 The clinical rotations course grade will be calculated on the sum total of each clinical experience. The percentage of total points earned will be used for assigning a letter grade according to the table below. Also, understand that your preceptor evaluation is only part of your overall grade. As noted above your scores on write-ups, end of clinical experience exams and faculty evaluations are integral in determining your final grade. Clinical Preceptor Manual *106 Final Rotation Grade Assignment The grading assignment method for your clinical rotations is listed below: Points Percent Grade Quality Points 431-460 412-430 398-411 379-397 365-378 351-364 333-350 319-332 274-318 <274 93.5-100% 89.5-93.4% 86.5-89.4% 82.5-86.4% 79.582.4% 76.5-79.4% 72.5-76.4% 69.5-72.4% 60-69.4% 0-59.9% A AB+ B BC+ C CD E 4.0 3.7 3.3 3.0 2.7 2.3 2.0 1.7 1.3 0.0 Remediation During the clinical year each student must continue to maintain an overall 3.0 GPA in order to receive the Master of Health Science degree and certificate as a Physician Assistant. In addition to the overall GPA requirement students must attain a minimum of a B- (2.7) in each clinical experience. An unsatisfactory rating on any item on a clinical evaluation, or the clinical evaluation in total will result in failure of the rotation. Failure to achieve a minimum of a B- in any rotation will require that the student repeat the rotation. A grade of less than B- in more than one clinical experience will result in the student being dismissed from the program. A. Submissions Post Card Within the first week of each clinical experience you must complete the online postcard located on the student clinical web page entitled Update "Postcard" Contact Information If any information is missing from your “post card”, it will be considered incomplete and late. 1. Your name 2. Your mailing address 3. Name of your primary preceptor 4. Name of your clinic / hospital 5. Your clinic and hospital contact numbers 6. Your home or cell phone numbers 7. Copy of planned weekly schedule B. Individual Goal Assessment Within the first week of each clinical experience, the student will discuss their personal goals as well as objectives, as listed in the Preceptor manual, with the preceptor. This discussion will provide a chance to hear the preceptor’s Clinical Preceptor Manual *107 expectations and requirements for the student in that period. The student will then write out a formal goal plan (using the template at the end of this section) for that clinical experience which agrees with the discussion. All individual goal assessments must be signed by your precepting physician. Email or fax these to your faculty advisor by the end of the first week. Clearfield Fax: 814-768-3440 Lock Haven Fax: 570-484-2540 Harrisburg Fax: 570-484-2624 Coudersport Fax: 570-484-2607 C. Case Reports Case reports consist of a detailed discussion of the salient facts related to an interesting or unusual case you have seen in clinical practice. Unlike a SOAP note or H&P these reports contain a discussion of the critical history, physical examination and laboratory findings that led the author to the diagnosis, a brief summary of the pathophysiology involved, a differential diagnosis, and information regarding how this particular patient was treated, the current recommended treatment for the disorder and if variation in treatment occurred the rationale that was used. All case reports are referenced utilizing APA style. The exact requirements, including the grading rubric, can be found on the clinical web page. D. Write ups: In order to assure the breadth of your clinical experience, you will be required to submit various write-ups to your faculty advisor. Prior to the beginning of each semester you will meet with your advisor and you will be assigned the write-ups you need to submit by the end of each clinical experience. All write-ups, for each clinical experience, must be turned in by the end of the 4th week. Grading rubrics will be provided to assure students are clear regarding expectations for these write-ups. Students are required to complete the following write-ups during their clinical year. Listed below are the minimum number of write-ups in each category that you must complete. Write-ups can be combined to meet the requirements listed below. Case Reports-5 Complete H&P-4 Soap Notes-3 Admission H&P-1 Long term Care1 Pap/Pelvic Note1 Pre-natal Note1 Procedure Note1 Post-op Note-1 Out-patient Note-1 Pediatric Development Note-1 In-patient note-1 Clinical Preceptor Manual *108 Discharge Summary-1 Pediatric Well Child Exam-1 Psychiatric Note1 1. Complete H&P a. This assignment must contain a thorough and complete write-up including exhaustive review of systems, past medical history, family history, social history, meds, allergies, physical exam, assessment, & plan. b. During the clinical year one of each of the following are required as a component of a complete H&P: I. Health Promotion and Disease Prevention Plan (HPDP) for an adult patient II. Long Term Care Unit complete write-up including HPDP, assessment of long term care needs, and a thorough plan for addressing them. III. Pediatric H&P including anticipatory guidance that should be provided for parents of children in the following age ranges: a. 1-3 b. 4-6 c. 8-10 d. 10-15 e. >15 Write-ups will: be typewritten and submitted electronically to the Clinical PA Website be spell checked not contain any patient identifying information. be in standard format (S.O.A.P. , complete H&P, etc.) include the student’s impression of the patient’s diagnosis. include an appropriate treatment plan. not be done on pre-made office forms which uses check lists or the like be submitted via the Clinical PA Website for your faculty advisor to review and grade. Your supervising physician will review the original write-up and attach and sign the charting coversheet found at http://gradprograms.lhup.edu/pa/files/File/PAStudent%20Charting%20Evaluation.p df). You are to attach the grading sheet to the original write-up and hand carry it to your faculty advisor during PA days. Failure to hand in the graded write up will result in you receiving a zero for that assignment. You will be graded on the first submission only. Unacceptable notes will be returned to the student with suggestions for re-submission. After the corrections are made the write-up will be re-submitted. Failure to resubmit acceptable notes, prior to the end of the clinical experience, may result in failure of the rotation. E. Journals A daily journal is required for each day on a rotation or preceptorship. At the end of each week a journal entry must be entered into the online student Clinical Preceptor Manual *109 journal found on the On Clinical Year Student Site (http://gradprograms.lhup.edu/pa/). The journal serves numerous purposes including; 1) to serve as a reflection on your day to day activities within the clinic; 2) to assist your faculty advisor in evaluating your clinical experience 3) to assure you are acquiring a wide variety of clinical experiences in various settings. To facilitate an accurate journal, we suggest you carry a small notebook for notes during your workday. Your weekly journal is due each Sunday by midnight. Warning- Failure to submit a weekly journal entry on the online forms page will result in your failing the rotation! Heading 1. Your Name, 2. Dates of the Week & which week of the clinical experience 3. Specialty Type & Where Weekly Summary 1. A one-paragraph summary telling your feelings about that week’s Clinical experience. How are your progressing and if there are any problems. Daily Summaries 1. Date 2. Total hours worked. 3. Total Number of patients seen 4. Count on number of patients seen with each diagnosis or procedure and log them on the patient tally sheet. 5. Thought of the day: Either an interesting case or ethical issue or interpersonal issue you encountered & your thoughts on them. 6. Breakout of the payer class and age group for total number of patients seen (i.e. 16 Medicare, 12 Medicaid, 13 no insurance, 10 private insurance) 7. The patient tally sheets are vital in documenting your clinical experiences. After graduation insurance companies and hospital credentialing committee’s will require specific information regarding your training in order to grant privileges. These tally sheets serve as a reference, documenting your experiences and are used to verify your clinical experiences. We cannot verify this information if you fail to document them on your tally sheet. F. Quizzes on Readings Each week, for the first five weeks of your clinical experience, you will go to the LHUP Program website and find that week’s reading requirements. A link to a quiz that covers those readings is also given. Each weekly quiz must be Clinical Preceptor Manual *110 completed by midnight on Sunday. Quizzes completed after the deadline will not be graded and you will not receive credit for it. G. Preceptor Evaluation The Preceptor Evaluation form is in the back of this section. Copy this form as needed. Students are required to hand carry their preceptor evaluations to their faculty advisor on PA days at the end of their clinical experience or the student must make arrangements for the preceptor evaluations to be sent to the PA Program prior to the end of that clinical experience. Failure to hand in this evaluation could cause you to fail the clinical experience. H. End of Clinical Experience Testing Upon completion of each clinical experience, the student will take an end of clinical experience exam. These exams are important in preparing you for the national certification exam and to that end you will be taking the 5 exams given below. During your elective clinical experience you will do the readings, quizzes and clinical experience exam in either OB-GYN or ER. Due when you return from: Clinical Rotations I, II Exam(s) 1. Internal Medicine 2. Pediatrics 3. Surgery 4. Ob-Gyn 5. ER Clinical Rotations III Psychiatry Summative Exam Post Clinical Preceptorship exam Pharmacy Exam The topics covered in the exams can be found in Section III. These topics correspond to those that are commonly encountered both in practice and on national boards. You will need to do your own reading to assure your competence in these areas. A score of 70 percent or better on each examination is required in order to be eligible for graduation from the Department of Physician Assistant Studies. I. Practical Examination During the clinical year each student will be scheduled for clinical skills examinations with a faculty member. The PA student handbook addresses oral/practical examination repeat and/or failure policies. Clinical Preceptor Manual *111 1. The first unsatisfactory performance on a practical/oral will result in the exam being re-scheduled, with a different faculty member, at a time convenient for the faculty member. 2. If on the second attempt the student is unsuccessful in completing the exam the student will be counseled and provided with a written contract that outlines the requirements for successful completion of the assignment. A retake examination will then be scheduled at the end of the semester, after the completion of all exams, on the last day of final exams week, or at another end of semester time determined by the faculty. 3. Failure of this third attempt will result in dismissal from the program. PA Student Handbook 2010-2012 All clinical experience practical examinations must be completed by the last day of the fall semester. Following each clinical experience students will return to the University main campus for testing. Clinical skills examination will be scheduled by the clinical coordinator. All students will complete a minimum of two directed exams during the clinical year. The first practical will be administered either following the first or second clinical experience. Students who fail to meet the minimum requirements for these directed practical exams will complete an additional practical exam following their third clinical experience. All students will complete a second practical exam following clinical experience 4 or 5... The following are examples of the topics that will be used, as well as a sample evaluation format. Chest Pain Dyspnea Abdominal Pain Joint or Back Pain Change in Mental Status In addition, students are expected to be prepared to complete a thorough directed history, physical exam, differential diagnosis, order appropriate laboratory and imaging studies, develop an appropriate treatment and patient education plan for: Chest Pain: MI, Pericarditis, Costochondritis Dyspnea: Pneumothorax, Pneumonia, Anemia, TB, Asthma Abdominal Pain: Appendicitis, Diverticulitis, Cholecystitis, Irritable Bowel Syndrome Joint Pain: MS Strain, RA, Septic Joint, Metastatic Disease Change in Mental Status: CVA, Alzheimer’s, Sub-Dural Hematoma, Polypharmacy, Metabolic toxicity Summative Evaluation At the completion of your clinical experience all students will be required to complete a summative evaluation process. This process will include written examinations, clinical OSCE exams, a diagnostic station and therapeutics station. All students must successfully complete these exams in order to Clinical Preceptor Manual *112 successfully complete the program. Students will be allowed to remediate the summative examination one time. If they remain unsuccessful then they will be required to enroll in appropriate remedial activities that may result in delay of their expected graduation. Clinical Preceptor Manual *113 Lock Haven University of Pennsylvania Physician Assistant Program Fax 570-484 2540 Student’s Section Student’s Name: Faculty Advisor: Date: Clinical Specialty: Rotation Location: Preceptor’s Name: Write ups that you are submitting: 1.________________________________________________________________ 2.________________________________________________________________ 3.________________________________________________________________ Preceptor’s Section Unacceptable Poor 0 points 1 point Average 2 points Good 3 points Superb 4 points Legibility Content Preceptor’s Comments: (Optional) Preceptor’s Signature _________________________________________________________ Clinical Preceptor Manual *114 Section Five: EVALUATION FORMS Clinical Preceptor Manual *115 LOCK HAVEN UNIVERSITY OF PENNSYLVANIA PHYSICIAN ASSISTANT PROGRAM STUDENT CRITIQUE FORM Student Rotation/Preceptorship Site Period (circle one) I II III IV V P1 P2 Utilizing the following scale, respond to each of the following statements by choosing a number from the scale that most closely indicates the degree with which you agree or disagree. Please write “NA” if not applicable. STRONGLY DISAGREE 1 2 3 1. 3. Obtain and record a thorough and reliable history. Obtain and record a thorough and reliable physical exam. Develop a problem list. Develop a list of possible etiologies (differential diagnosis). Order appropriate studies. Recommend rational therapy. Communicate with health team. Increase proficiency in technical procedures. Increase knowledge of patient problems in primary care. My responsibilities such as assignments, rules and regulations, were clear to me. My housing arrangements were adequate. Costs: Room Board Other 4. STRONGLY AGREE 5 6 This preceptorship enabled me to meet the following objectives: a. b. c. d. e. f. g. h. i. 2. 4 /week /week /week Describe housing arrangements Estimate the number of hours “on the job” during an average week Of these hours, how many were: In the doctor’s office In the hospital with inpatients In the emergency room In the nursing home On a house call Other (please describe) hours/week Number Total Clinical Preceptor Manual *116 5. Were medical conferences, such as grand rounds, available? Did you attend? 6. Did you participate in any other community activities? 7. At the beginning and end of this preceptorship my anxiety for encountering patients was: (circle the number from the scale best expressing your anxiety): (describe) NO ANXIETY a. At the beginning: b. At the end: 8. 1 1 GREAT ANXIETY 2 2 3 3 4 4 5 5 6 6 Circle the amount of progress you have made during this preceptorship: 1 Minimal Progress 2 3 4 5 6 Maximum Progress 9. The preceptor’s understanding of the role of the PA student was adequate: Yes No Explain: 10. List the physicians with whom you spent part of this preceptorship period, approximate time spent with each and type of practice of each. PHYSICIAN 11. TYPE OF PRACTICE The preceptor used the following teaching techniques: NEVER 1 2 3 4 5 a. b. c. d. e. f. g. h. i. j. k. l. 12. % OF TIME Directly observed the student Confirmed student’s data by redoing or rechecking Provided oral feedback on performance Provided adequate “hands on” experience Directed student to literature Made reading assignments Assigned research projects Orally quizzed or questioned student Demonstrated technique to student Set specific goals for student Asked student for self-evaluation Directed student to lectures, grand rounds, CME, etc. List ways in which this preceptorship could be improved: Clinical Preceptor Manual *117 6 ALWAYS Lock Haven University of Pennsylvania Physician Assistant Program 432 Railroad Street, Lock Haven, PA 17745 570-484-2541 Fax 570-484-2540 PRECEPTOR EVALUATION Student Name: _____________________________________________________________ Preceptor: _________________________________________________________________ Date: ______________________ Please select specialty: o o o o o o o Family Medicine/Primary Care Obstetrics/Gynecology Emergency Medicine General Surgery Internal Medicine Pediatrics Elective: ___________________________________________ Definition of Terms: Honors-The student exceeded expectations throughout the rotation. They demonstrated the highest level of intellectual ability,motivation, and self disciple which clearly set him/her apart from the majority of other students. Above Average- The student perform at a high level of competency and exhibitied a significant degree of intellectual ability,motivation, and self disciple. Areas of weakness were not substantial or were accountable to lack of sufficient expereince. Adequate- The student meet the minimum requirements established by the preceptor for this rotation. They had clear areas of weakness but resonded well to remedition efforts. Inadequate- The student did not meet the minimum standards. Areas of weakness were identified early in the rotation but thte student was unresponsive to remedition efforts by the preceptor. Please document such efforts in the remarks section for review by the PA Program. Clinical Preceptor Manual *118 Did you identify any areas of weakness in the student’s preparation for this rotation? Clinical Preceptor Manual *119 Section Six: AGREEMENT FORMS Clinical Preceptor Manual *120 AFFILIATION AGREEMENT This agreement is made and entered into as of this day of , 20 , by and between Lock Haven University of Pennsylvania of the State System of Higher Education (“School”) and (“Hospital”) WITNESSETH: WHEREAS, School offers to enrolled student a master’s degree program for the Physician Assistant Program; and WHEREAS, Hospital manages a comprehensive inpatient and outpatient facility; and WHEREAS, School desires to provide to its students a clinical learning experience, under the supervision of licensed physicians with medical staff privileges at Hospital; and WHEREAS, Hospital has agreed to make its facility available to School for such purpose; NOW, THEREFORE, in consideration of the mutual promises contained herein, the parties hereby agree as follows: 1. Responsibilities of School a. Clinical Program: School shall be responsible for the implementation and operation of the clinical component of its program at Hospital (“Program”), which Program shall include, but not be limited to, the following: (1) provision of classroom theory and practical instruction to students prior to their clinical assignment at Hospital; (2) continuing oral and written communication with Hospital regarding student performance and evaluation, absences and assignments of students, and other pertinent information; (3) periodic on-site visitation by Program faculty; (4) participation, with the students, in Hospital’s Quality Assurance and related programs; (5) performance of such other duties as may from time to time be agreed to between School and Hospital. (6) all students, faculty, employees, agents, and representatives of School participating in the Program at Hospital (“Program Participants”) shall be accountable to the Hospital’s clinical education coordinator or other designee. b. Student Statements: School shall require each Program Participant to sign a Statement of Responsibility in the form attached hereto as Exhibit A, and a Statement of Confidentiality in the form attached hereto as Exhibit B. c. Insurance: School shall require that student Program Participants obtain and maintain their own appropriate professional liability insurance coverage in amounts acceptable to Hospital. Hospital understands and agrees that such student insurance coverage is not provided to students by School itself. Hospital further understands and accepts as sufficient that School’s faculty and other employees are covered by the Commonwealth of Pennsylvania’s Tort Claims Self-Insurance Program, administered by the Bureau of Risk and Insurance Management of the Department of General Services. Clinical Preceptor Manual *121 d. Health of Participants: All Program Participants shall pass a medical examination acceptable to Hospital prior to their participation in the Program at Hospital. Program Participant shall be responsible for arranging for the Program Participant’s medical care and/or treatment, if necessary, including transportation. In no event shall Hospital be financially or otherwise responsible for said medical care and treatment. School will require each student upon their arrival at the Indian Health Service facility to provide evidence of rubella and rubeola immunity and tuberculin skin test status. If the latter is positive, there shall be evidence of treatment in accordance with Centers for Disease Control and Prevention guidelines. e. Dress Code: School shall require Program Participants to dress in accordance with dress and personal appearance standards approved by School (and consistent with Hospital’s standards regarding same), including a distinctive coat with the School insignia and an identifying badge with the student’s name and “Physician Assistant Student” clearly visible. f. Performance of Services: All physician preceptors (Preceptor) supervising students will be licensed physicians with staff privileges at Hospital. (1) Preceptors will supervise and coordinate on a day to day basis the clinical experiences of the student with Hospital. (2) School acknowledges that Preceptor is neither the agent nor employee of Hospital for purposes of supervision and coordination of student’s clinical experiences at Hospital. (3) School will provide a faculty member (“Clinical Coordinator”) who will provide educational supervision of all students on behalf of the School, act as liaison between the School and Hospital and Preceptor. (4) School and all Program Participants shall perform their duties and services hereunder in accordance with all relevant local, state and federal laws, comply with the standards and guidelines of all applicable accrediting bodies, the Bylaws and rules and regulations of Hospital, and any rules and regulations of School as may be in effect from time to time. Neither School nor any Program Participant shall interfere with or adversely affect the operation of Hospital or the performance of services therein. (5) School shall at all times remain solely responsible for the evaluation and grading of Program Participants. (6) Unless prior agreement otherwise, School agrees not to send any student(s) who have, at the end of the didactic year, less than a 3.0 grade point average (on a 4-point scale) to Hospital. 2. Responsibilities of Hospital a. Hospital shall accept the students assigned to the Program by School and cooperate in the orientation of all Program Participants to Hospital. Hospital shall provide the opportunities for such students, who shall be immediately supervised by Preceptors, to observe and assist in various aspects of patient care consistent with the role of Physician Assistant students. b. Hospital shall assist School in coordinating rotation and assignment schedules with its own schedule and those of other educational institutions. c. Hospital shall at all times retain ultimate control of the Hospital and responsibility for hospital care of patients. Clinical Preceptor Manual *122 3. 4. 5. 6. d. Emergency Outpatient treatment for injuries sustained while performing assigned services will be provided the intern/student/resident. They may also be provided temporary care and treatment in HIS facilities under the same circumstances and to the same extent such care and treatment may be provided to paid employees. Responsibilities of the Student a. Insurance: Student Program Participants shall be responsible to obtain and maintain their own appropriate professional liability insurance coverage in amounts acceptable to Hospital. Hospital understands and agrees that such student insurance coverage is not provided to students by School itself. Hospital further understands and accepts as sufficient that School’s faculty and other employees are covered by the Commonwealth of Pennsylvania’s Tort Claims Self-Insurance Program, administered by the Bureau of Risk and Insurance Management of the Department of General Services. b. During all activities in which students, volunteers, or residents will be interacting or providing care to children less than 18 years old, such activities must be performed within the sight and under the supervision of an Indian Health Service employee who has satisfactorily completed the Child Care National Agency Check with Written Inquiries (CNACI) Security Investigation. Withdrawal of Program Participant a. Hospital may request School to withdraw or dismiss a student from the Program at the Hospital when his/her performance is unsatisfactory to Hospital, or his/her behavior is disruptive or detrimental to Hospital and/or its patients. b. Hospital may, at its discretion, immediately curtail activities of a Program Participant if, in Hospital’s opinion, doing so is in the best interest of the Hospital and/or its patients. In such event Hospital will immediately notify School and Preceptor of its action. Independent Contractor a. The parties hereby acknowledge that they are independent contractors, and neither the School nor any of its agents, representatives, faculty, students or employees shall be considered agents, representatives, or employees of Hospital. b. In no event shall this Agreement be construed as establishing a partnership or joint venture of similar relationship between the parties hereto. c. No Program Participant shall look to Hospital for any salaries, insurance or other benefits. d. All parties acknowledge that the student’s purpose in participating in a clinical experience at Hospital is educational, and that the student, though he/she may provide services to patients at the Hospital, shall not be used as a substitute for regular staff. Confidentiality a. School and its agents, students, faculty, representatives and employees agree to keep strictly confidential and hold in trust all confidential information of Hospital and/or its patients and not disclose or reveal any confidential information to any third party without the express prior written consent of Hospital. b. Neither School nor Hospital shall disclose the terms of this Agreement with any person who is not a party to this Agreement except as required by law or as authorized by the other party to this agreement. Clinical Preceptor Manual *123 7. Term; Termination a. The initial term of this agreement shall be for one year and commence . At the end of the initial term, unless otherwise terminated as provided herein, this Agreement may be renewed for one year for up to four successive terms upon mutual agreement of the parties. b. Either party may terminate this Agreement at any time upon at least thirty (30) days written notice. In the event the Hospital terminates the agreement any student enrolled in the clinical program may continue his or her educational experience until it would have concluded absent termination. 8. Nondiscrimination a. Nondiscrimination. The parties agree to continue their respective policies of nondiscrimination based on Title VI of the Civil Rights Act of 1964 in regard to sex, age, race, color, creed, national origin, Title IX of the Education Amendments of 1972 and other applicable laws, as well as the provisions of the Americans with Disabilities Act. 9. Interpretation of the Agreement a. The laws of the Commonwealth of Pennsylvania shall govern this Agreement. 10. Modification of Agreement a. This Agreement shall only be modified in writing with the same formality as the original Agreement. 11. Relationship of Parties a. The relationship between the parties to this Agreement to each other is that of independent contractors. The relationship of the parties to this contract to each other shall not be construed to constitute a partnership, joint venture or any other relationship, other than that of independent contractors. 12. Liability a. Neither of the parties shall assume any liabilities to each other. As to liability to each other or death to persons, or damages to property, the parties do not waive any defense as a result of entering into this contract. This provision shall not be construed to limit the Commonwealth’s rights, claims or defenses, which arise as a matter of law pursuant to any provisions of this contract. This provision shall not be construed to limit the sovereign immunity of the Commonwealth or of the State System of Higher Education or the University. 13. Entire Agreement a. This Agreement represents the entire understanding between the parties. No other prior or contemporaneous oral or written understandings or promises exist in regards to this relationship. Clinical Preceptor Manual *124 IN WITNESS WHEREOF, the parties hereto have executed this Agreement. Representative of Lock Haven University Date Representative of Hospital Date Clinical Preceptor Manual *125 EXHIBIT A STATEMENT OF RESPONSIBILITY For and in consideration of the benefit provided the undersigned in the form of experience in evaluation and treatment of patients of Hospital, the undersigned, and his/her heirs, successors and/or assigns does hereby covenant and agree to be solely responsible for any injury or loss sustained by the undersigned while participating in the Program operated by Lock Haven University at Hospital, unless such injury arises solely out of Hospital’s negligence or willful misconduct. Program Participant (Signature) Date Program Participant (Printed Name) Witness Date Clinical Preceptor Manual *126 EXHIBIT B CONFIDENTIALITY STATEMENT The undersigned hereby acknowledges his/her responsibility under Federal applicable law and the Agreement between Lock Haven University (School) and Hospital to keep confidential any and all information of Hospital. The undersigned agrees, under penalty of law, not to reveal to any person or persons except authorized clinical staff and associated personnel any specific information regarding any patient, and further agrees not to reveal to any third party any confidential information of Hospital. Program Participant (Signature) Date Program Participant (Printed Name) Witness Date Clinical Preceptor Manual *127 MEMORANDUM AGREEMENT This agreement is entered into by and between the Lock Haven University of Pennsylvania, Department of Physician Assistant and Graduate Studies in Education—Physician Assistant Program (Program) and (Preceptor) for the purpose of providing a clinical experience, in conjunction with required course work, to student within the Program. 1. The Program and the Preceptor agree that the policies, procedures and objectives of the Program shall govern the operation of the clinical experience. 2. The Program agrees that each student will be required to maintain his or her own professional liability insurance protection in the amount of $1,000,000 per plaintiff and $3,000,000 per occurrence. Proof of such insurance protection will be provided to Preceptor prior to the student being allowed to participate in any clinical activities. Preceptor understands and agrees that such coverage is not provided to students by the Program itself. 3. Program and Preceptor agree that Program faculty will establish the course objectives, activities, requirements, standards and methods of evaluation for each course for which clinical experiences are offered. 4. The Preceptor agrees to provide supervised clinical instruction. 5. The Preceptor agrees to coordinate the use of necessary health provider facilities including hospitals, clinics and other facilities for the appropriate instruction of students. 6. The Preceptor agrees to complete, as required, an evaluation form regarding the student’s performance, and to notify the Program Director or Medical Director immediately of any adverse concerns, problems, incidents, claims or potential claims arising from the actions of the student(s) during the course of the clinical experience. 7. This agreement shall be effective with the date of the preceptor’s appointment and will continue until that appointment is terminated. Signature of Preceptor Date Signature of Program Director Date OR Clinical Preceptor Manual Signature of Medical Director *128 Date Date Physician Assistant Program Lock Haven University of Pennsylvania PRECEPTORSHIP APPLICATION FORM PLEASE PRINT OR TYPE ALL INFORMATION NAME License #/State Last First Middle Office Address Office Phone ( ) Fax Number Email zip code 1. Physician Specialty 2. M.D. D.O. M PA-C F Year received degree Please attach a copy of your current Curriculum Vitae. 3. Are you now, or have you been, associated with professional medical personnel training programs? yes no If yes, please list: 4. List your current professional affiliations: 5. A representative number of patients seen in my office per day would be: (1) none (2) 1-5 (3) 6-10 (4) 11-15 (5) 16-20 (6) 21-25 (7) 26-30 (8) 31-35 (9) 36-40 (10) 41 plus 6. A representative number of patients I encounter in the hospital per day would be: (1) none (2) 1-5 (3) 6-10 (4) 11-15 Clinical Preceptor Manual (5) 16-20 (6) 21 plus *129 7. Indicate the areas in which the student will participate and estimate the % time for each. Yes No Adult Medicine (Internal Medicine) Surgery (includes specialty) Pediatrics Obstetrics Gynecology Geriatrics Emergency Medicine Other Percent Time % % % % % % % % 8. As a component of your preceptorship, do you anticipate that the physician assistant student will be involved in the care of your hospital patients? yes no 9. Please list all facilities where you have staff privileges: 10. Name of your office/clinic: 11. Number of examining rooms in your office/clinic: 12. Is a laboratory facility located in the office/clinic? yes no 13. Estimate the average number of ACTUAL CONTACT HOURS OF TEACHING (one to one or in a group) that you as preceptor provide, or will provide, to a student during a six (6) week or eighteen (18) week clinical experience. Choose a time frame of a day, a week, or a six (6) week or eighteen (18) week period to indicate your estimate of teaching hours. Use only one time frame, that which is descriptive of your practice. hours/day hours/week hours/6 weeks hours/18 weeks 14. Will other physicians, physician assistants, nurse practitioners, etc. in the practice/group be involved in teaching the physician assistant student? yes no If YES to the preceding question, list the names of the physicians and other professionals, who will be working with the physician assistant student during a six week period (preceptorship). Clinical Preceptor Manual *130