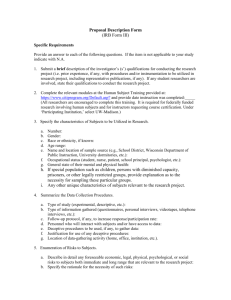
Study Type and Performance Site
advertisement

Table of Contents Funding Study Type and Performance Site Study Purpose and Direction Research, Activities, Procedures, and Schedule of Events for Study Participants Data and Safety Subject Population(s) Children Cognitively Impaired Pregnant Women, Fetuses, Neonates Prisoners Recruitment Radiation Procedures and Radioactive Drugs Drugs, Devices, Biologics PHI/Consent Conflict of Interest Disclosure Signing Other Committee Approval Help and Suggestions Funding Internal Funding Information Identify if the study is either not funded or if the study is funded by internal funds such as departmental funds, personal funds, or a donor/gift. External Funding Information If the study is funded or supported by an external funding source such as a grant from a Federal or private agency, contract from a pharmaceutical company or other entity, or a sub-contract from another university or research organization; provide information regarding the external funding source. When a commercial entity contracts through a Federal agency but not directly with Vanderbilt University, only include the Federal agency. This information should include identification of the agency/sponsor, the funding mechanism (grant or contract), and if the award is pending or has been awarded. IRB fees may apply. Funding Information – Industry-Supported The VU IRB currently charges for the review of those studies or clinical trials that are supported by industry. A study is determined to be Industry-Supported if a commercial entity contributes to the design or conduct of the study (as evidenced by a sponsor’s protocol, sponsor’s identification number and/or Investigator’s brochure); coordinates the study as a multi-center trial; reimburses VU or a VU Investigator for costs associated with conducting the trial; or will have access to, or publish/present the data gained from conducting the trial. Identify if this study is “Industry-Supported.” If yes, a VU center number and account number must be provided for the payment of the $2250 (Full Committee/$500 (Expedited) fee for initial review. If this is VSRH, IEI, or other non-Vanderbilt site, payment is required as specified in the signed MOU. Indicate whether a check payable to the “VU IRB” in the amount of $2250 (Full Committee)/$500 (Expedited) is attached or if a check has been requested. Requests for a waiver of this fee must be submitted in writing to the IRB Director at 504 Oxford House (4315). Industry-Supported studies that do not include this information will not be accepted for processing. Study Type and Performance Site Vanderbilt University Serving as the Coordinating Center or Lead Institution A multi-center study is one where different PIs at different institutions are conducting the same study. The coordinating center/lead institution is the site responsible for coordinating the collection of data across all institutions involved in the project. If VU is the lead institution, all additional participating institutions must be listed in this section of the application and letters of IRB approval from each of the listed institutions must be provided to the VU IRB. It is important for the IRB to understand what Vanderbilt’s function is in relationship to a multi-center research project; therefore, details of the PI’s plan to assure data collection and participant safety should be included in the Data and Safety section of this application. Location of Research It is important for the VU IRB to obtain information regarding the location(s) where research will be conducted. This is commonly referred to as a “performance site” because it is the site where the PI/additional study personnel are performing research activities. Depending on the location of the performance site and the type of affiliation with Vanderbilt University that may exist (i.e., contractual arrangement, coordinating center, etc.), the VU IRB may be required to obtain different types of information regarding a performance site. Engaged Versus Not Engaged in Research Performance Sites Engaged in Research A performance site is considered to be “engaged in research” when an employee or agent of the performance site: (i) intervenes or interacts with a living individual for research purposes; (ii) obtains individually identifiable private information for research purposes; or (iii) receives a direct federal award (grant) to support the research activities. Performance Sites NOT Engaged in Research A performance site is considered to NOT be “engaged in research” only when there are NO employees or agents of the performance site that: (i) intervene or interact with a living individual for research purposes; (ii) obtain individually identifiable private information for research purposes; or (iii) the performance site DOES NOT receive a direct federal award (grant) to support the research activities. Engaged In Research IRB of Record All performance sites “engaged in research” must have their portion of the study reviewed by an IRB. Indicate if the VU IRB is the “IRB of Record” for the Performance Site’s portion of the study or if another IRB is the “IRB of Record” for the Performance Site’s portion of the study. NOTE: If the PI at the performance site requests for the VU IRB to serve as the IRB of record for the Performance Site “engaged in research”, a Memorandum of Understanding will need to be negotiated with the appropriate institutional official at the performance site and the IRB Director. Contact the IRB Office at 615-322-2918 or 1-866-224-8273 for more details. Performance Site List the name of the performance site where research will be conducted. FWA Holding Institution. The performance site may either be associated with an institution that holds a Federal Wide Assurance (FWA) with the Federal Government or may hold an FWA directly. It is important to know that holding an FWA allows an institution/performance site to receive federal support for the conduct of human subjects research. IRB Approval A copy of IRB approval for a non-VU performance site must be forwarded to the VU IRB before final approval may be granted for research to begin at the performance site. Indicate if the approval letter is attached or is pending IRB review. It is the Investigator's responsibility to obtain and maintain current IRB approval letters for all non-VU performance sites. Below are some examples: Example #1: Dr. VU plans to collaborate with Dr. Private on a research study funded by the NIH. Both PIs will be collecting blood from patients seen in their clinics (VUMC Clinic and The Private Clinic) for this research study. What should Dr. VU do? In addition to choosing VU as a performance site, Dr. VU should list The Private Clinic as a performance site. Second, he should verify with Dr. Private that her clinic either has an FWA or is associated with an institution that has an FWA. After discussing with her, she indicated that her clinic is associated with Metropolitan Health Department for Nashville & Davidson County. She further indicated that Metro has an FWA and that her portion of the research will be reviewed by Metro’s IRB. NOTE: When a performance site “engaged in research” does not have an FWA, you should instruct officials at that site to work with the Division of Assurances and Quality Improvement at the Office of Human Research Protections (OHRP) to file for an FWA. You can access their office on-line at: http://www.hhs.gov/ohrp/assurances/ Example #2: Sally Student is a VU Doctoral Candidate and is ready to begin her dissertation research. Currently, she is an employee of the University of Colorado in their Children’s Center and has just received a grant from the U.S. Department of Education for her intervention program with the center. Sally would like to use the data she gathers under this grant for her dissertation research. What should Sally do? Sally not only needs to obtain IRB approval from the Vanderbilt University IRB because she is a student, but she also needs to obtain IRB approval from the University of Colorado because that institution is receiving a direct award for the conduct of research. NOTE: The assurance number provided to the DOEd should be that of the University of Colorado, not that of Vanderbilt University. Further, she should list the University of Colorado Children’s Center as a Performance Site and should then indicate that the University of Colorado is the FWA Holding Institution and that their IRB is also responsible for reviewing the study on behalf of that University. NOT Engaged in Research Name of Performance Site. List the name of the performance site where research will be conducted. 1. Performance Site IRB. If the Performance site has an IRB indicate if a copy of the approval letter is attached or indicate if the approval letter is pending IRB review. 2. No Performance Site IRB. If the Performance site does not have an IRB, a letter of cooperation must be provided. This letter should be signed by the appropriate institutional official from the Performance Site and should state that the institution fully understands the research and agrees to allow the use of the performance site facilities for research purposes. Indicated if the letter is attached or is pending. Below are some examples: Example #1: Dr. VU plans to review Metro Health Department Records and is working alone. Despite the fact that these are public records, they do include names and identifiers and are only located in the offices of Metro Health Department. What should Dr. VU do? Dr. VU should list Metro Health Department as a Performance Site and should verify with officials there if they have an IRB or IEC. After discussing with officials at Metro, they indicate that they do have an IRB and this study will need IRB review and approval. Dr. VU should indicate that IRB approval from the Performance Site is pending. NOTE: Final VU IRB Approval cannot be granted until a copy of the IRB Approval from the Performance Site has been obtained. Example #2: Sally Student plans to observe a first grade class at Fairview Middle School for her dissertation research. She is working directly with her advisor, Dr. Guidance, but there is not an investigator at the school working with her on the research. What should she do? Sally Student should list Fairview Middle School, which is part of the Williamson County School District, as a Performance Site and should verify with officials there if they have an IRB or IEC. After discussing with the Principal at the school, he indicates that they do not have an IRB/IEC, but approval to conduct her research will have to be obtained from the Williamson County School Board. Sally Student should indicate that a Letter of Cooperation from the Performance Site is pending. NOTE: Final VU IRB Approval cannot be granted until a copy of the Letter of Cooperation from the Performance Site has been obtained. Study Purpose and Direction Purpose of the Study/Study Abstract Health Science: Provide a summary that describes the specific scientific objectives of the proposed research understandable to the IRB committee members. The IRB Committees are comprised of scientists with varied backgrounds, non-scientists, and community members. Provide the phase and expected duration of the study. Note: A separate Informed Consent Document and Clinical Trial Patient Cost Template should be created for each phase of a study. Social and Behavioral Science: In 250 words or less, provide a summary that describes the specific scientific objectives and purpose of the proposed research in lay language. Also describe any interventions that will be used with participants, the kind of data that will be collected, and how the data will be used to answer your study question. Description/Background of the Study Health Science: This should include the hypothesis; previous experience, including human and animal safety data, if applicable; and a critical evaluation of existing knowledge about the research topic. A reference list and copies of pertinent articles can be appended if thought to be of value in the evaluation of the proposed research by the IRB. Social and Behavioral Science: Provide a description of all background information regarding the proposed research. This should include the specific aims, hypothesis, or research question and relevant literature. A critical evaluation of existing knowledge about the research topic. A reference list and copies of pertinent articles can be appended if thought to be of value in the evaluation of the proposed research by the IRB. Research, Activities, Procedures, and Schedule of Events for Study Participants Data Collection, Storage of Data/Specimens, and/or Issues of Confidentiality NOTE: Any device (e.g., personal computer, laptop, etc.) used to save or store individually identifiable health information must be either encrypted or saved on a server housed in an approved data center. Vanderbilt Medical Center has agreed to use Check Point. For more information and how to obtain Check Point please visit the website: Information Privacy and Security. Describe the methods in which data will be collected, stored, and how confidentiality of participants will be maintained. This description should include information regarding the tools that will be utilized in the collection and storage of research information (hard copies and electronic databases, specimens, audio/videotapes, etc.), who will have access to the research information, what will be done with the data/specimens once the research is complete, issues specific to the study that might increase the risk of a breach of confidentiality such as the use of video tapes, how codes will be generated if codes are used to protect the identity of participants, and who will have access to these codes. In addition, the VA has specific guidance on the banking of human research subjects’ specimens. Describe how the confidentiality of participants will be assured. Include a description of any issues specific to the study that might increase the risk of breach of confidentiality. For example, video/audiotapes, discovering information about the participant that could be harmful if released such as mental illness, genetic information, sexual preference, drug abuse, etc. Describe how codes will be generated if codes are used to protect identities, and who will have access to such codes. If a certificate of confidentiality will be provided, include the name of the person holding the certificate. NOTE: A certificate of confidentiality can be requested from the federal government in the event that a study will obtain sensitive, private information that is directly linked to the participant. For more details, see “Certificates of Confidentiality Kiosk” at http://grants1.nih.gov/grants/policy/coc/index.htm. Behavioral Observation It is common in the behavioral sciences to conduct observations of the behavior of individuals. These observations may be done in public settings such as parks or shopping malls or in other non-public settings such as classrooms or hospitals. Identify whether or not this study includes behavioral observation. Describe the focus, duration, and number of observations and specify how the observations will be recorded and who will do the recording. Randomization (Random Assignment, Randomized) The assignment of participants to different treatments, interventions, or conditions according to chance rather than systematically (e.g., as dictated by the standard or usual response to their condition, history, prognosis, or according to demographic characteristics) is commonly referred to as randomization. Random assignment of subjects to conditions is an essential element of experimental research because it makes more likely the probability that differences observed between subject groups are the result of the experimental intervention. Identify whether or not this study includes randomization. If so, briefly describe the method that will be used to randomize participants. Blinding (Masking) Studies that are designed to compare two or more interventions in which either the Investigators, the subjects, or some combination thereof do not know the treatment group assignments of individual subjects are referred to as "blind" or “masked” study designs. Identify whether or not this study involves blinding/masking. If “yes”, provide a description of the blinding/masking. This should include a description of who will be blinded/masked, if and when research results or previously blinded/masked treatment assignments will be made available to participants when the study is completed and any provisions for breaking the blinding/masking (e.g., SAE, emergency visit, participant's request, etc.). Surveys, Interviews, and Questionnaires Identify whether or not this study involves the use of surveys, interviews, or questionnaires. If surveys, interviews or questionnaires will be conducted with this study, indicate who will conduct the survey, interview or questionnaire. In addition, describe the setting and mode of administering the instrument (e.g., by telephone, one-on-one, group, etc.) and attach a copy of all instruments. In addition, indicate if any questions, or pictures shown, may be of a "sensitive" nature to the participant. (e.g., graphic depictions of violence, explicitly sexual stimuli). Documents and Artifact Collection Describe any materials that may be collected during the course of this research (e.g., patient journals, quality of life journals, personal journals, student written assignments, etc.) that are to be collected. Deception, Withholding, or Postponing Medications/Treatments or Imposing Other Restrictions Identify whether or not this study involves deception, withholding or postponing medications/treatments, or imposing other restrictions. If so, describe the methods of deception to be used, the medications being withheld or postponed, the length of time medications will be withheld or postponed, any other restrictions to be imposed on participants (i.e., diet, exercise), and the precautions that will be taken to decrease or eliminate risks to participants. Audio/Video Recording The use of audio or videotapes provides for a direct link to the participant. The IRB must clearly understand the need for the use of audio or videotapes, as well as the plans for storage and timeline for destruction of the tapes. Specimen Collection Identify whether or not this study involves the collection of specimens such as blood, tissue, saliva, hair, urine, nail clippings, etc. If the study involves the collection of blood, identify the amount in teaspoons or tablespoons, timing and frequency of blood draws. For all other specimen collections, describe the type of collection and frequency of collection. Indicate if the specimens obtained will be used for genetic testing for this study or for the future. If “yes” include the genetic template language from the IRB web-site into the consent document. Schedule of Events and Financial Liability for Study Participants It is important for the IRB as well as the participant to understand what research-related activities/procedures will be conducted, the frequency of the activities/procedures, where the activities/procedures will occur, and who will be responsible for the costs associated with each of these activities/procedures. It is important to include this information in a summary format to the participant in the informed consent document. http://www.cms.hhs.gov/center/coverage.asp - this is a link to the Medicare Coverage Center where national and local coverage determinations can be found. http://www.cms.hhs.gov/manuals/Downloads/bp102c16.pdf - this is a link to Medicare Benefit Policy Manual Chapter 16 entitled “General Exclusion from Coverage” For assistance in developing a budget access the Department of Finance and click on “Clinical Trial Patient Cost Template.” Additionally, you may contact Research Support Services Hotline at 322-7343 and assistance with this procedure can be obtained. Please note: When you submit the Clinical Trial Patient Cost Template to Finance and to the IRB for review you are attesting to its accuracy and stating it is your plan for billing the study. Changes to the Clinical Trial Patient Cost Template must be submitted to Finance and the IRB must be notified through submission of an IRB amendment if there are changes to the template. Both Finance and the IRB will utilize the latest version submitted for their reviews. Study Type Information Expedited Review is a term defined by federal regulations and is only applicable when research is no more than minimal risk and the research fits into one or more of the following expedited review categories: (F)(1) Clinical studies of drugs and medical devices only when condition (a) or (b) is met. (a) Research on drugs for which an investigational new drug application (21 CFR Part 312) is not required. (NOTE: Research on marketed drugs that significantly increases the risks or decreases the acceptability of the risks associated with the use of the product is not eligible for expedited review.) (b) Research on medical devices for which (i) an investigational device exemption application (21 CFR Part 812) is not required; or (ii) the medical device is cleared/approved for marketing and the medical device is being used in accordance with its cleared/approved labeling. (F)(2) Collection of blood samples by finger stick, heel stick, ear stick, or venipuncture as follows: (a) from healthy, nonpregnant adults who weigh at least 110 pounds. For these subjects, the amounts drawn may not exceed 550 ml in an 8 week period and collection may not occur more frequently than 2 times per week; or (b) from other adults and children2, considering the age, weight, and health of the subjects, the collection procedure, the amount of blood to be collected, and the frequency with which it will be collected. For these subjects, the amount drawn may not exceed the lesser of 50 ml or 3 ml per kg in an 8 week period and collection may not occur more frequently than 2 times per week. (F)(3) Prospective collection of biological specimens for research purposes by noninvasive means. Examples: (a) hair and nail clippings in a nondisfiguring manner; (b) deciduous teeth at time of exfoliation or if routine patient care indicates a need for extraction; (c) permanent teeth if routine patient care indicates a need for extraction; (d) excreta and external secretions (including sweat); (e) uncannulated saliva collected either in an unstimulated fashion or stimulated by chewing gumbase or wax or by applying a dilute citric solution to the tongue; (f) placenta removed at delivery; (g) amniotic fluid obtained at the time of rupture of the membrane prior to or during labor; (h) supra- and subgingival dental plaque and calculus, provided the collection procedure is not more invasive than routine prophylactic scaling of the teeth and the process is accomplished in accordance with accepted prophylactic techniques; (i) mucosal and skin cells collected by buccal scraping or swab, skin swab, or mouth washings; (j) sputum collected after saline mist nebulization. (F)(4) Collection of data through noninvasive procedures (not involving general anesthesia or sedation) routinely employed in clinical practice, excluding procedures involving x-rays or microwaves. Where medical devices are employed, they must be cleared/approved for marketing. (Studies intended to evaluate the safety and effectiveness of the medical device are not generally eligible for expedited review, including studies of cleared medical devices for new indications.) Examples: (a) physical sensors that are applied either to the surface of the body or at a distance and do not involve input of significant amounts of energy into the subject or an invasion of the subject's privacy; (b) weighing or testing sensory acuity; (c) magnetic resonance imaging; (d) electrocardiography, electroencephalography, thermography, detection of naturally occurring radioactivity, electroretinography, ultrasound, diagnostic infrared imaging, doppler blood flow, and echocardiography; (e) moderate exercise, muscular strength testing, body composition assessment, and flexibility testing where appropriate given the age, weight, and health of the individual. (F)(5) Research involving materials (data, documents, records, or specimens) that have been collected, or will be collected solely for nonresearch purposes (such as medical treatment or diagnosis). (NOTE: Some research in this category may be exempt from the HHS regulations for the protection of human subjects: 45 CFR 46.101(b)(4). This listing refers only to research that is not exempt.) (F)(6) Collection of data from voice, video, digital, or image recordings made for research purposes. (F)(7) Research on individual or group characteristics or behavior (including, but not limited to, research on perception, cognition, motivation, identity, language, communication, cultural beliefs or practices, and social behavior) or research employing survey, interview, oral history, focus group, program evaluation, human factors evaluation, or quality assurance methodologies. (NOTE: Some research in this category may be exempt from the HHS regulations for the protection of human subjects: 45 CFR 46.101(b)(2) except for children when the Investigators participate in the activities and (b)(3). This listing refers only to research that is not exempt.) (F)(8) Continuing review of research previously approved by the convened IRB as follows: (a) Where (i) the research is permanently closed to the enrollment of new subjects; (ii) all subjects have completed all research-related interventions; and (iii) the research remains active only for long-term follow-up of subjects; or (b) where no subjects have been enrolled and no additional risks have been identified; or (c) where the remaining research activities are limited to data analysis. (F)(9) Continuing review of research, not conducted under an investigational new drug application or investigational device exemption where categories two (2) through eight (8) do not apply but the IRB has determined and documented at a convened meeting that the research involves no greater than minimal risk and no additional risks have been identified. Note: An expedited review procedure consists of a review of research involving human subjects by the IRB chairperson or by one or more experienced reviewers designated by the chairperson from among members of the IRB in accordance with the requirements set forth in 45 CFR 46.110. Note: Children are defined in the HHS regulations as "persons who have not attained the legal age for consent to treatments or procedures involved in the research, under the applicable law of the jurisdiction in which the research will be conducted." 45 CFR 46.402(a). Data and Safety Minimizing Risks to Participants/Data and Safety Monitoring Plan (DSMP) Federal regulations clearly state that risks to research subjects posed by participation in research should be justified by the anticipated benefits to the subjects or society. It is the PI’s responsibility to describe plans for minimizing risks to the research participant in this study. It is important for the Investigator to have a written plan of how he/she will monitor the collection of research data and the safety of research participants. This includes how the PI plans to assure that he/she meets his/her responsibilities when functioning as the coordinating center for a multi-center trial. This information is important to the IRB so it can determine that the administrative operations of the Coordinating Center has sufficient mechanisms in place to assure that: each collaborating institution holds an OHRP-approved assurance (FWA); each protocol is reviewed and approved by an OHRP-registered IRB at the collaborating institution prior to the initiation of research; informed consent is obtained from each participant in compliance with policy and regulations, if applicable; adequate plans are provided for evaluating, processing and reporting adverse events occurring at non-VU sites; and adequate plans are provided for assuring participant confidentiality. If the VU site and the PI are serving as a Coordinating Center for multi-center studies, the questions on the IRB application should be answered, describing the PI’s responsibilities as a performance site and as a coordinating center. Minimization of Risks Health Science: Provide a summary of how the risks to the participant will be minimized. Examples of minimizing risks include the following: review of study design/procedures by internal committees (GCRC, SRC, HSRC, RDRC, IBC), and external committees (ECOG, NIH, DSMB, other cooperative groups, expert consultants, etc.); limiting inclusion criteria to those who could most likely benefit, appropriately excluding those who are at greater potential for harm; additional safeguards to protect vulnerable populations; planned interim safety analyses; ongoing monitoring of the appropriateness of the research design; providing oversight by key personnel who are qualified to conduct study activities; organizing a DSMB to oversee the study progress and adverse events; a safety reporting plan; protecting participant privacy and confidentiality by coding data and specimens; and interventions which may serve both standard of care and research purposes. Behavioral Science: Provide a summary of how the risks to the participant will be minimized. Examples of minimizing risks include the following: review of study design/procedures by internal/departmental committees (e.g., faculty advisor, dissertation committee, etc.), and external committees (NIH, DSMB, other cooperative groups, expert consultants, etc.); limiting inclusion criteria to those who could most likely benefit, having a researcher present during experimental manipulations and/or data collection, appropriately excluding those who are at greater potential for harm; additional safeguards to protect vulnerable populations; planned interim safety analyses; ongoing monitoring of the appropriateness of the research design; providing oversight by key personnel who are qualified to conduct study activities; organizing a DSMB to oversee the study progress and adverse events; a safety reporting plan; protecting participant privacy and confidentiality by coding data and specimens; and interventions which may serve both standard of care and research purposes. If there is a chance you will identify any serious threats to participant safety (e.g., depression, suicidal threats, anxiety that does not quickly subside) describe how you will respond to these threats in order to minimize participant risk. Risk/Benefit Ratio Provide a description of the risks and benefits to participants and indicate how they are justified. This can include benefits to humankind as well as to the participants. Data Safety Monitor/Board Check the appropriate box to identify if an independent safety monitor or board/committee exists to review this study for safety and adherence to the study protocol. The monitoring may be conducted by an individual or a group of experts. There may be a committee with this responsibility that may function under another name, e.g. protocol monitoring committee. If “Yes” is indicated, include information about the composition of the committee, their qualifications, and their plans for monitoring the progress of trials and the safety of participants (e.g., timing of DSM reviews and reports planned interim analysis, etc.). DSMB reports are required to be submitted to the IRB immediately upon receipt. Data Safety Monitoring Plan Even if there is no DSM Board/Committee, there should always be a plan in place for monitoring data and ensuring the safety of participants. In this section, the PI should describe his/her data and safety monitoring plan and explain plans for assuring data accuracy and protocol compliance. When designing a DSMP, the Investigator should take into consideration the type(s) of risk(s) that the research involves. This DSMP should include an indication of whether a data safety monitor or a board/committee has been assigned as well as a general description of the DSMP. Progress Monitoring Describe plans for monitoring the progress of the research study and the safety of the participants. Describe the qualifications of the monitor/committee members. Define the process for approving and monitoring the research study. Identify the frequency of data safety monitoring reviews and reporting including planned interim analysis. Please note that DSM/B reports are required to be submitted to the IRB immediately upon receipt. Adverse Event/Unanticipated Problem Reporting Health Science: Describe plans for assuring compliance with requirements regarding reporting of adverse events or unanticipated problems involving risk to subjects or others. Include plans for reporting adverse events or unanticipated problems to subjects or others to the IRB and to the appropriate regulatory agencies. Behavioral Science: Compliance with Adverse Event and Suspension Reporting. This is a certification by the PI that all requirements regarding reporting adverse events (AEs) and suspensions will be followed. In accordance with federal regulations and VU policy (see IRB Policy III.L) adverse events and unanticipated problems involving risk to participants or others that fall under VU IRB jurisdiction must be reported within 10 working days after learning of the event or problem. Reporting of Suspensions Health Science: Describe plans for assuring that any action resulting in a temporary or permanent suspension is reported to the IRB and to the appropriate regulatory agencies. Also, describe plans for assuring any temporary or permanent suspension of a funded clinical trial is reported to the grant program director responsible for the grant. Behavioral Science: For funded research projects, any action resulting in a temporary or permanent suspension must be reported to the program director responsible for the grant. Data Accuracy and Protocol Compliance Describe plans for assuring data accuracy and protocol compliance. Coordinating Center Functions Complete this section when the PI functions as the coordinating center AND as a recruitment site. If Vanderbilt PI will function strictly as a Coordinating Center for a multi-center trial, please complete the Coordinating Center application. Sample consent form development or distribution will be part of the coordinating center responsibilities, describe the coordinating center’s role in reviewing modifications by the collaborating institution of sample consent information related to risks or alternative procedures to assure changes are appropriately justified (a copy of the sample consent form intended for distribution should be submitted with this application). Critical documents (study) management - CC’s may assume responsibility from the sponsor for tracking IRB approvals at each participating site, assuring IRB approval is granted prior to enrollment of participant at a participating center, and assuring no participants are enrolled prior to written IRB approval or during a lapse in approval (see the ICH guidelines section 8.2 for a listing of critical documents required before the trial commences and at the end of the trial and where the files are typically located). Site Selection and Training in Study Procedures - include how sites are selected (e.g., PI and key study personnel qualifications, experience, adequate resources and facilities). Assuring informed consent is obtained - If “Yes,” describe the mechanisms to be employed, if “N/A,” explain who is responsible for assuring informed consent is obtained. Studies involving different Phases Indicate the phase(s) of the study to be coordinated under this application. Clinical Trials Have plans been developed to register the trial with Clinicaltrials.gov? The NCT number should be entered on the Info tab of the study main page after the NCT number has been assigned by the ClinicalTrials.gov registry. There are currently 4 mandates for registration of clinical trials: FDA, NIH, CMS and ICMJE. Congress requires the registration of clinical trials at the ClinicalTrials.gov. under the FDA Amendment Acts of 2007 as described by NIH policy. Additionally, this is required by the Center for Medicare and Medicaid Services NCD of July 9, 2007. If you already have ClinicalTrials.gov accounts log into the Protocol Registration System (PRS) for the latest information on the changes currently in progress. If it is the responsibility of an industry sponsor to register the trial, you should still ensure it has been properly registered prior to enrolling participants. What are the “applicable clinical trials” that must be registered? 1. Trials of Drugs and Biologics: clinical investigations, other than a phase I investigations, of a product subject to FDA regulation 2. Trials of Devices: (a) a prospective clinical study of health outcomes of devices subject to FDA, other than small feasibility studies (b) a pediatric postmarket surveillance Note to PI: The members of the International Committee of Medical Journal Editors (ICMJE) will consider a trial for publication only if it has been registered publicly before enrollment of the first patient. http://www.icmje.org/clin_trialup.htm Who is responsible for Registration? The “Responsible Party” is defined as: 1. Commercial Sponsor of the clinical trial 2. Principal investigator (a) If so designated by a sponsor, grantee, contractor, or awardee so long as the PI is responsible for conducting the trial and has sufficient data rights (access to and control over the data from the clinical trial, the right to publish the results of the trial, and the ability to meet all of the requirements for submitting information under the law). (b) If you are the Investigational New Drug Application (IND) or Investigational Device Exemption (IDE) holder, you may be the “sponsor” as that term is defined in the FDA regulations (21 CFR 50.3). (c) If you are a Principal Investigator who has been delegated registration duties by the sponsor. (d) If you are the funding recipient you may be considered the “responsible party” as defined in the Act. For extramural trials, NIH is not the responsible party. NOTE to PI: It is your responsibility to ensure that your registration meets the requirements of applicable laws and regulations. Acceptance by ClinicalTrials.gov in the Protocol Registration System (PRS) and assignment of a National Clinical Trial (NCT) number to a registration record does not ensure compliance with applicable laws. Contact Research Support Services if you have questions regarding the law or need assistance registering a trial at (615) 322-7344 or Research.Support.Services@vanderbilt.edu. Additional information on the new registration requirements is available on the PRS Web site http://prsinfo.clinicaltrials.gov/. Subject Population(s) Maximum number of participants that are planned to be consented by this PI (including any withdrawals by participant, PI or sponsor OR consented screen failures) Provide the maximum number of anticipated participants at Vanderbilt and non-Vanderbilt sites who will be enrolled by this PI. Of the maximum number anticipated to be consented by this PI, how many of these are expected to complete the study or will participate in the study beyond screening? Total number of participants stated in the protocol to be studied at all sites (regardless of PI) Provide the total number of anticipated participants stated in the protocol to be studied at all sites, regardless of the PI. This applies even if Vanderbilt is not the coordinating center/lead institution. If this is a multi-center trial and you are the PI of the study at Vanderbilt as a participating performance site but not the coordinating center, please include the total overall number of participants for the entire multi-center trial including Vanderbilt and non-Vanderbilt sites. This does not apply to all studies. Targeting One Gender or Social/Ethnic Group It is important for the IRB to understand if and why your research is targeting only one gender and/or one social/ethnic group. The IRB must follow specific guidance when reviewing proposed research of this nature. For further information, see the following website: Inclusion of Women and Minorities in Research http://www.hhs.gov/ohrp/irb/irb_chapter6.htm (Federal regulations require the equitable selection of minorities as research subjects to ensure that they receive an equal share of the benefits of research and to ensure that they do not bear a disproportionate burden.) Risk for Incarceration HHS regulations at 45 CFR part 46, subpart C provide additional protections pertaining to biomedical and behavioral research involving prisoners as subjects. These regulations apply to research studies that target prisoners but also to research studies where it is not anticipated and an enrolled participant inadvertently becomes a prisoner at any time during the study. If a research participant becomes a prisoner after enrolled in a research study, the Investigator should report this to the IRB immediately. All research interactions and interventions with, and obtaining identifiable private information about, the now-incarcerated prisoner-subject must cease until the requirements of subpart C have been satisfied with respect to the relevant protocol. If the Investigator asserts that it is in the best interests of the subject to remain in the research study while incarcerated, the IRB Chairperson may determine that the subject may continue to participate in the research until the requirements of subpart C are satisfied. The Investigator must comply with the IRB Chairperson’s determination. If participants become prisoners when they are enrolled in a research study, state whether the Investigator will withdraw the prisoner-subject from the study. If not, describe how recontacting, reconsenting, treatment, and/or follow-up will occur. It is important to identify who your research subjects will be The IRB must follow specific guidance and regulations for certain populations. Place a check beside all of the categories of potential subjects that apply to the proposed research. If Veterans are your targeted population, R&D Committee approval will also be required. In addition, the appropriate IRB supplemental form should be completed as indicated on the application. The IRB Supplemental Forms may be accessed via the VU IRB website at http://www.mc.vanderbilt.edu/irb/forms. For additional information regarding the inclusion of pregnant women, fetuses, prisoners, children, and cognitively impaired individuals, as participants, you may refer to the following websites: Inclusion of Children in Research http://www.hhs.gov/ohrp/humansubjects/guidance/45cfr46.htm#subpartd Inclusion of Women and Minorities in Research http://www.hhs.gov/ohrp/humansubjects/guidance/45cfr46.htm#subpartb Prisoner Research http://www.hhs.gov/ohrp/humansubjects/guidance/prisoner.htm IRB Guidebook, Chapter VI – Special Classes of Subjects http://www.hhs.gov/ohrp/irb/irb_chapter6.htm Children Place a mark in the box beside the category that best represents the proposed research. Carefully read all the information under each category and answer all questions. Note: Minimal risk means that the probability and magnitude of the harm or discomfort anticipated in the research are not greater in and of themselves than those ordinarily encountered in daily life of a healthy child or during the performance of routine physical exams or tests. CATEGORY 1 (45 CFR 46.404; 21 CFR 50.51) This proposed research poses no greater than minimal risk to children. Explain why the research falls under this category and describe the provisions for soliciting the assent of the children and the permission of at least one parent/guardian. Describe the methods which will be used for evaluating dissent. Note: When research is covered by §46.405, informed consent should be sought from both parents unless one parent is deceased, unknown, incompetent, or not reasonably available, or when only one parent has legal responsibility for the care and custody of the child. Under this category, only consent from one parent is required to allow individual to participate. CATEGORY 2 (45 CFR 46.405; 21 CFR 50.52) This proposed research poses greater than minimal risk to children and includes an intervention or procedure that DOES hold out the prospect of a direct benefit for the individual child or a monitoring procedure that is likely to contribute to the child’s well-being. Explain why the research falls under this category; why the relation of the anticipated benefit to the risk is at least as favorable to the subjects as that presented by available alternative approaches; and how adequate provisions are made for soliciting the assent of the children and the permission of at least one parent/guardian. Note: When the research meets either category § 46.406 or § 46.407, informed consent must be obtained from both parents unless one parent is deceased, unknown, incompetent, not reasonably available, or when only one parent has legal responsibility for the care and custody of the child. CATEGORY 3 (45 CFR 46.406; 21 CFR 50.53) This proposed research poses greater than minimal risk to children and is presented by an intervention or procedure that DOES NOT hold out the prospect of direct benefit for the individual subject, or by a monitoring procedure which is not likely to contribute to the well-being of the child, BUT is likely to yield generalizable knowledge about the subject’s disorder or condition. Explain why the research falls under this category; state how the risks are more than minimal and explain why the additional risk is reasonable but not more than they would experience or expect considering their disorder or condition. Consider the magnitude of the potential harm and the likelihood of it occurring, CATEGORY 4 (45 CFR 46.407; 21 CFR 50.54) This proposed research does not meet the requirements of Category 1, 2, or 3 listed above. Research under Category 4 must include consultation with the Secretary of Health and Human Services if the research is funded or conducted by the Department of Health and Human Services. The IRB must submit the study to the Office of Human Research Protections (OHRP) for review and approval prior to the initiation of any research-related procedures. The Secretary will then consult with appropriate experts, followed by publication in the Federal Register of the intent to approve such research. Once approval is granted, the IRB may then approve the research. Explain why the proposed research presents a reasonable opportunity to further the understanding, prevention, or alleviation of a serious problem affecting the health or welfare of children. Cognitively Impaired – Comatose/Traumatized Explain why it is necessary to involve this population Provide a detailed rationale for why it is necessary to include this population as participants in research. This rationale should include information regarding the potential benefit to this population in relationship to potential risks. If research involves institutionalized individuals Provide a justification for the use of institutionalized individuals, if applicable. Describe why noninstitutionalized individuals could not be substituted. If research pertains to aspects of institutionalization If applicable, provide a description of the research as it pertains to institutionalization. This description should include if the research plan involves the manipulation of the institutionalized individuals routine schedule, rewards for participation, etc. Evaluating mental status Describe the procedures for evaluating the mental status of the prospective participant to determine whether they are capable of consenting. This would include the use of standardized measurements, consults with another qualified professional, etc. Loss of capacity to consent or withdraw Provide a description of how the participant will be protected in the event they lose their capacity to consent or their capacity to withdraw. This may include the use of an ombudsman, frequent cognitive status evaluations, etc. Another person authorized to consent Describe how persons authorized to obtain legally valid consent will be identified in the event any individual is judged incapable of consenting on their own behalf. This could include the use of a durable power of attorney for healthcare, a legally appointed guardian (this must be a court-appointed individual), or the use of surrogate consent as outlined and approved in IRB policy IV.A. Consultation of health care provider Describe when and how the participant’s health care provider will be consulted prior to participation in the research. This may include notification when changing routine care practices, coordination of care, etc. Interference with ongoing therapy or regimens Describe if this research will likely interfere in ongoing therapy or regimens of the participant. This should include if the participant will be removed from routine drugs/treatments, wash out periods, etc. Pregnant Women, Fetuses, Neonates Place a check next to the category that best describes your proposed research and answer all questions related to that category. § 46.204 Research Involving Women or Fetuses. 1. 2. 3. 4. 5. Explain why the research is scientifically appropriate. Describe any animal studies and previous human studies that have been conducted on pregnant animals /humans or non-pregnant animals/humans to support the research. Describe the potential risks to pregnant women and fetuses. Select the box that best describes your research regarding the risk/benefits to the study population. Describe the potential benefits to the women/fetus if any. If the research involves no benefit to the participants and involves no more than minimal risk, please provide information to support the minimal risk determination and how the study may provide important biomedical knowledge that cannot otherwise be obtained. Explain how the risks to subjects will be minimized; and are the least possible to achieve the objectives of the research. Please complete items a, b and c. Please note, to meet the requirements for IRB approval each of the responses must be “no”. If any of the responses are “yes”, please contact the IRB for assistance. In summary: a. Inducements, either monetary or otherwise, cannot be offered to terminate a pregnancy. b. No individual who will be engaged in the research (performing research procedures, including recruitment and obtaining consent) can be involved in any decisions as to the timing, method, or procedures used to terminate a pregnancy. c. No individual who is engaged in the research can have any part in determining the viability of a fetus. Indicate the procedures for obtaining informed consent by completing section/s a - d as appropriate. If a waiver or alteration of informed consent or a waiver of the documentation of informed consent is being requested, please also complete the Request for waiver form 1112. In determining whether one or both parents are required to provide consent, consider the individuals who will potentially benefit from the research. If there is benefit for the pregnant women and fetus; or if there is no benefit to either, and the research is minimal risk, only the mother is required to provide consent. However, if the benefit is solely to the fetus, consent must be obtained from both parents (unless the father is unable to consent because of unavailability (inconvenience does not qualify), incompetence, or temporary incapacity or the pregnancy resulted from rape or incest. For research involving pregnant minors, assent is also required from the pregnant child. In accordance with the Federal regulations, children are persons who have not attained the legal age to consent to treatments or procedures involved in the research, under the applicable law of jurisdiction in which the research will be conducted. In Tennessee, the legal age for consent is 18 years of age.) Please complete the Vulnerable Population Form for Children (Form 1117). Please note, under certain circumstances, mature or emancipated minors may be considered as individuals who can provide consent. Please see IRB Policy IV.A Informed Consent Process for further guidance. § 46.205 Research Involving Neonates A neonate cannot be involved in research until it has been ascertained as viable or not viable. Viable Neonates A neonate after delivery that has been determined to be viable may be included in research if all of the requirements of Subparts A and D of 45 CFR 46 are met. Describe the procedures used for obtaining informed consent. Indicate if a legally authorized representative will be used or if the consent process will require signatures from both parents. Note: Please check the box for Children and complete the questions regarding that population in addition to the section for viable neonates. Neonates of Uncertain Viability and Nonviable Neonates Give a description of why this research is scientifically appropriate. Describe any animal studies and previous human studies that were conducted that can provide data for assessing potential risks to neonates. Indicate if any individuals engaged in research will have any part in assessing viability. Please note, if the answer is yes neonates of uncertain viability and nonviable neonates may NOT be included in the research. Neonates of Uncertain Viability Please indicate either the research holds out the prospect of enhancing survival to the point of viability and how the risks are the least possible; OR whether the information cannot be obtained by any other method and there will be no added risk to the neonate. Describe the procedures used for obtaining informed consent. Indicate if a legally authorized representative will be used or if the consent process will require signatures from both parents. Nonviable Neonates (additional requirements for their inclusion in research) Indicate if the vital functions of the neonate will be artificially maintained and describe the procedure for maintaining vital functions. Indicate if the research includes procedures to terminate the heartbeat or respiration of the neonate. Describe any added risks that may result to the neonate from this research. Indicate whether the sole purpose of the research is for the development of important biomedical knowledge and whether the knowledge can be obtained by any other means. § 46.206 Research Involving, After Delivery, the Placenta, the Dead Fetus, or Fetal Material. Indicate by checking the boxes of all that apply to the proposed research. The use of any of the listed must be conducted in accordance with any applicable Federal, State, and local laws, regulations, and institutional policies regarding such activities (See IRB Policy IX.C for further details). Indicate if any information associated with the material could be recorded for research purposes in such a manner that living individuals can be identified. Describe the rationale for the recording of identifiable information. If the information is identifiable, those individuals are considered to be research subjects and all pertinent human subject regulations are applicable to their participation. § 46.207 Research Not Otherwise Approvable Which Presents an Opportunity to Understand, Prevent, or Alleviate a Serious Problem Affecting the Health or Welfare of Pregnant Women, Human Fetuses, or Neonates. This requires review by the Secretary of the Department of Health and Human Services (DHHS) and posting in the Federal Register for public comments and review. Provide information to justify how the research presents an opportunity to further understand, prevent or alleviate a serious problem affecting the health or welfare of pregnant women, fetuses or neonates. 1. 2. Describe how the research will be conducted in accord with sound ethical principles; and Explain how informed consent will be obtained. Prisoners Definitions: Minimal risk is the probability and magnitude of physical or psychological harm that is normally encountered in the daily lives, or in the routine medical, dental, or psychological examination of healthy persons. Prisoner means any individual involuntarily confined or detained in a penal institution. The term is intended to encompass: Individuals sentenced to such an institution under a criminal or civil statute; Individuals detained in other facilities by virtue of statutes or commitment procedures which provide alternatives to criminal prosecution or incarceration in a penal institution; or Individuals detained pending arraignment, trial, or sentencing. Note: Probation and parole are usually NOT considered as incarceration. Place a check in the box beside the category that best represents the research. Carefully read all the information under each category and select the box that best represents the research. Explicitly state the rationale for the selection including any supportive information/documentation. On June 20, 2003, the HHS Secretary allowed a waiver for certain research conducted or supported by HHS functions for research which has as its sole purpose (i) to describe the prevalence or incidence of a disease by identifying all cases, or (ii) to study potential risk factor associations for a disease. The range of studies to which the waiver applies includes epidemiological research related to chronic diseases, injuries, and environmental health. The research may use epidemiologic methods such as interviews and collection of biologic specimens that generally entail no more than minimal risk to the subjects. All of the other requirements of Subpart C apply to research in this category. NOTE: research on conditions particularly affecting prisoners as a class and research practices, both innovative and accepted, which have the intent and reasonable probability of improving the health or well-being of the subject must include consultation with the Secretary of Health and Human Services. The Secretary must consult with appropriate experts, including experts in penology, medicine, and ethics followed by publication in the Federal Register of the intent to approve such research. Once approval is granted the IRB may then approve such research. How does each of the following required conditions apply to the research? Please address each required condition by indicating “No” or “Yes”. Include the rationale for your selection in order to assist the Committee in reviewing the research and determining risk to this vulnerable population. Recruitment Participant Identification Provide a detailed description of how potential participants will be identified and contacted. When disclosure of a patient or students name or diagnosis to you would violate that person’s confidentiality rights, you may need to use a two-stage process in which clinic or school personnel (who know the patient or student) inform the individual of your study and obtain a consent to allow you to contact that individual. NOTE: If you are using private, identifiable information such as medical records or student records, there may be other VU offices that will need to approve the use of such information (e.g., Medical Records, Informatics Security Office, University Registrar, etc.) Inclusion/Exclusion Criteria Provide a detailed description of all requirements that must be met in order for potential participants to qualify for study participation and the procedures used to determine eligibility. To be specific, you may need to describe how data that will be used to determine eligibility will be obtained. For example, if psychiatric diagnosis is an exclusion criterion, how will you determine (e.g., interview, questionnaire, medical record review) whether or not each potential participant qualifies? NOTE: An amendment must be submitted to the IRB for review/approval before executing any deviations, exceptions, or changes from the IRBapproved criteria. Participant Selection Provide a description of how the selection of participants will remain equitable in relation to the research purpose and setting. This can include a statement that no one ethnic group or gender will be targeted. For example, the study will attempt to recruit an equal number of female and male participants. In addition, describe the composition of anticipated participants such as teachers vs. students vs. parents or healthy volunteers vs. patients. Advertisements Identify if you plan to use any sort of advertisement for recruitment purposes. If “yes”, identify the method(s) of advertisement that will be used (internet, letters, radio, newspaper ads, telephone, television, flyers, posters, mass e-mails). NOTE: A copy of all advertising materials including ads, letters and telephone scripts, must be submitted with this application. If graphics will be used, they must be included on what is submitted for review and approval. The IRB must review/approve final copies of all audio/videotapes prior to use. NOTE: Any advertisements to be submitted for mass e-mail solicitation can be requested directly from the Executive Director of Medical Center Communications if you have a stamped IRB approval on your ad. Compensation Specify the method of compensation, if any, and describe how it will occur in the course of the study. Vanderbilt-Approved List Services, Web Sites, or Publications Vanderbilt University has a variety of list services and publications, such as the Clinical Trials Website. Posting research protocol information on research-related websites and other listing services, allows potential participants to search and find studies related to their condition or interest. Prior to any information being forwarded for posting on such websites, it is the responsibility of the Principal Investigator to be aware that if a research study is being conducted subject to a contractual agreement, it may be necessary to obtain written permission from the sponsor prior to authorizing the release of any study information for these purposes. Identify whether or not you would like for information regarding this study to be released and posted on Vanderbilt-approved list services, websites, or publications. If yes, the IRB approved Consent Form, Item #1, Purpose of the study, language may be used as the lay description for the study. Radiation Procedures and Radioactive Drugs Please indicate where at VU/Department administering the X-ray or radionuclide procedures: It is important for the VU HSRC to obtain information regarding the location(s) where radiological procedures for research will be conducted. This ensures that appropriately trained radiological personnel are performing the procedures/administering radiolnuclides and that the appropriate individuals from the department have been involved in the development of research-related procedures. Will this study include any external beam (X-ray) procedures for research purposes? Use the table to list the individual radiological procedures being performed for research purposes, the number of procedures performed per subject during the first year, and the total number of procedures performed for research purposes over the course of the study. If a procedure is not listed in the dropdown menu you may free type the name of the procedure in the table. For fluoroscopy, type in the body location and “on time” for the procedure. The table entry will be highlighted in red for free text entries. Does this study involve the administration of radioactive materials? If your study involves a MUGA or whole body bone scan for research this question should be marked “Yes”. Use the table to list radioactive materials administered for research purposes. For MUGA, select Tc-99m Red Blood Cells. For whole body bone scan select Tc-99m MDP. Radioactive Materials for Imaging, Treatment, or Diagnosis Study Procedures Only procedures that are being performed for research purposes should be included. For each procedure, please note the total number of procedures that will be performed per subject for the first year and the total number of procedures to be performed per subject over the course of the study. Radioactive Materials for Basic Knowledge, Metabolism, and Distribution Outline of related work and pre-clinical studies Identify related published materials and/or results from pre-clinical studies that support the use of this radiological procedure for the purposes of this study. Outline of plan of investigation, including analytical procedures used for radioactivity measurements Specifically outline the plan of investigation and procedures used to measure radioactivity throughout the course of the study. A clear plan is essential for the protection of participants receiving research related radiation exposure. For each radioactive drug utilized in this study, the following should be identified: radionuclide and drug administered; justification for radiation exposure; route of administration; activity (mCi or MBq) per administration/subject/year (provide typical value and dose range); maximum possible number of administrations/subject/year; source of radiation dose information; references from the scientific literature (reprints must be enclosed). Estimated time needed to complete study Identify the estimated time needed to reach study goals and complete study participation. Pharmacologically active ingredients of the drug Provide a list of each chemically active agent contained in the radiological drug. Total amount of drug to be administered Provide the total amount of drug (labeled plus unlabeled) to be administered to participants. Dose ranges should be provided in mass or volume units rather than radioactivity units. Quality of Radioactive Drug Please name the identity, strength, quality and purity of the radioactive drug and specify how appropriate pharmaceutical and radiochemical standards will be met. Note: Materials for parental use must be sterile and pyrogenfree. Does the drug produce a clinically detectable pharmacological effect? Provide pharmacological dose calculation or data if applicable. Additional Information Regarding HSRC/HDRC Studies Consent Language The HSRC/RDRC must approve the wording utilized in the Informed Consent Document (ICD). The Dosimetrist will provide appropriate language based on the procedures being done for research. A copy of the ICD should be included in the HSRC submission and should identify the exact risk language for radiological procedures. Billing for research procedures For studies that include radiological procedures for research purposes, a consult with the senior billing manager from radiology is required to ensure that payment for the procedures are charged appropriately. This individual will also help identify the responsible party representing the department that will be administering the radionuclide exams or x-ray procedures. The Senior Billing Manager can be contacted at 3-2779. To qualify for RDRC review, protocols must meet the following criteria: 1. 2. 3. 4. 5. 6. 7. The use of a Radioactive Material (RAM) for Research Purposes; Administering Physician must be approved by the Radiation Safety Committee (RSC); RAM must not have an IND, NDA, PLA; Purpose of the study must be for basic information, including kinetics, distribution and localization, or regarding physiology, pathophysiology, or biochemistry; Procedures can not be intended for therapeutic or other clinical benefit; Single doses must be less than 3 rem to the whole body, eyes, blood forming organs, or gonads OR less that 5 rem to other organs; Annual dose must be less than 5 rem to whole body, eyes, blood forming organs, or gonads OR less than 15 rem to other organs; AND 8. Active radioactively labeled ingredients must not be known to cause clinically detectable pharmacology effect in amounts to be administered. All RDRC protocols are reviewed at a convened meeting of the full committee as identified in 21 CFR 361.1. Also in accordance with these regulations, all approved RDRC protocols are reviewed quarterly at a convened meeting of the full committee for updated study information. Protocol Analysts from the RDRC Office will contact each PI on a quarterly basis to obtain the necessary study information for Committee review. In addition, yearly reports are reviewed and forwarded to the Food and Drug Administration (FDA) for annual reporting of the active approved protocols. PIs will be contacted by RDRC staff and, for all active studies, will be required to complete FDA form 2915 and submit to the RDRC office for federal reporting requirements. Drugs, Devices, Biologics Drug(s)/Biologic(s), or placebo, Used for Research that HAVE an IND In the table, indicate all requested information. The information in the table should be simplified in each section. The Committee will refer to the study protocol for more detailed information regarding the study drug. Note, please indicate whether the investigational pharmacy will dispense the drug/biologic(s). Drug(s)/Biologic(s), or placebo, Used for Research that DO NOT an IND [only include drugs that are being used outside of package insert labeling for indication, route of administration, dose, dosing frequency, dosage form, and/or population in which the drug is being used (i.e. children)]. The investigator will be required to complete questions relative to an IND exemption for drugs listed in this section. With regard to IND exemption criteria, clinical investigations of a drug, agent, or biologic that is lawfully marketed in the United States are exempt from the requirements of an IND, if all of the following conditions are met: 1. Use of the investigational drug, agent, or biologic is not intended to be reported to the FDA in support of a new indication for use nor support any significant change in labeling for the product; 2. The use of the investigational drug, agent, or biologic is not intended to support a significant change in the advertising of the product; 3. The use of the product does not involve a route of administration, dosage level, and/or use in a subpopulation, or other factors that significantly increase the risks, or decrease the acceptability of the risks associated with the use of the drug, agent, or biologic; 4. The use will be conducted in compliance with the IRB approval and informed consent procedures; 5. The use will be conducted in compliance with the requirements concerning the promotion and sale of the drug, agent, or biologic as described in FDA regulations 21 CFR Sec. 312.7; and 6. The use does not intend to invoke exception from informed consent requirements for emergency use. Note, please indicate whether the investigational pharmacy will dispense the drug/biologic(s). Gene Transfer, Live, Recombinant, and/or Attenuated Microorganisms for Vaccination or select Agents Note: If any answer in this section is checked yes, approval from the Institutional Biosafety Committee is required.) Device Research Indicate all requested information within table. If your device has a prior FDA determination such as 510(k), PMA, IDE, HDE/HUD, or is currently being used as approved, please provide documentation from the FDA regarding its approved use. If you have no FDA determination regarding your device, please indicate whether your device meets an IDE exemption category OR complete the last column in this table to indicate whether the device is considered SR or NSR by the Sponsor or Sponsor Investigator. Note, the IRB requests a description for each device listed immediately under the table. The IRB requests an explanation for each device determination of non-significant risk (in addition to any correspondence from the study sponsor and/or FDA to support this determination). The IRB also recommends contacting the MDRAPS office for assistance with you device if there is no prior FDA determination at 615-343-2430 or http://www.cttc.co/mdrap . Sham Product and/or Procedure In the event your research involves a sham product and/or procedure, please indicate “yes” to this question and provide a description of the shame product/procedure for the committee’s review. PHI/Consent Describe the Specific Steps for Obtaining Consent It is important for the Committee to understand the procedure that will be utilized when obtaining consent from a potential participant. Specifically: who will be obtaining consent; where that consent will take place (e.g., clinic, hospital, classroom, cafeteria, etc.); when (e.g., at initial visit, second semester, etc.); and any additional relevant information. Relationship with Participant Indicate if the Investigator or his/her staff has an existing relationship with the participant (e.g., spouse, child, other relative, friendship, co-worker, etc.). If yes, provide the IRB with information regarding the measures that will be taken to avoid undue influence or coercion. Surrogate Consent The use of surrogate consent in research must be reviewed and approved by the IRB. The rationale for use must fit the criteria as outlined by Federal, State, and local laws and policies. Consent of Non-English Speaking Participants Federal regulations require the equitable selection of minorities as research subjects to assure that they do not bear a disproportionate burden. Obtaining Consent Indicate how consent will be obtained from the participant. This may include the use of a translator, and the use of a short form as a summary in the participant’s language, or this may include an exact replica of the original English version of the consent document in the language of the participant. NOTE: The PI may wish to delay translation until IRB approval is granted of the English version informed consent document to avoid extra translation costs. Informed Consent & Non-English Speaking Participants http://www.hhs.gov/ohrp/humansubjects/guidance/ic-non-e.htm Translation Service Indicate the name of the individual or service that translated the informed consent document. Qualifications List the qualifications of the individual or the service that was used to translate the informed consent document. For example, include any credentials, certifications, education, native language fluency, etc. Waiver or alteration of the consent process or a waiver or alteration of the consent documentation Identify if the proposed research will require the use of any waiver or alteration of the consent process/documentation. Please refer to IRB Policy IV.C for further guidance. Please be aware, if a protocol is granted a “Waiver of Consent and/or Authorization” by the VU IRB, and the study involves the use of PHI, the PI is responsible for accounting of disclosures. Please contact the Vanderbilt Privacy Office at: http://www.mc.vanderbilt.edu/root/vumc.php?site=HIPAA, or call 936-3594. The following information must be obtained for any PHI disclosed: 1. 2. 3. 4. 5. The date of the disclosure; The name, title, and contact number of the VUMC workforce member making the disclosure; The name of the entity or person who received the protected patient information, and, if know, the address of such entity or person; A brief description of the protected patient information disclosed; and A brief statement of the purpose of the disclosure that reasonably describes the basis for the disclosure. This mandate is pursuant to 45 CFR 164.528, which states that an individual has the right to request and receive an accounting from the covered entity of all possible disclosures of his/her protected health information that was permitted without the individual's authorization. Request for Waiver of Documentation of Informed Consent The IRB may approve the waiver of the documentation of informed consent for some or all of the participants if the study meets one of the following conditions: The only record linking the participant to the study is the consent document. Describe how the procedures are minimal risk with the exception of the signed consent document. The participant must be asked if they would like to sign a consent document. The consent document must be approved by the IRB prior to approaching the potential participant. The research is minimal risk and involves only procedures that do not require written consent outside of research. Request for Alteration of the Informed Consent Process The IRB may approve a consent procedure that alters or omits some or all of the elements of informed consent, or may waive the requirements to obtain informed consent if the following conditions are met: A. Explain how the informed consent will be altered. B. Describe how the waiver or alteration of consent will involve no more than minimal risk and will not adversely affect the rights and welfare, including privacy, of the individual. C. Describe why the research could not be carried our without the alteration or waiver of informed consent process. D. Provide a plan for providing individuals with pertinent information as it becomes available after participation. Request for Waiver of *Authorization. Authorization only applies when protected health information (PHI) collected or maintained by Vanderbilt will be used, created or disclosed in the course of the research. The following conditions must be met to approve a waiver of authorization: A. Provide a description of why the research could not be conducted without access to PHI. B. Describe how the privacy risks are reasonable in relation to the anticipated benefits (if any) and the importance of the knowledge gained from the research. C. Provide a plan for protecting the identifiers from improper use and disclosure. D. Provide a plan for destruction of the identifiers at the earliest opportunity consistent with the research unless there is a justification for keeping the identifiers, such as being required by law. E. Provide verification that the PHI will not be reused or disclosed to any other person or entity unless required by law for authorized oversight of the research, or for other purposes or other research. Please refer to IRB Policy IV.C for further guidance. Please be aware, if a protocol is granted a “Waiver of Consent and/or Authorization” by the VU IRB, and the study involves the use of PHI, the PI is responsible for accounting of disclosures. Please contact the Vanderbilt Privacy Office at: http://www.mc.vanderbilt.edu/root/vumc.php?site=HIPAA, or call 936-3594. The following information must be obtained for any PHI disclosed: 6. 7. 8. 9. 10. The date of the disclosure; The name, title, and contact number of the VUMC workforce member making the disclosure; The name of the entity or person who received the protected patient information, and, if known, the address of such entity or person; A brief description of the protected patient information disclosed; and A brief statement of the purpose of the disclosure that reasonably describes the basis for the disclosure. This mandate is pursuant to 45 CFR 164.528, which states that an individual has the right to request and receive an accounting from the covered entity of all possible disclosures of his/her protected health information that was permitted without the individual's authorization. Protected Health Information (PHI) The Health Insurance Portability and Accountability Act (HIPAA) privacy rule establishes the conditions under which protected health information (PHI) may be accessed (used) for research purposes. Protected Health Information (PHI) is individually identifiable health information that is or has been collected or maintained by the covered entity in the course of healthcare services, and can be linked back to the individual participant. If PHI is accessed during the course of preparing this research study, the conditions of the “Statement of Affirmation” must be met. If Protected Health Information (PHI) is accessed as part of this study then certain conditions must be met. As the PI, you must ascertain that the following conditions are met before accessing any medical record information: 1. The use or disclosure of the PHI is sought solely for the purpose of this research protocol. 1. The PHI will not be removed from Vanderbilt University Medical Center. 2. The PHI is necessary for the purpose of this research study. Use or Disclosure of Protected Health Information The Health Insurance Portability and Accountability Act (HIPAA) privacy rule establishes the conditions under which protected health information (PHI) may be used or disclosed by a covered entity. Protected Health Information (PHI) is individually identifiable health information that is or has been collected or maintained in the course of healthcare services at VU that can be linked back to the individual participant. The complete OCR HIPAA guidance document may be found at: http://www.hhs.gov/ocr/hipaa/privacy.html. STATEMENT OF AFFIRMATION: The "Statement of Affirmation" is your acknowledgement that the use of the PHI is sought solely for the purpose of preparing the research protocol, that the PHI will not be removed from the covered entity, and that this information is necessary for the purpose of the research study. In order to state that the data is recorded in a manner considered to be de-identified, all 18 HIPAA identifiers must be removed. The identifiers are: 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. 16. 17. 18. Names; Any geographic subdivisions smaller than a State, including street address, city, county, precinct, zip code, and their equivalent geocodes, except for the initial three digits of a zip code; All elements of dates (except year) for dates directly related to an individual (e.g., date of birth, admission); Telephone numbers; Fax numbers; Electronic mail addresses; Social security numbers; Medical record numbers; Health plan beneficiary numbers; Account numbers; Certificate/license numbers; Vehicle identifiers and serial numbers, including license plate numbers; Device identifiers and serial numbers; Web Universal Resource Locators (URLs); Internet Protocol (IP) address numbers; Biometric identifiers, including finger and voiceprints; Full-face photographic images and any comparable images; and Any other unique identifying number, characteristic, or code. The limited data set is protected health information that excludes all above data elements with the exception of elements of dates, geographic information (not as specific as street address), and any other unique identifying element not explicitly excluded in the list above. Intra-Vanderbilt Data Use Agreement Indicate all individuals who will be requesting authorization to access the “limited data set”. This set of study related data excludes the following direct identifiers of the individual or of relative, employer, or household member of the individual: names, postal address information (other than town or city, state, and zip code), telephone numbers, fax numbers, electronic mail addresses, social security numbers, medical records numbers, health plan beneficiary numbers, account numbers, certificate/license number, vehicle identifiers and serial numbers (including license plate numbers), device identifiers and serial numbers, web universal resource locators (URLS), internet protocol (IP) address numbers, biometric identifiers (including finger and voiceprints), and full-face photographic images and any comparable images. Attach a copy of the agreement to this application, if applicable. If the limited data set is disclosed to individual or institutions outside of the covered entity, a data use agreement is required. The data use agreement template is located at: http://www.mc.vanderbilt.edu/irb/forms/Form1109_DataUseAgreement.doc. Please submit the agreement to the Office of Grants and Contracts Management. ** “Covered entity” is defined by the function in which an individual accesses, uses or discloses individually identifiable health information. This includes any health information generated for treatment purposes. If the information is generated for research purposes only (involving no standard of care treatment), the information is research health information and is not under the covered entity. See the “Statement of Designation as a Hybrid Entity under HIPAA” for more information. Conflict of Interest Disclosure Potential Conflict of Interest According the VU IRB Policy VI.C Investigator and Key Study Personnel Conflict of Interest, all Investigators and Additional Study Personnel must identify in the IRB application, whether they or any other person responsible for the design, conduct, or reporting of the research has an economic interest in, or acts as an officer or a director of any outside entity whose financial interests would reasonable appear to be affected by the research. Identify whether or not the Investigator or any Additional Study Personnel have a potential conflict of interest. If yes, complete item 23 B. by placing a check beside all of the five categories that best describe the potential conflict of interest. An Investigator is considered to have a financial conflict of interest if he/she, his/her spouse, domestic partner and dependent children own together any equity in a sponsor. Do not consider the combined ownership of all investigators. NOTE: Although approval may be granted by the IRB, the Investigator may not proceed with the research until the MCCOIC or the University Conflicts Committee has rendered a final determination. Signing Principal Investigator’s Assurance Statement Carefully read this entire statement prior to signing. If the Principal Investigator is a student, his/her advisor MUST read and sign the Faculty Advisor Assurance Statement. NOTE: A Division Chief or Department Chair, in addition to the Principal Investigator, must also sign the Assurance Statement. Faculty Advisor’s Assurance Statement The faculty advisor must be a member of the Vanderbilt University Faculty. The faculty member is considered the responsible party for legal and ethical performance of this research project. Carefully read this entire statement prior to signing. NOTE: A Department Chair, in addition to the Faculty Advisor, must also sign the Assurance Statement. Please note both assurance statements are located within DISCOVR-E. Other Committee Approval Additional VU Committee Approvals As stated in VU IRB Policy VII.E, there are times when it is necessary for other University Committees at VU review and provide approval or guidance for a specific study. See the chart below for guidance: General Clinical Research Center (GCRC) GCRC reviews and approves all protocols to be conducted in the VU Clinical Research Center. Submit the GCRC supplemental form to the IRB for concurrent review. See the GCRC website for more details: http://www.mc.vanderbilt.edu/gcrc/ Human Subjects Radiation Committee (HSRC) HSRC must review and approve all research involving radiation exposure (from x-rays or radionuclides) of human subjects for routine diagnostic or therapeutic procedures used in a supporting role and which the subject would otherwise not receive as part of their medical care. Approval must be received prior to submission to the IRB. See IRB website for more details: IRB Policy XII.B. Institutional Biosafety Committee (IBC) IBC approval is required for research involving any of the following: deliberate transfer of recombinant DNA or RNA, DNA or RNA derived from recombinant DNA live, recombinant, and/or attenuated microorganisms for the purposes of vaccination “select agents” as defined by the U.S. Patriot’s Act. http://www.cdc.gov/od/sap/docs/42cfr73.pdf page 14 IBC approval must be received prior to IRB final approval, for all of the above-mentioned categories. IBC approval is required for research involving the use of recombinant DNA or potentially infectious microorganisms, which are not intended for direct and deliberate transfer into human subjects. IBC approval is not required prior to IRB final approval in this type of use. See IBC website for more details: http://www.safety.vanderbilt.edu/. Scientific Review Committee (SRC) Formerly known as the CPRMC, this committee must review and approve all protocols that involve cancer research. Approval from the SRC does not have to be obtained prior to submission to the IRB. Radioactive Drug Research Committee (RDRC) RDRC is authorized by the U.S. Food and Drug Administration to approve research projects involving the use of certain “non-approved” radioactive drugs for pre-Phase I research. RDRC approval must be received prior to submission to the IRB. See IRB website for more details: IRB Policy XII.D. Help and Suggestions For further help with any of these items, please call the VU IRB at (615) 322-2918 and ask for a Regulatory Compliance Analyst with either a Behavioral Science or Health Science team. If you have SUGGESTIONS to offer regarding the Wizard Application, Instructions, or the IRB in general, you may do so at http://mcapps01.mc.vanderbilt.edu/IRB/WkshpReg.nsf/Suggestion%20Form?OpenForm. NOTE: When utilizing the IRB suggestion box, you may choose to have your comments remain anonymous by not completing the contact information section.